‘Unknowing’ and mental health system reform in Palestine
—
Abstract
In 2012, the Palestinian Ministry of Health and the World Health Organisation (WHO) started a three-year initiative with funding from the European Union to improve the mental health system in the West Bank of the occupied Palestinian territories. This is the second phase of an initiative to reform the institution-based mental health system by introducing a community-based approach rooted in scientific evidence. In one of its first project reports, the WHO (2006, 19) asserts that evidence shows ‘that community-based mental health services, together with modern treatment methods not only improve the quality of life for service users and their carers, but are also cost effective’.
We seek to trouble this line of argument by demonstrating that mental health system reform in the West Bank is not simply shaped by scientific evidence and international standards but rather by concrete political constellations, national and international development agendas, and local and global socioeconomic contexts. We further argue that these political and socioeconomic forces gain their influence not by being openly discussed in public fora, project reports, or scientific texts, but precisely because they are rendered invisible and turned into what Geissler (2013) calls ‘unknown knowns’. Like ‘public secrets’ (Taussig 1999), unknown knowns are open to experience but, for one reason or another, cannot be articulated in a particular societal arrangement. As active practices, unknown knowns create particular forms of knowledge while also serving specific political and economic interests by ‘making domination unspoken, silencing critique and resistance, and exacerbating power differentials’ (Geissler 2013, 15).
To bring the unknown knowns of mental health system reform processes in the West Bank to the fore, we draw on data obtained during a qualitative pilot study carried out in 2013. We mapped organizations currently providing mental health care, conducted interviews with their staff, and collected reports on mental health as well as pamphlets from nongovernmental organisations and health service providers in the West Bank. We first show how the unknowing of political power plays allows for a particular imagination of mental health system reforms in states emerging from armed conflict. We then contrast this with a genealogy of mental health system reforms in the West Bank that highlights the interplay between ‘evidence-based’ standards, political events, and unequal power relations between international and local institutional actors over time. And, finally, we present Palestinian mental health providers’ reflections on these complex processes, and how they imagine a more sustainable mental health system that, in turn, builds on unknowing the stigma surrounding mental health. Our goal in this Think Piece is to stimulate a discussion around what ‘unknowing’ does to mental health system development and care in different societal contexts.
Imagining mental health system reform in war and postwar contexts
Imaginaries of mental health system reform in regions recently emerging from armed conflict or under endemic and protracted violence build on an understanding that the mental health situation in such contexts is particularly grave (Kienzler 2008; Tol et al. 2011). For instance, a recently conducted systematic review indicates an average prevalence of 15.4 percent for PTSD (in thirty studies) and 17.3 percent (in twenty-six studies) for depression in conflict-affected populations (Tol et al. 2011). These rates are considerably higher than the average of 7.6 percent for any anxiety disorder and 5.3 percent for any mood disorder, which have been reported for general populations in the World Mental Health Survey (Demyttenaere 2004). Despite this recognition of the gravity of the mental health situation, scholars and interventionists largely agree that we know relatively little about the ways in which these elevated rates of mental disorders and psychosocial problems might be effectively treated (Collins et al. 2011). To fill this knowledge gap, they generally advocate for research and for prioritizing adequate and sustainable mental health policies and interventions (Meffert and Ekblad 2013). Increasingly, such calls for action also include demands to reform entire mental health systems in accordance with international evidence-based standards, based on the presumption that only through a systemic approach can appropriate mental health care and psychosocial support be provided to civilian populations (Patel et al. 2012).
Often these reforms start out amidst crisis, as emergency projects in which psychological first aid and a variety of psychosocial support practices are offered (Kienzler and Pedersen 2012). Rather than prescribing pharmaceutical relief, evidence-based guidelines indicate that individuals experiencing acute mental distress after exposure to trauma are best supported through the provision of ‘basic, nonintrusive pragmatic care with a focus on listening but not forcing to talk; assessing needs and ensuring that basic needs are met; encouraging but not forcing company from significant others; and protecting from further harm’ (Sphere Project 2004, 293).
Once the immediate crisis is over, psychiatric first aid and initial psychosocial support services operate as the basis for developing extended mental health services and psychosocial support programs (Abramowitz 2010; Kienzler 2012). In order to render them sustainable, they are coupled with projects that enhance government-driven policies, human resources and training, programming and services, research and programme monitoring, and finances (Patel et al. 2012). In some national contexts (such as Bosnia-Herzegovina, East-Timor, Kosovo, and the occupied Palestinian territories), support is not only provided to improve mental health and psychosocial services, but also as part of the thorough reform of national mental health systems. Such reforms are often claimed to follow international guidelines and evidence-based standards that demand the closure of large psychiatric institutions and the creation of new institutional structures that provide mental health care through more holistic approaches in the community (WHO 2009; Patel et al. 2012).
This progression – from the provision of short-term emergency support to the development of evidence-based sustainable mental health systems – is presumed to be both linear and logical, and is the dominant model utilized by international stakeholders to justify ongoing work in war-affected societies. However, the emphasis on the utilization of standardized guidelines and evidence-based approaches not only justifies reform processes, it also diverts attention from ways in which political constellations, socioeconomic contexts, and differently positioned actors influence institution building, work practices, and care. We argue that ‘unknowing’ these factors creates a space of make-believe that allows for the imagination of a scientifically driven agenda that is free from politics, economic opportunism, and material and social inequalities. To substantiate this argument, we turn the previous narrative inside out by focusing on sociopolitical and economic arrangements that shape mental health reform in a particular context, namely in the West Bank.
The political life of mental health system reform in the West Bank
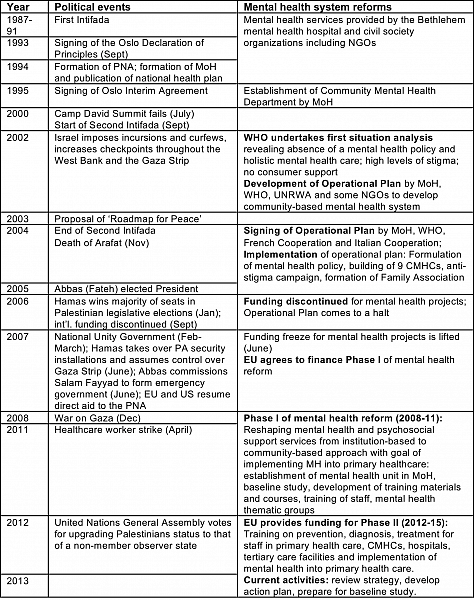
In the occupied Palestinian territories, recent political events have directly affected developments in national mental health system reform (see table 1). Concerted efforts to reform health care and mental health care began with the formation of the Palestinian National Authority following the signing of the Oslo Declaration of Principles in September 1993, and continued with the signing of the Oslo Interim Agreement two years later (Giacaman et al. 2009). Notably, these political events were crucial to the development of a national health system and the publication of a national health plan that included the establishment of the Community Mental Health Department in 1995 (see WHO 2006), the first since the beginning of the Israeli occupation in 1967.
However, until the Second Intifada (the second Palestinian uprising against Israel) in 2000, the Bethlehem Psychiatric Hospital and a few civil society organizations, including NGOs, mainly provided mental health services. According to a WHO (2006, 15) report, ‘Psychiatric hospitals in Bethlehem and Gaza were still the main assets to mental health care, while community mental health provision was extremely patchy and rooted in a traditional and biomedical-oriented approach’.
It was only during the Second Intifada that mental health received increased attention in Palestine. For example, the director of the Health Department at the United Nations Relief and Works Agency (UNRWA) told us, ‘The Second Intifada … put mental health on the agenda in Palestine’, before he continued more forcefully, ‘One can say that the Second Intifada shaped mental health’. The reason for this shift was a reported increase of distress and trauma-related mental disorders due to experiences of extreme violence including the demolition of houses and bombardment of residential areas, an increase in detentions and torture, and the killing of more than 3,135 Palestinians (Giacaman et al. 2009; B’tselem 2005). This took place in parallel with expanded restrictions on movement imposed by Israel consisting primarily of the introduction of hundreds of military checkpoints and regular curfews (UN 2009). These events and their detrimental health and mental health consequences led the Palestinian Ministry of Health to contact the WHO asking for a credible situational analysis of the population’s mental health and the functioning of the mental health system (WHO 2010).
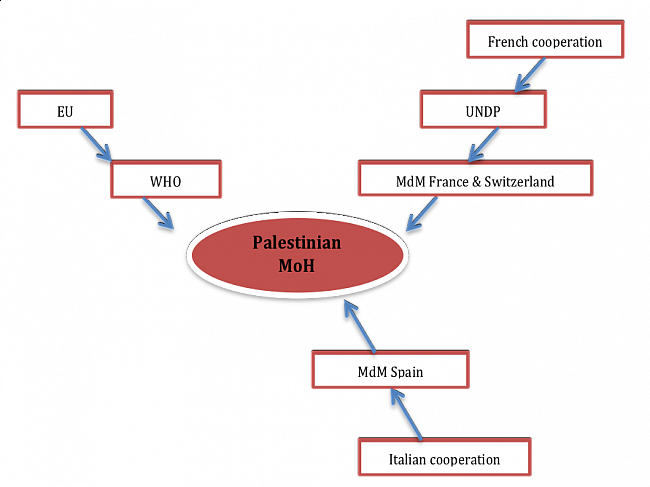
The situational analysis was eventually headed by Benedetto Saraceno, the then director of the Mental Health and Substance Abuse Department at the WHO Geneva, and resulted in attention being drawn to particular gaps in the system and recommendations for future reforms (WHO 2010). The report and recommendations were followed by an operational plan, which was signed by the Palestinian Ministry of Health, the WHO, the French Cooperation, and the Italian Cooperation, to support mental health collaboratively, with additional funding from the EU in 2004. However, as the EU and the French Cooperation and Italian Cooperation were not allowed to directly sponsor non-recognized states, a solution was found by channelling funding to the Palestinian Authority through multilateral and nongovernmental organisations (see figure 1). Thereby, the WHO and Médecins du Monde got directly involved in the first mental health system reform initiatives, and began to work in close collaboration with the Palestinian Authority.
The overall objective of the mental health system reform was ‘developing, reorganizing, improving and expanding current mental health services according to a community-based mental health approach’ (WHO 2009, 21). In concrete terms, this included funding, albeit very limited, for the building of nine community mental health centres (CMHCs), the formulation of a mental health policy, an anti-stigma campaign, and the creation of a Family Association consisting of the family members of people suffering from mental health problems.
However, in 2006, these reform processes were forcibly interrupted. All direct financial support by the international community was withdrawn following the election of Hamas, which was identified as a terrorist organization with which the donor countries refused to formally interact. Our interlocutors explained that this funding freeze resulted in the suspension of the building of several CMHCs and other activities, and that the mental health policy remained unfinished, making it difficult, if not impossible, for mental health professionals to provide adequate community-based mental health care. The situation changed again, in 2007, when the Palestinian factions reached an agreement for Hamas to take over the Gaza Strip and for Mahmoud Abbas to form an emergency government in the West Bank. As a result of this political shift, it became possible for the WHO to apply for funding to underwrite the implementation of the mental health policy that had been previously put into writing.
The EU agreed to provide funds for what is now known as Phase I of the mental health reform (2008–2011) with the goal to reshape mental health and psychosocial support services from an institution-based approach to a community-based one. This entailed the creation of a mental health department within the Ministry of Health, the execution of a baseline study, the development of training materials and schedules, and the first staff training initiatives for those working in primary health care and mental health. However, the reform processes came to a halt again when the funding ran out in 2011. Consequently, the actual integration of mental health into primary healthcare did not take place. As the national officer of mental health at the WHO stated: ‘Training and then nothing. Nobody followed up’.
In 2012, the EU agreed to provide money to start Phase II of the mental health system reform, a three-year project to improve community-based services with a focus on prevention, diagnosis, and treatment of common and severe mental health disorders in primary health care clinics, CMHCs, general hospitals, and tertiary-care facilities. At the time of writing, the funding cycle was about to finish and new applications were being written by the WHO in collaboration with the Palestinian Ministry of Health to persuade the EU to continue their support of the mental health system reform.
This overview makes apparent that this stop-and-go process of mental health system reform is not simply shaped by scientific evidence or best practices in the mental health field. Rather, it is controlled and influenced by large-scale political events, decision-making policies, the demands of donor agencies, and funding scarcity. Interestingly, the influences and effects of these forces on (mental) health system reform remain largely invisible in government and organizational reports. It may be argued that unknowing these power plays is ‘constitutive of social order’ (Geissler 2013, 15) in a two-fold way. First, it allows interventionists to gloss over the fact that intended sustainable program development has been reduced to a project-like patchy effort to change professional practices on the ground and improve the mental health situation overall. Unlike programmes (sustained groups of related projects), projects can react much more flexibly to frequent changes in administration and funding interruptions due to their relatively clearly and often narrowly set goals and predefined end-dates (Jacobsen 2014). Second, unknowing these political power plays allows actors like the EU, multilateral organizations (WHO and UNDP), bilateral development organizations (the French and Italian Cooperations), and other NGOs to provide development aid and engage in institution building without openly questioning the status quo of the Israeli occupation and related human-rights violations, the involvement of Europe and North America in this quagmire, and the possibility of sustainable national development when the occupied Palestinian territories and political institutions are contested and always on the verge of disintegration.
However, we do not want to say that this kind of unknowing takes place in all sectors of society all the time. On the contrary, unknowing political power plays is a partial and context-dependent social action; if the unknown known is transformed into a known entity, new forms of vital unknown knowns are created.
Institutional power struggles and their impact on reform processes
Besides macro-level politics, mental health system reform processes in the West Bank are also affected by power struggles between and within international and local institutions as well as those between differently positioned individual actors. These power dynamics and tensions are partly a result of the weak government-run mental health system, a system that lacks human resources, particularly specialists, and access to adequate medication and infrastructure, and that depends almost entirely on external funding and expertise.
The precarious position of the government-led mental health system was a topic that most of our interlocutors, including Ministry of Health staff, discussed openly. One person stated, for example, ‘I think there isn’t a strong body in the Ministry. The mental health unit was created, but I don’t think that they are really taking leadership. So, there is a lack of leadership in mental health and a lack of coordination’. Similarly, someone working for the Swedish International Development Cooperation Agency, a government agency that used to provide funding for several mental health projects in the West Bank, said, ‘Mental health is an orphaned sector. The Ministry of Health focuses on the “hardware”, that is, building hospitals and centres, and investing in equipment and tools. The “software”, like mental health treatment, is pushed to civil society organizations, who are then left to deal with it’.
This lack of Ministry of Health leadership and expertise, coupled with irregular financial support and investments into material structures that signal measurable outputs (buildings and tools) and accountability (money appropriately spent), has led to a situation in which Palestinian NGOs and the UNRWA have become the central players in mental health system reform processes and the provision of mental health care more generally. In fact, it is they who provide professional mental health training and services, and who are actively engaged in programme monitoring, research, and awareness-raising campaigns. Besides expertise, our interviews and review of NGO websites and grey literature showed that their strength lies in establishing and maintaining bidirectional exchange networks not only among each other but also with a number of foreign NGOs and multilateral organizations. As such, they contribute to the creation of dynamic institutional mental health networks that exist, for the most part, outside of and yet in interaction with the reform process being driven by the Palestinian Authority and the WHO.
Similar to the government sector, local NGOs and the UNRWA are also dependent on external funding from donors that tend to fund time-limited projects directed at particular populations that promise concrete and preferably measurable outcomes. A child protection specialist working at UNICEF told us, ‘Donors want to see something tangible, they want to see numbers. Long-term approaches to therapy and response are often not attractive for donors. … To work with one case for a long time is not interesting. Donors don’t want to provide money for therapy. But funding for psychosocial work is interesting as one can reach thousands of people’. While international support enables the flow of resources in the form of money, in-kind donations, and trainings, these links with international donors also require oversight and management resulting in the development of audit mechanisms. These mechanisms are social practices that allow overseeing how donations are put to use by requesting aid recipients to produce tangible ‘outputs’ such as reports detailing numbers of persons reached and activities performed in a limited period of time.
Strathern (2000, 310) highlights in her work that while audits make certain transactions and outputs visible, they render others invisible, and, consequently, ‘the idea of audit as an obvious instrument of surveillance is thrown into doubt’. We argue that in our case the outward display of buildings, tools, training curricula, number of people trained, and patient registries camouflage what is lacking: ongoing mental health care available to all members of the society. Instead, NGOs rely on short-term psychosocial projects directed at particular populations (such as children); once funding dries up, institutions are required to apply to new calls for applications that might support a completely different population (such as women) with similar or very different therapeutic techniques. As a result, the development of long-term relations between service providers and their clientele, as well as the creation of a sustainable mental health program, is hampered while success stories related to tangible outputs continue to circulate with the hope of attracting future funding.
As donors have organizations in their grip, the latter are hardly able to sustain themselves in times of funding shortages or politically motivated funding freezes. A clinical psychologist working for a local NGO said, ‘One can’t count on them, as they might leave at any time to Syria, Kosovo, Portugal’. After a short pause, he asked himself, ‘Will we, as Palestinians, always look to foreigners and funders to give us money? Or can we build a solid body of psychological [support] where psychotherapists and psychoanalysts are able to offer these services?’ Similarly, other individual service providers we talked to spoke openly about their perception of the current state of the mental health system, thereby making the unknown knowns somewhat knowable. To give a flavour of their frustrations, the following quotes are illustrative of the particular systemic weaknesses and tensions that most of them identified:
Lack of overall mental health system structure and coordination: ‘NGOs [are] doing their own thing; the ministry [is] doing its own thing; UNRWA has different opportunities and challenges’. (coordinator, NGO)
Donor dependency and short-term projects: ‘It’s all done on a project basis and the projects depend on external donors who provide money for one or two years and then, once the money runs out, the projects have to discontinue their work’. (director, NGO)
Shortages of mental health professionals: ‘Each CMHC has a different staff structure. Most CMHCs have just one psychiatrist and one nurse. Other centres have only one nurse and get visited by a psychiatrist a few times per week’. (coordinator, government sector)
Weak education and training system: ‘How can you expect students to become psychologists by simply learning things by heart, with no practical training and limited supervision?’ (psychologist, NGO)
All of the mental health care practitioners and administrators whom we interviewed described the current health care system as fragile and the working conditions as sometimes very challenging, especially in terms of education and training of personnel, access to treatment and medication, salaries, and insurance. Moreover, they had their own visions for a sustainable, locally grounded, and socially acceptable mental health system. Specifically, they highlighted the importance of (1) cooperative efforts to improve coordination between the different stakeholders; (2) establishing a strong educational system through the revision of university curricula, the establishment of international exchange programs, and a properly functioning residency program; and (3) investing in long-term development rather than short-term emergency interventions. However, all study participants agreed that achieving this does not solely hinge on strategic and multisectoral reforms, evidence-based approaches to mental health care, and sustainable finance mechanisms. Rather, the solution must be, first and foremost, a political one beginning with political stability through the end of the Israeli occupation.
What is, in turn, made unknowable in these narratives is the persistent stigma around mental health in many parts of Palestinian society, including the health sector. During our interviews, NGO workers providing training to CMHC staff complained about the stigmatizing attitudes of many mental health workers. Mental health professionals explained that only very few students choose to study psychiatry or psychology – most are rather ‘bumped down’ to these subjects when they fail to have the required grades to enter medical school – and staff of the mental health unit in the Ministry of Health accused their colleagues of sidelining mental health. Someone said, for instance, ‘the Ministry of Health itself stigmatizes mental health and doesn’t think that it is an important field’. Moreover, mental health providers themselves felt stigmatized by the general public for the work they perform. One person said, for instance, ‘When I tell someone that I work in mental health, they react with surprise and with a gasp and say, “Why do you still work in this field? Change your job! You will become like them [patients]’’’.
The stigma and related attitudes toward mental health care seem to suggest that the general population and many health professionals do not, in fact, fully support making mental health system reform an issue of central importance. However, unknowing the stigmatizing attitudes – or at least downgrading them to stumbling stones – that disrupt the provision of better mental health care allows individuals and institutions to continue their much-needed work. As a social practice, unknowing is not solely a destructive force. On the contrary, Geissler (2013, 15) states, ‘nonknowing, like knowledge, can link (and separate) actors and produce, shape, and cut networks, collaborations and social processes’. This creative aspect to unknowing might be an important skill for Palestinian mental health professionals to use in continuing their work despite the myriad power plays and barriers.
We used this case study of the political life of mental health system reform in the West Bank over the past decades to bring to light how these processes are shaped by local and international political events and co-produced by various stakeholders and their institutions. Through these dynamic sociopolitical processes and interactions, relatively flexible and situational knowledges and actions emerge that do not easily map onto top-down evidence-based blueprints for mental health system reform.
Instead, the establishment and reform of mental health systems is something that is created through the interaction of differently positioned actors as well as culture, local and global socioeconomic contexts, and national and international development agendas. In other words, articulations of systemic transformations, unequal power relations between donors and recipients, and practices of exclusion in the context of the Israeli occupation manifest themselves as concrete political constellations that cannot be ignored. Thus, it is important for the aid community to face up to these challenges and stop hiding behind and justifying their work with catchphrases such as ‘evidence-based’, ‘best practice’, ‘sustainability’, and ‘accountability’, and to address the impact of the Israeli occupation, militarized violence, and economic and political oppression head-on when providing systemic mental health support. While it might seem obvious to call for making the unknown known, that is, to lift the veil off public secrets, we know little about the risks involved for the ones who do the unveiling and disturb the social order. For the unknown known to be ‘faced head-on’ it is crucial that a safe space is provided that enables these difficult conversations to happen rather than ostracising and marginalising individuals and institutions working in Palestine and with Palestinians even further.
About the authors
Hanna Kienzler is a Lecturer (Assistant Professor) in the Department of Social Science, Health and Medicine at King’s College London. She has a long-standing academic interest in the field of global health, in connection with organized violence, ethnic conflict, and complex emergencies, and their health and mental health outcomes. She conducts ethnographic research on the impact of war and trauma on women in Kosovo, on new mental health treatment options for torture survivors in Nepal, and on humanitarian and mental health interventions in the occupied Palestinian territories and Kosovo.
Zeina Amro is a PhD candidate in the Department of Social Science, Health and Medicine at King’s College London. The focus of her research is on conceptions of well-being among conflict-affected populations, with a focus on Palestinian refugees from Syria currently living in Jordan. She received her MSc in Political Psychology from Queen’s University of Belfast in 2011, and has worked as research assistant in the mental health unit of the Institute of Community and Public Health at Birzeit University. Amro has conducted research on issues related to mental health among children of Palestinian political detainees; youth participation in rural Palestinian communities; and the concept of dignity among Palestinian youth.
References
Abramowitz, Sharon. 2010. ‘Trauma and Humanitarian Translation in Liberia: The Tale of Open Mole’. Culture, Medicine, and Psychiatry 34, no. 2: 353–79. http://dx.doi.org/10.1007/s11013-010-9172-0.
B’tselem. 2005. ‘Intifada Toll 2000–2005’. BBC News Online, 2 August. http://news.bbc.co.uk/1/hi/world/middle_east/3694350.stm.
Collins, Pamela Y., Vikram Patel, Sarah S. Joestl, Dana March, Thomas R. Insel, Abdellah S. Daar, Isabel A. Bordin, et al. 2011. ‘Grand Challenges in Global Mental Health’. Nature 475: 27–30. http://dx.doi.org/10.1038/475027a.
Cordesman, Anthony H., and Jennifer Moravitz. 2005. The Israeli-Palestinian War: Escalating to Nowhere. Santa Barbara, CA: Greenwood Publishing Group.
Demyttenaere, K., R. Bruffaerts, J. Posada-Villa, I. Gasquet, V. Kovess, J. P. Lepine, M. C. Angermeyer, et al. 2004. ‘Prevalence, Severity, and Unmet Need for Treatment of Mental Disorders in the World Health Organization World Mental Health Surveys’. Journal of the American Medical Association 291, no. 21: 2581–90. http://dx.doi.org/10.1001/jama.291.21.2581.
Geissler, Paul. 2013. ‘Public Secrets in Public Health: Knowing Not to Know While Making Scientific Knowledge’. American Ethnologist 40, no. 1: 13–34. http://dx.doi.org/10.1111/amet.12002.
Giacaman, Rita, Rana Khatib, Luay Shabaneh, Asad Ramlawi, Belgacem Sabri, Guido Sabatinelli, Marwan Khawaja, and Tony Laurance. 2009. ‘Health Status and Health Services in the Occupied Palestinian Territory’. Lancet 373, no. 9666: 837–49. http://dx.doi.org/10.1016/S0140-6736(09)60107-0.
Jacobsen, Kathryn. 2014. Introduction to Global Health. Burlington, MA: Jones & Bartlett.
Kienzler, Hanna. 2008. ‘Debating War-Trauma and Post-Traumatic Stress Disorder (PTSD) in an Interdisciplinary Arena.’ Social Science and Medicine 67, no. 2: 218–27. http://dx.doi:10.1016/j.socscimed.2008.03.030.
Kienzler, Hanna. 2012. ‘The Social Life of Psychiatric Practice: Trauma in Postwar Kosova’. Medical Anthropology 31, no. 3: 266–82. http://dx.doi.org/10.1080/01459740.2011.623287.
Kienzler, Hanna, and Duncan Pedersen. 2012. ‘Strange but Common Bedfellows: The Relationship between Humanitarians and the Military in Developing Psychosocial Interventions for Civilian Populations Affected by Armed Conflict’. Transcultural Psychiatry 49, no. 3–4: 492–518. http://dx.doi.org/10.1177/1363461512447927.
Meffert, Susan, and Solvig Ekblad. 2013. ‘Global Mental Health Intervention Research and Mass Trauma’. Open Access Journal of Clinical Trials 5: 61–69. http://dx.doi.org/10.2147/OAJCT.S37037.
Patel, P. P., J. Russell, K. Allden, T. S. Betancourt, P. Bolton, A. Galappatti, Z. Hijazi, et al. 2011. ‘Transitioning Mental Health and Psychosocial Support: From Short-Term Emergency to Sustainable Post-Disaster Development. Humanitarian Action Summit 2011’. Prehospital and Disaster Medicine 26, no. 6: 470–81. http://dx.doi.org/10.1017/S1049023X1200012X.
Sphere Project. 2004. Humanitarian Charter and Minimum Standards in Disaster Response. Oxford: Oxfam.
Strathern, Marilyn. 2000. ‘The Tyranny of Transparency’. British Educational Research Journal 26, no. 3: 309–21. http://dx.doi.org/10.1080/713651562.
Taussig, Michael. 1999. Defacement: Public Secrecy and the Labor of the Negative. Stanford, CA: Stanford University Press.
Tol, Wietse A., Corrado Barbui, Ananda Galappatti, Derrick Silove, Theresa S. Betancourt, Renato Souza, Anne Golaz, and Mark van Ommeren. 2011. ‘Mental Health and Psychosocial Support in Humanitarian Settings: Linking Practice and Research’. Lancet 378, no. 9802: 1581–91. http://dx.doi.org/10.1016/S0140-6736(11)61094-5.
United Nations. 2009. ‘UN Report on Human Rights in Palestine and Other Occupied Arab Territories: Report of the United Nations Fact Finding Mission on the Gaza Conflict (Goldstone Report)’. http://www2.ohchr.org/english/bodies/hrcouncil/specialsession/9/docs/UNFFMGC_Report.pdf
World Health Organization (WHO). 2006. ‘Community Mental Health Development in the Occupied Palestinian Territory: A Work in Progress with WHO’. Geneva: WHO. http://mhinnovation.net/sites/default/files/downloads/innovation/reports/Report-Community-Mental-Health-Development-in-Palestine.pdf.
WHO. 2009. ‘WHO-AIMS Report on Mental Health System in West Bank and Gaza’. Geneva: WHO. http://www.who.int/mental_health/evidence/west_bank_and_gaza_who_aims_report.pdf.
WHO. 2010. ‘Country Cooperation Strategy for WHO and the Occupied Palestinian Territory 2009–2013’. Geneva: WHO. http://www.who.int/countryfocus/cooperation_strategy/ccs_pls_en.pdf.