Naming and forgetting
Sowa Rigpa and the territory of Asian medical systems
—
Abstract
For the sake of living beings, the emanations of the Sugata [Buddha]taught the preparation of medicine in India, cauterization and channel cleansing in China, mainly bloodletting in the land of Dolpo,pulse and urine diagnosis in Tibet, the Science of Healing Collection [gso dpyad ’bum pa] to the gods, the Caraka Aṣṭavarga to the Rishis, the Black Iśvara Tantra to the ‘non-Buddhists’, and the Guardian of the Three Lineages to the Buddhists. All these [medical teachings] are included in this medical tantra [Four Treatises]; there is no medical practice not within it. The Great Compassion has no partiality, but things appear according to individual disposition. Just as a single moon in the skyappears as individual moons in every water urn, one teaching was delivered but many were understood.
– [Desi] Sangye Gyatso (1982b, 67/6–18), quoting Yuthog Yönten Gonpo (1982, 660/6–14)[note 1]
I think it is better to use the classical term Sowa Rigpa for amchi medicine in Nepal. The nomenclature matters a lot in [the] longer term.
– Dr. Padma Gurmet, director of the National Research Institute for Sowa Rigpa, Ladakh, India, advising Nepali practitioners on paths to national recognition (e-mail message to Craig, September 2015)
The subaltern groups are tied also to specific places, but their ties are to the particularity of local settings, rather than a lifestyle potentially available to the hegemonic group everywhere.
– Paul Connerton (2009, 133)
Introduction
Much can be said about the work of naming – what it accomplishes and what it elides.[note 2] The process of deciding upon a name for something such as a form of medical practice is an act of classification that can have high stakes in terms of knowledge ownership, contested identities, and belonging within and beyond nation states. Naming practices are exercises in power and legitimacy, even as the meanings of names can change over time. In this article, our object of analysis is Sowa Rigpa (gso ba rig pa). Often translated as ‘science of healing’, this term is now viewed widely as a synonym for ‘Tibetan medicine’, not only by a range of practitioners and institutions in Asia but also, increasingly, in academic literature and in the global circulation of therapeutic practices derived from Asia. This collaborative piece of scholarship in fact resulted from our individual academic experiences of having to define these terms in each paper we write, becoming actors ourselves in the global dissemination of terminology and the politics of naming. Our frequent discussions and own decision-making regarding the usage of Sowa Rigpa versus Tibetan medicine in academic publications inspired and urged us to write this article.
Although Sowa Rigpa has come to be synonymous with Tibetan medicine, it has meant different things to those writing and speaking in Tibetan and related languages over the centuries. As Fjeld and Hofer (2010-11, 177) point out, ‘Before the twentieth century, there was little need to identify the diverse bodies of Sowa Rigpa knowledge, practice, and experience as either Tibetan or ‘traditional’; they were simply referred to by Tibetans as ‘medicine’ (sman) or as ‘sowa rigpa’. Throughout the article we distinguish these two uses by capitalizing Sowa Rigpa when it stands for the formal name of a medical system, as with Ayurveda or Traditional Chinese Medicine, and use it in italicized lower case as sowa rigpa when we are discussing it as a multivalenced term in circulation.
In this article, we explore major trajectories in the transformation of sowa rigpa as a term, and ask what this says about Sowa Rigpa as a medical system. We understand this medical system to be a broad collection of practices that are neither homogenous nor closed but that share textual orientations and epistemological grounding (see Pordié and Blaikie 2014; Gerke 2011; Schrempf 2007; Samuel 2008). We examine the etymological and sociohistorical roots and transfigurations of this term in Tibetan medical texts, in the self-representation of contemporary institutions both within and beyond Asia, in its usage among practitioners themselves, and in the context of academic discourse. In doing so, we aim to address the following questions: What encompasses rigpa – a word often glossed as ‘science’ but that might also be translated as ‘field of knowledge’ – in a Tibetan context? What is meant by sowa, ‘healing’? When did Sowa Rigpa come to mean ‘Tibetan medicine’ and how has the term been used in the promotion of this medical tradition in national and transnational contexts? And what does this tell us about the politics of naming and about the larger changes that medical traditions in Asia undergo when their names are popularized or used for political or even commercial ends? We explore how the use of ‘foreign’ terms, for example the Sanskrit‘vidyā’ or the English ‘science’, have underlined certain types of authority in the process of naming – in this case as Sowa Rigpa has come to be used not only synonymously with but also more visibly than Tibetan medicine. We also link these inquiries to debates on cultural memory. Following Paul Connerton (2009, 2011), we ask: what forms of ‘forgetting’ must be employed so that the meaning of a name can be transformed over time, toward distinctly contemporary goals, even if done in the name of preserving ‘tradition’?
The transformation of sowa rigpa as a term has involved turning a vernacular concept in the Tibetan language into an idiom that sounds ‘authentic’, perhaps even ‘exotic’, when used in English-language contexts or in global situations, by Tibetan speakers and non-Tibetan speakers alike. By ‘vernacular’ we mean a formal technical and literary term that is also used in common speech. As one of our peer reviewers pointed out, a similar dynamic has occurred with Ayurveda and Yoga. At the same time, sowa rigpa has come to reflect political concerns, from the loss of territory and national identity among diasporic Tibetans and constrained forms of ethnic autonomy within the People’s Republic of China (PRC) (see Glover 2006) to the politics of ‘Tibetanness’ in national or regional contexts such as Nepal, Mongolia, or Ladakh, India – places where the medical practice flourishes among people who are not, as such, ‘Tibetan’. As a form of strategic essentialism, Sowa Rigpa exists as the label for a medical system that is experienced in diverse ways and places yet still affectively, morally, and textually linked. At the same time, the term allows practitioners to connect this label to certain concepts of citizenship and what it means to be a doctor these days. It is a term that seemingly transcends the nation state even as it is also bound up with struggles for national recognition, and, simultaneously, is becoming visible on the global stage. As such, we are interested not only in tracing the historical roots of this term but also in describing how Sowa Rigpa has come to occupy powerful virtual and global spaces, even at times becoming like a brand. We argue that the use of this term makes possible forms of ‘virtual’ belonging among practitioners, even as forgoing ‘Tibetan medicine’ for Sowa Rigpa may be disquieting to some practitioners. By ‘virtual’ we do not exclusively refer to Internet connectivity, even though the Internet and social media increasingly play a significant role in sowa rigpa-related communication, but primarily to a sense of belonging that is not bound to territory or nationhood but that is tied to shared epistemologies of practice, shared concerns about access to materia medica and desires to produce efficacious medicines, and shared moral frameworks, rooted in Buddhism (Blaikie et al. 2015).
In her afterword to a special issue of East Asian Science and Technology Studies (EASTS) devoted to Himalayan and Tibetan modes of healing, Elisabeth Hsu (2013, 506) cautions, ‘By adhering to the practitioners’ naming of the practice, a political orientation may find entry into academic discussion more easily than is desirable’. Our work contributes to Hsu’s analysis of the ‘politics of practice’ in which ‘a name connotes not only ongoing polemics of legitimation … but also hegemonic political histories’ (Hsu 2013, 507). We understand that there is as much at stake in belonging to a nation state as to a family lineage (Pordié and Blaikie 2014), and that specific identity politics are being enacted when the term ‘Sowa Rigpa’ is chosen over a term like ‘Tibetan medicine’ (Kloos, this issue; Blaikie, this issue). In her 2013 essay, Hsu suggests the term ‘East Asian Medicine’. Despite its imperialistic overtones, she argues that it might be a better choice to overcome nationalism linked to terms for traditional medicine in China, Mongolia, Japan, Korea, and Tibet. However, she also acknowledges that since Sowa Rigpa has strong historic links not only with East Asia but also with South Asia and the Arab world, such an umbrella term might not encompass all there is to this ‘current of tradition’ (Scheid 2007). We agree with Hsu’s problematizing caveat and would push it further. We argue that the fundamentally transnational nature of Sowa Rigpa – the terrain of practice it encompasses – can help to complicate and productively challenge the ways that ‘national’ traditional medicines have been situated in South and East Asian contexts, and how ‘Asian medicine’ has been positioned globally. Seeing Sowa Rigpa as something that can function within and across specific territories, andthat can operate in de- and reterritorialized global spaces, exemplifies how, why, and to what end modernity forgets (Connerton 2009).
Finally, we argue for the need to explore how and to what extent practitioners’ self-representation and the evolving conventions of scholarly work (by both native and non-native scholars) have co-produced new meanings for the term. To this end, we reference forms of collaborative ethnography focused on the coproduction of knowledge in Sowa Rigpa spaces (Blaikie et al. 2015) as well as scholarly work being produced in English by Sowa Rigpa practitioners (Gurmet 2004). We also acknowledge that local contingencies – for example Nepali practitioners using the term ‘Sowa Rigpa’ as a way of avoiding the term ‘Tibetan’ for fear of political repression – have also informed the theorization of contemporary Tibetan medicine, for example in the conceptualization of a ‘sowa rigpa sensibility’ (Adams, Schrempf, and Craig 2010) as a way of recognizing epistemological claims that are distinct from, but operating in relation to, those of biomedicine.
We aim to spur questions not only about why names matter but also how names gain momentum. Momentum emerges through a dialectical relationship between political efforts toward recognition and support of a ‘traditional’, ‘alternative’, or ‘minority’ practice in national and transnational contexts, as well as through scholarly work to document and analyze such efforts. We also note an increasing engagement among Sowa Rigpa practitioners in transnational and deterritorialized spaces, which has engendered new forms of self-representation. As Shneiderman (2015) has shown in relation to the category ‘ethnicity’ in her work with Thangmi communities between Nepal, India, and the PRC, we understand contemporary choices by practitioners and their institutions to adopt the term ‘Sowa Rigpa’ as illustrative of a performative claim of belonging to a particular tradition in specific sociopolitical contexts, often with distinct goals. And yet, also following Shneiderman, we argue that the adoption of such naming strategies is not merely strategic and aimed at ‘outside’ audiences (ministries of health, international foundations, and so forth); the term ‘Sowa Rigpa’can also produce strong affective responses among those on the ‘inside’ of this tradition. As with Shneiderman’s recognition of how her ethnography has helped to ‘produce’ Thangmi as a recognizable ethnic category in pursuit of rights, resources, and political representation, we also acknowledge our role as scholars in helping to produce the evidence by which Sowa Rigpa has gained currency and gone global, even as the term means different things to people enmeshed in the work of healing in specific local contexts.
Methodology
This article is based on a close reading of the etymology and textual history of the term sowa rigpa, combined with study of ethnographic and contemporary media sources on its place in the discourse and practice of Asian medical systems. In addition to textual sources in Tibetan language and, in some cases, their English and Chinese translations, we rely on various forms of gray literature (websites, brochures, reports, and public and academic presentations) that adopt the term sowa rigpa as a descriptor and/or Sowa Rigpa as a formal name for this medical system. Such sources provide additional forms of evidence for the ways that this term’s meaning has shifted over time, becoming a sign of belonging and global identification, even as it might not indicate shared practices or shared politics among practitioners.
We weave into our analysis views from medical practitioners from India, Nepal, and the PRC, to understand how variedly they associate with this term and what it means to them. Although the words of many practitioners inform our analysis, interviews with three individuals have directly shaped this paper. Dr. Namgyal Qusar was trained at the Men-Tsee-Khang institute in Dharamsala, India, and established his own clinic, the Qusar Tibetan Healing Centre in Sidhbari, near Dharamsala in northwestern India, where he produces his own medicines and sees patients. Dr. Tenzin Bista is a Buddhist monk in the sakya tradition as well as a medical practitioner and the cofounder of Lo Kunphen, a school, pharmacy, and medical clinic based in Mustang District, Nepal, on the border with the Tibet Autonomous Region, China. In addition to his monastic training, he hails from a family of medical practitioners. Dr. Mingji Cuomo graduated from the Tibetan Medical College in Lhasa and holds degrees in medical anthropology and public health from European universities. She worked at the Lhasa Mentsikhang and the Shongpalhachu Tibetan Medical Factory and is currently part of an EU-funded research project on Tibetan pharmaceuticals (www.ratimed.net). Gerke interviewed Namgyal Qusar, Craig interviewed Tenzin Bista, and we interviewed Mingji Cuomo together. We also draw on informal conversations with each of these individuals as well as with other practitioners from Nepal, India, and China to whom we have directly asked questions about the history and current use of the term sowa rigpa. While some of the conversations with Bista occurred at his clinic in Nepal in 2015, others took place while he was visiting the United States in 2014 and during an international conference in 2013. The interviews with Cuomo took place via Skype in 2014 and those with Qusar both at his clinic in India in 2014 and during international meetings, workshops, and conferences between 2013 and 2015. This fact is itself illustrative of the globalization of this tradition and the importance of such events as ‘field sites’ in their own right (Blaikie et al. 2015; Blaikie, this issue).
These practitioners present differential analyses of this multivalent term: its history and current use. They use and understand this term in varied ways. And yet each would agree that it has come to be, in the words of Qusar, a ‘political-technical term’. To varying degrees, each feels that the term can help create a wider acceptance of their practice and all it connotes, though they do not necessarily or fully identify with the term itself. The de-territorialized belonging that the term inspires seems to at once reaffirm and challenge the boundaries of subjectivity among these practitioners.
Sowa rigpa: Etymology and history
What is the etymology of the term sowa rigpa within Tibetan medical sources? How has it been interpreted over time? In what follows, we present a succinct answer to these questions, based largely on the varied use of the term in titles of Tibetan medical works. While this is not based on extensive textual research, it helps to illustrate one of the key points of this article: namely, that what began as a broad term denoting allmedical systems from within a Tibetan sociolinguistic framework (sowa rigpa) has come to be reframed, first as an essentially Tibetan medical system and, now, as Sowa Rigpa, a system that signifies practice and belonging well beyond Tibetan regions of the PRC or the Tibetan diaspora.
We do not know much about early Tibetan terms for Sowa Rigpa from the era of the Zhang Zhung kingdom, predating the arrival of Buddhism to Tibet. In Zhang Zhung language, ‘sorig’ (gso rig) or ‘soche’ (gso byed or gso byad), and perhaps also ‘sowa’ (gso ba) or ‘tsowa’ (’tsho ba), are termed ‘tsochi’ (’tsho ci), which may be a Zhang Zhung back formation that derives from a Tibetan term for doctor, ‘tsoche’ (’tsho byed) (Henk Blezer, e-mail message to Gerke, July 2016). The term ‘tsoche’, however, is rarely used today to describe practitioners; the term ‘amchi’, a loanword from Mongolian (emchi), is much more common, as is the term ‘menpa’(sman pa), literally ‘medicine person’ or ‘one who confers medicine/healing’. The similar phonetics of ‘tsowa’ and ‘sowa’ and their similar meaning might point to common linguistic roots. The Tibetan religion known as Bon developed alongside Tibetan Buddhism in the eleventh century (Van Schaik 2011). The Four Treatises (Rgyud bzhi) is a foundational medical text codified in the twelfth century that remains the primary source for studying Sowa Rigpa today. Its Bon equivalent is titled Sorig Bumshi (Ggso rig ’bum bzhi), but this is a ‘current term’ (Blezer, e-mail message to Gerke, November 2016); the contents of these texts are largely identical. In either case, ‘tsowa’ means ‘livelihood, sustenance, nourish, survival, cure, be alive and keep alive’, and ‘sowa’ means ‘to enhance, feed, nourish, strengthen, heal, cure’ but can also, in Bon texts, refer to restoring objects to ideal states (e.g. sharpness to a knife) and can be used metaphorically (THL 2010).
These definitions were echoed by Tenzin Bista from Nepal: ‘The meaning of sowa, it is related to Bodhisattva mind [byang chub gyi sems] because it is about taking care [in English]. As doctors we must put the needs of our patients first. The aim of sowa rigpa is to alleviate suffering, and this intent is in the word itself’. This reading by Bista underscores a distinction also in the Four Treatises, namely that anything that can bring benefit to the patient should be considered part of sowa rigpa.
Sowa rigpa combines what is likely an ancient Tibetan cognate (’tsho ba) with a concept that can be considered to have been ‘borrowed’ during the transmission of Buddhism from India to Tibet. The concept of rigpa emerges from the Sanskrit cikitsāvidyā, which was one of the five major fields of knowledge, often simply called the ‘five sciences’, taught at Indian monastic universities, the other four being esoteric learning (nang rig pa, now often translated as ‘Buddhism’), logic (gtan tshigs rig pa), grammar or language (sgra rig pa), and arts and crafts (bzo rig pa). This classification was set around the fourth century CE by Asaṅga. It was adopted by Tibetan writers in the ninth century and generally employed up until the late seventeenth century, when the five sciences were more deeply linked to politics and forms of government in Central Tibet, largely under Desi Sangye Gyatso, the Fifth Dalai Lama’s regent and one of the most important figures in the development and dissemination of medical knowledge in Central Tibet (Schaeffer 2011, 292–93). Among the five major sciences, logic, language, and Sowa Rigpa underwent a more formal codification in written treatises, while arts and crafts were taught by craftsmen and appeared more in commentaries than classical treatises (Schaeffer 2011, 292). The Tibetan translations of Sanskrit medical works that were included in the commentaries of the Tibetan Buddhist canon, the Tenjur, also classified Sowa Rigpa as one of the ten sciences – the five major as outlined above as well as five minor sciences: grammar (sgra), poetics (snyan ngag), metrics (sdeb sbyor), drama (zlos gar), and lexicography (mngon brjod). Here again, although sowa rigpa is used as a classificatory marker of medical works regardless of their place of origin, it referred to the various medical traditions that were known to the Tibetan world – but not limited to Tibet – at that time in history, including Indian, Chinese, Central Asian, and Greco-Arab texts and practices.
Not only can sowa rigpa be considered a borrowed term, it is also accompanied by an adopted sense of ‘science’ that came along with its translation from Sanskrit to Tibetan. However, the ten areas of knowledge traditionally studied in Buddhist monasteries also have become conventionally translated as ‘science’ (rigpa). When speaking of traditional medicine in contemporary contexts, the term ‘science’ can be fraught, given the ways that the term links to value systems defined in relation to biomedicine (Adams 2002). But ‘science’ here can also be interpreted as ‘a field of knowledge’ or an academic or monastic ‘discipline’. Where ‘science’ leaves off and ‘religion’ begins remains rich epistemological and cultural terrain (see Adams, Schrempf, and Craig 2010). Yet we cannot think of Sowa Rigpa simply as ‘Buddhist medicine’; it is rather a process ‘moving toward a scientific and empiricist mentality’ that has been influenced by ‘Buddhist habits of thought and practice’ over time (Gyatso 2015, 16–17).
In fact, Janet Gyatso (2004, 5) has recently argued that in Tibet, medical practitioners developed their own epistemic orientations and material focus with a ‘scientific sensibility’. This intellectual development took place within the context of state-sponsored Buddhism and esoteric tantric Buddhism, and largely outside the intellectual developments of European modern medicine of the time (Gyatso 2015). Thus, ‘scientific thinking’ in Tibet might look different from the Enlightenment ‘science’ of Europe. Tibetan practitioners present and use the term ‘science’ today in multiple and fluid ways, depending on with whom they are speaking; but with respect to sowa rigpa etymology, we are referencing a long tradition in science and philosophy before the advent of ‘modern science’, which in itself is an ambiguous term. Thus our discussion also has to do with other ideas of self-representation. The English translation of Sowa Rigpa as ‘science of healing’ in many modern works in fact reveals the dialectic relationship between sowa rigpa and Sowa Rigpa – the fluid practice and the reified medical system – reflecting issues of social prestige and validation that include the use of ‘science’ as a political strategy in varying Tibetan contexts (Adams 2002).
As with many other forms of knowledge that traveled from the Indian subcontinent to the Tibetan plateau, the conceptual frameworks for understanding health and responding to illness became linked to local, indigenous, and ‘enskilled’ practices. Here, following Tim Ingold (2000, 2011), we understand such ‘enskilled’ practices to be not just technical skill but rather embodied ways of perceiving, dwelling within, using, and making sense of one’s environment – not only the physical environment but also the internal worlds of the body, as linked through Sowa Rigpa conceptualizations of health and disease. This ‘vernacularization’ occurred over a long period, between the ninthand seventeenth centuries, and was very diverse. For example, in the Four Treatises, sowa rigpa refers to both a general category of knowledge as well as to a diversity of medical traditions known at the time, as expressed in the epigraph to this article. Not only are there references to medical practices in places as specific as Dolpo (a culturally Tibetan region in what is today northwestern Nepal) but we are also reminded that, ‘All these [medical teachings] are included in this medical tantra[Four Treatises]; there is no medical practice not within it’ (emphasis added) (Sangye Gyatso 1982b, 67/13–14). This diversity is at the core of what is meant by ‘medicine’ during the disseminations of Buddhism to Tibet, a meaning consonant in the seventeenth century, as evidenced by how it is still quoted by Sangye Gyatso (1982b, 67/16–18) in his work on medical history, the Mirror of Beryl: ‘Just as a single moon in the sky appears as individual moons in every water urn, one teaching was delivered but many were understood’. Note that he quotes from the Four Treatises here, which uses the older term ‘soche’ (gso dpyad) for medicine, not ‘sowa rigpa’.
To Sangye Gyatso, writing in the seventeenth century, the term sowa rigpa meant more than one thing. In the Mirror of Beryl he uses it in two ways: first, as one of the forms of knowledge following the Indian tradition of the five major sciences, and second, as a general term to delineate the medical traditions of the various gods and Bodhisattvas (Schaeffer 2011, 299). Sangye Gyatso (1982b, 19/17–20/6; see also Kilty 2010, 48–49) discusses how Bodhisattvas study the science of healing, and then defines the term as follows:
Therefore, it is definitely part of bodhisattva conduct and a field of endeavor for the wise. In Sanskrit this science is known as āyurveda. ‘Lifespan’ (tshe, āyuș) and ‘life force’ (srog, prāṇā) are synonyms. ‘Life’ (’tsho ba, jīva) is the basis of consciousness. In the desire and form realms, it is the basis for warmth and consciousness. Knowledge of this life is the science of life. The Sanskrit term cikitsā means ‘expertise in healing’. It is the expertise in balancing the disordered elements or constituents of the body. It is also referred to as the ‘science of healing’ (gso ba rig pa) or cikitsā vidyā.
This quote is noteworthy in that it defines sowarigpa as a ‘field of endeavor’ (gzhol pa’i gnas, lit. ‘a place to work hard’) whose conceptual basis and humanistic utility is evidenced not only through a lineage of texts but also through ‘expertise in healing’ (gso ba’i dpyad). Here, ‘expertise’ should be understood as practices of examination and analysis – an ‘enskilled’ way of being that occurs in the process of balancing the body in day-to-day life. It is not just textual or theoretical knowledge that makes something a sowa rigpa practice; it is putting that knowledge into action in particular contexts. Contemporary Tibetan physicians still recognize this concept of enskillment and even include it in their definitions. Mingji Cuomo translated the term to us as follows: ‘My translation is: “science and art of healing”. The entire Four Treatises are written in a very artistic way of order. It is all poetry, they have a lot of artistic things inside, not … only how to live a healthy life, but you can actually understand the essence of life’.
In a similar vein to the expansiveness described in Sangye Gyatso’s work, and with an appreciation of the complexity of the term akin to Cuomo’s, Tenzin Kunsel (2015), an administrator at the Central Institute of Tibetan Studies in Sarnath, India, translated the term as ‘science of restoration’ in a recent presentation. He explained that when he spoke about this translation in conversations with exiled Tibetan practitioners in India, they felt that ‘healing’ was ‘too small a word to describe what sowa rigpa is’. So this administrator from a leading Tibetan institution was instructed to translate sowa as ‘restoration’, signaling to this global academic audience that it was more than just about ‘fixing a disease’ but rather a philosophy and practice that ‘is about overall connection to health, to mind–body balance’.
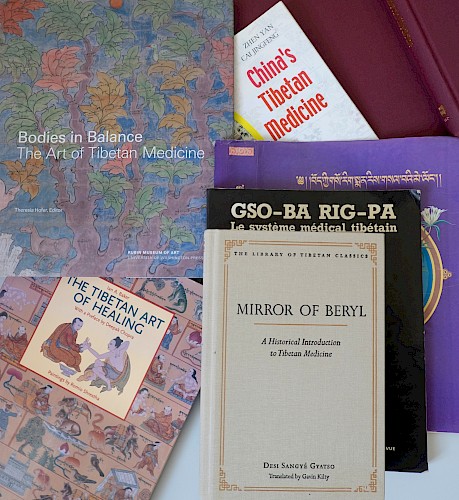
As such, in both historical texts and their contemporary interpretations, we learn that sowa rigpa involves practical skills that have manifested in many different traditions of healing, for example in the ‘celestial realm’ as well as in Ayurveda and Indian medical traditions (all described in several chapters of the Mirror of Beryl). The Mirror of Beryl is thus, in the words of Namgyal Qusar, a ‘history of medicine, not a history of Tibetan medicine’ (emphasis added), even though it is often presented as such – for example, in the subtitle of Kilty’s translation, A Historical Introduction to Tibetan Medicine. As we shall see, the use of ‘Tibetan’ or bö (bod) in the title of Tibetan medical texts is largely a creation of modern Tibetan authors and appears predominantly in twentieth-century medical titles and in Western academic and nonacademic translations. As one of the peer reviewers for this article pointed out, sometimes ‘Tibet’ is also replaced by ‘Snowland’, which is a geographically more inclusive and less politically loaded term (see for example Jampa Trinlé 2000).
From sowa rigpa to Tibetan medicine
So, how does sowa rigpa become ‘Tibetan medicine’? As a way of addressing this question, first let us go back to the Four Treatises and the appearance of the term in this seminal medical work. The term appears in the beginning of the Four Treatises as a general expression for ‘science of healing’ as taught by the Buddha. The first chapter of the Four Treatises presents an Indian mythological setting, where the Medicine Buddha at the center of a mandala is surrounded by four types of disciples: Gods (Devas), Sages (Rishis), Buddhists, and non-Buddhists. The Medicine Buddha delivers the teachings of sowa rigpa to all of the surrounding disciples, each of whom understands it according to their own system of belief. This emphasizes a kind of openness and multivocality to the meaning of this term. Yet, in this version of medical history, it is only when the Buddhist disciple Yilekye understands the medical teachings ‘in accordance with the tradition and system of their own Master’ (translation by Men-Tsee-Khang 2008, 9), that Sowa Rigpa begins its sojourn as a medical science of healing expressed in Tibetan cultural terms. This is evident from the focus on materia medica and foods prevalent in Tibetan regions, which are then mentioned throughout the text in the form of dietary prescriptions or recipes (Kilty 2010, 7). Qusar explained the emergence of Sowa Rigpa as specifically ‘Tibetan medicine’ during an interview at his Tibetan medical clinic in northwest India:
At that very beginning [of the Four Treatises or Gyushi] the term means not only Tibetan medicine but all kinds of science of healing. During the time the Medicine Buddha was teaching the Gyushi you find all kinds of disciples, and they each practice their traditions, which are also considered sowa rigpa. In the second chapter, the purpose of studying sowa rigpa is mentioned. Then the disciple and master have a dialogue, and the disciple requests him to teach the Gyushi, and from that [point] onwards it is Tibetan medicine.
The term ‘Tibetan medicine’ does not appear in the Four Treatises nor does the text present itself as a work on ‘Tibetan medicine’. The term for Tibet, ‘bö’, appears only in the ‘Concluding Chapter’, in a list of different medical practices that the Buddha taught in various countries, including Tibet, here called‘böyül’ (bodyul)[note 3] (Yuthog Yönten Gonpo 1982, 660/8). The identification of Sowa Rigpa with ‘Tibetan medicine’ in the Four Treatises as expressed by Qusar is neither a literal synonym nor does it parallel a political entity of a nation – except from his contemporary perspective.
Qusar’s interpretation of what comprises sowa rigpa and ‘Tibetan medicine’ in the Four Treatises inspired us to ask the question: how have Tibetan medical authors over the centuries dealt with these labels in the titles of their written works? Even a short analysis of the 250 titles of Kurtis Schaeffer’s ‘Chronological Medical Texts List’ (2010) points to a notable trajectory[note 4]: before the seventeenth century only two works use the term ‘sowa rigpa’in their title, and ‘bömen’(bod sman) appears only in twentieth-century titles. This does not mean, however, that it is a new term. ‘Sorig’[note 5] and ‘bömen’[note 6] are old terms that appear in classical Tibetan medical literature, but they appear much more prominently in modern post-1959 titles. A search for ‘bömen’ in the Tibetan Buddhist Resource Center database lists thirty-one medical works, which are also predominantly modern publications.[note 7]
Between the eighth and sixteenth century, titles of medical works more frequently refer to the Indian tradition of the ‘Eight Branches’ (yan lag brgyad). We also find the term ‘medical treatise’[note 8] (sman gyi bstan bcos, for example, in Rangjung Dorje 2006) or the term for physician, ‘soche’ (for example, in Yuthog Yönten Gonpo 1967, text 17; Drakpa Gyaltsen 1993) or ‘menche’ (for example in Tashigang 1989). During the seventeenth century, the famous physician of the Drikung medical school, Drikung Chökyi Drakpa (1999), uses the term ‘sowa rigpa’ in the title of his medical work ’Bri gung gso rig gces bsdus, thus emphasizing the naming of medical knowledge according to certain medical schools in Tibet, here the ‘Drikung science of healing’. This naming practice is indicative of claims to lineage-based authority but also to the ways such practices overlap with the founding of medical ‘schools’ or ‘houses’ (Craig 2012; Pordié and Blaikie 2014; Hofer forthcoming; Travers 2015).
It appears that Sowa Rigpabecame a more representative label for the centralized and institutionalized forms of Tibetan medicine as Desi Sangye Gyatso consolidated medical science into his political agenda (Schaeffer 2003; J. Gyatso 2004, 2015). However, the more frequent use of the term in the titles of Sangye Gyatso’s works[note 9] and in those of his contemporaries might just point to the medical sciences becoming more prominent during this era rather than actually indicating a change in the representation of the newly institutionalized Tibetan medical traditions as Sowa Rigpa in the late sixteenth and early seventeenth centuries (J. Gyatso, pers. comm. with Gerke, February 2015). Sangye Gyatso does not imply that Sowa Rigpa is equivalent to ‘Tibetan medicine’ or bömen, or the ‘Tibetan science of healing’ or böki sowa rigpa (bod kyi gso ba rig pa). Rather, he still uses it as a way to name distinct systems of healing. As noted above, the need to call sowa rigpa knowledge ‘Tibetan medicine’ or ‘traditional’ is a twentieth-century phenomenon, as is the shift to viewing Sowa Rigpa as a synonym for Tibetan Medicine.
This change occurred as Tibetans developed new nationalist sensibilities, which also include expressions of cultural ownership, during the twentieth century and into the twenty-first century, particularly after the Chinese annexation of Tibetan regions and the PRC Communist Party-controlled installation of ‘ethnic minority medicine’ (shaoshu minzu yixue) policies. Contemporary Tibetan language texts published in China began to use the term sowa rigpa but in ways that qualified this term in some cases as overtly Buddhist (bstan ‘gyur nang gi so ba rig pa;Pha khol 1989) or overtly Tibetan (bod gyi gso rig;Kunchok Gyaltsen et al. 2007; bod lugs gso rig;JampaTrinlé 2008). In cases where Tibetan language titles are translated, they are glossed as ‘Tibetan medicine’ or ‘medicine of Tibet’ (Xizang yiyao) in English and Chinese (Glover 2005). Conversely, Chinese publications in English use titles such as ‘‘‘Chinese Tibetan medicine” or “Tibetan medicine of China”, always educating the reader about the correct framework of interpretation’ in political terms (Saxer 2013, 19; emphasis added). For example, a compendium of writings by the famous Tibetan physician Jampa Trinlé (1928–2011) was recently republished in Chinese, English, and Tibetan under the English title China’s Tibetan Medicine, a most direct claim to national Chinese ownership of this Tibetan knowledge system (Jampa Trinlé 2013; see also Yan and Jingfeng 2005). Significantly, the Tibetan language title of this book mirrored the English (krung go’i bod kyi gso ba rig pa;JampaTrinlé 1996); krung go’i signifies ‘Chinese’ (and is the politically correct term in Tibet for the PRC) but is, interestingly, a Tibetan transliteration of the Mandarin itself (zhong guó) rather than the more common Tibetan word for ‘Chinese’, rgya nag.
In the Tibetan exile context, efforts to identify Sowa Rigpa as an explicitly Tibetandomain also began in earnest. This period, beginning in the 1980s, ushered in the first major works to reach English-speaking audiences about this medical system, as well as a first wave of strong scholarly collaborations between Tibetan physicians and Western scholar–practitioners. Terry Clifford’s Tibetan Buddhist Medicine and Psychiatry (1984) was followed byDr. Yeshi Donden’s Health through Balance: An Introduction to Tibetan Medicine (1986) and Barry Clark’s The Quintessence Treatises of Tibetan Medicine (1995). In the first text, something that might not be well known to a Western audience was connected to a recognizable concept, psychiatry. In the second, Donden aimed to describe a core epistemological orientation of the medical system in ways that the uninitiated would understand. In the third, Tibetan medicine was made somehow more authentically esoteric through an English gloss of the Tibetan titles for the first two books of the Four Treatises. The term sowa rigpa is scarcely seen in these texts, which were all produced in collaborations between Western scholars and Tibetan physicians living and working in exile.
By the 1990s, several texts featuring the paintings commissioned by Sangye Gyatso to illustrate the Blue Beryl were published with English commentaries. The term sowa rigpa is not present in these works, with authors and publishers opting instead to identify these works simply with Tibetanness: Tibetan Medical Paintings (Parfionovitch 1992) and The Tibetan Art of Healing (Baker 1997). Significantly, in the first book, the paintings in question were produced in Lhasa and then taken to Buryatia, as testament to the early and continued transnational reach of this medical tradition. In the other, the thangka paintings were repainted by a prominent Nepali artist and the practice was reframed around ‘art’ instead of ‘science’, and, given the preface by Deepak Chopra, the book seems to be indicative of an increasing cosmopolitan interest in Asian medicines as antidotes for modernity’s ills (see Langford 2002). But the term ‘art’ might have also been an expedient and literal choice since the book did feature paintings made by artists (albeit also originally made for the purpose of medical memorization and as symbols of political prestige presented to the Fifth Dalai Lama). Perhaps this is an indication that earlier uses of the term ‘art’, which are literally focusing on artistic expressions of medical knowledge, set the stage for later turns toward discussions about ideas of skill: seeing both the art and science within the embodied practice. In contrast, the first contemporary printing in China of the medical thangka plates was given the English title Tibetan Medical Thangka of the Four Medical Tantras (Jampa Trinlé et al. 1987).
So, the latter half of the twentieth century witnessed a shift in some instances toward the qualification of Sowa Rigpa as expressly Tibetan or in the use of the term ‘Tibetan medicine’ instead of the term Sowa Rigpa, further qualified in ways that delineated clearly nationalist agendas. And yet while this worked, in a sense, for both Chinese and exiled Tibetan communities, it did not represent the full spectrum of practice and claims to belonging that this diverse system of scholarly Asian medicine encompasses. Beginning in the late 1970s in India, and picking up momentum in the 1990s, there became a growing and vocal recognition among practitioners of this medical system who were notTibetan – namely Nepalis, Ladakhis, Bhutanese, Mongolians, and others – that the term ‘Tibetan medicine’ had political consequences for them. This occurred during a time marked by radical shifts in politics and civil society across Asia, from the breakup of the Soviet Union and political revolution in Nepal, to the beginnings of democracy in Bhutan and a new era of ‘reform and opening up’ in the PRC. This shift speaks to what Connerton (2011, 33–35) has called ‘an ethics of memory at the end of the twentieth century’ and to what he calls the forms of ‘prescriptive forgetting’ that allow for the ‘shared amnesia’ of particular nation-state formations. Whether expressed in the politics of titling publications or in the politics of naming institutions, what to call this practice and its associated corpus of medical texts became contentious in the sphere of regional and national identity. It is to these issues that we now turn.
The terrain of Sowa Rigpa recognition across Asia
As our colleagues Stephan Kloos (2013, this issue) and Calum Blaikie (2013, this issue) have documented extensively, in the late twentieth and early twenty-first century, much debate occurred among exiled Tibetan and Ladakhi practitioners in India, as they were fighting for official recognition of their medical science by the Indian government. Should this system be called ‘Tibetan medicine’ or should it be called ‘Sowa Rigpa’? Most Tibetans in exile argued for the former, in great part because they were loath to lose the ‘Tibetanness’ inherent in this practice, given the importance of claiming Tibetan identity for the diasporic community and also acknowledging that the core texts and, with them, epistemological orientations toward practice,emerged from Tibetan regions in what is today China. The Ladakhis, however, pointed out that such a designation excluded them, if not in practice, then through the politics of naming. Competing and eventually complementary efforts at gaining legal recognition ensued for the better part of two decades. The Ladakhis pushed for recognition by the Indian government by identifying Sowa Rigpa as a ‘lost’ form of Ayurveda, knowing that the textual basis for their work emerged from treatises written in Tibet, by Tibetans. Eventually, official recognition by the Indian government in 2010 was for Sowa Rigpa, not Tibetan Sowa Rigpa or Tibetan medicine. Sowa Rigpa has since been incorporated into India’s Department of AYUSH (Ayurveda, Yoga, Unani, Siddha, and Homeopathy) previously within the Ministry of Health and Family Welfare, and since 2014 a ministry in its own right. Notably, there are some ongoing debates about whether an additional ‘S’ should be added to AYUSH to account for Sowa Rigpa (Dastidar 2015). These changes also affected the naming of degrees and departments, such as at the Central University of Tibetan Studies, which was officially renamed the Department of Sowa Rigpa. As one of the teachers explained:
In 1993, we called our department ‘Tibetan Medicine Department’ [or] Bhat Chikitsia Vidhya. After recognition in 2010, we changed it to ‘Department of Sowa Rigpa’. We also changed the names of the degrees around 2011/12. What used to be called ‘Bachelor of Tibetan Medicine and Surgery (BTMS)’ is now called ‘Bachelor of Sowa Rigpa Medicine and Surgery (BSRMS)’. These decisions were made based on internal discussions. (pers. comm. with Gerke, March 2015)
A similar renaming occurred in Ladakh, where the AYUSH-sponsored office, first known as the Amchi Research Unit, became the Sowa Rigpa Research Centre and is now the National Research Institute for Sowa Rigpa. At the same time there was a renewed focus on popular English-language literature on Tibetan medicine, such as the late Dr. Pema Dorjee’s Tibetan Healing Science: Bod Kyi Sowa Rigpa (2009). The title of this text, written in English with Eleanor Lincoln Morse, clearly not only claims Sowa Rigpa as distinctly Tibetan but also reinforces the notion that it is a ‘science’. Unfortunately, we could not ask Pema Dorjee directly about his involvement in the choice of the title, but considering that he was a practitioner and produced scholarly publications in English and Tibetan, the use of the term ‘science’ by Tibetan writers like him would be a good area of further inquiry.[note 10]
For exiled Tibetans in India, the inclusion of what they do under the name Sowa Rigpa within AYUSH has created a new platform for policy making and political lobbying, including emergent concerns about intellectual property rights (Pordié 2008) and sensibilities pointing toward Sowa Rigpa as ‘intangible cultural heritage’. AYUSH has shifted away from earlier identifications of this tradition with the term ‘amchi medicine’ – itself a testament to early and consistent lobbying by elite Ladakhi practitioners and with which exiled Tibetans were very unhappy – toward Sowa Rigpa, which exiled Tibetans see as an improvement if not an ideal. And yet there remain mixed feelings about the official designation being Sowa Rigpa – with no visible marker of Tibetanness.
Yet when one examines how these terms are represented in different forums, including institutional websites in India, we see illustrations of national and regional identity resurfacing: The Central Council of Tibetan Medicine, established in Dharamsala in 2004 as a group representing all Sowa Rigpa medical practitioners in exile (but registering also Sowa Rigpa practitioners in Europe and the USA), described (at least until 2014) this practice – in Tibetan language – as: ‘the medical assembly of Tibetan Sowa Rigpa of the Tibetan refugees’ (btsan byol bod mi’i bod kyi gso ba rig pa’i sman pa’i lhan tshogs) (Central Council of Tibetan Studies 2013). In contrast, the Ladakh Society of Traditional Medicine still uses the term ‘amchi medicine’ as well as Sowa Rigpa (Nomad RSI). Here we can see in practice what Qusar meant when he called Sowa Rigpa a ‘political-technical term’. It is perceived by some as needed spaces of bureaucracy but not necessarily how they would identify themselves as practitioners. Quite contrary to a Tibetan physician at the Central Institute of Tibetan Studies (quoted extensively below), who calls himself ‘a lifelong student of Sowa Rigpa’, Qusar explained: ‘I am a Tibetan doctor not a Sowa Rigpa practitioner’.
Yet for many practitioners, calling oneself a ‘Tibetan doctor’ remains untenable in national contexts. In the case of Nepal, the term ‘Tibetan Medicine’ remains politically problematic; the alternative, ‘Nepal Himalayan Amchi Medicine’ (ne pal hi ma la ya’i am ji gso rig) is not only unwieldy but also has problems of translatability. As Tenzin Bista put it, ‘When we say “amchi” people from the government or even other Nepali people do not know what this means. They think it is like a jankri [Nepali term for ‘shaman’] or some other thing that is not scientific, that does not have a long and deep history’. For Bista and others like him, the possibilities afforded by a shift from calling what they do ‘amchi medicine’ to calling it ‘Sowa Rigpa’ brings a greater sense of authority, now reinforced by the 2010 decision to recognize Sowa Rigpa as an Indian system of medicine. Nepali practitioners understand the translation of this term as ‘science of healing’ as additionally useful because it lends their work a sense of legitimacy and value as part of an ideology of science, reinforcing neat parallels with the ways that nationally recognized Ayurveda is often translated as the ‘science of life’. Perhaps we can recognize here how ‘foreign’ terms underline a certain authority of naming, such as in Sangye Gyatso’s (1982b, 20/6) quote above, where he introduced the ‘science of healing’ (gso ba rig pa) as a translation of the Sanskrit cikitsā vidyā.
Nepali amchi’sattempts to lobby for official government recognition and financial support for education and clinical practice has been only marginally successful over the past fifteen years, the reasons for which are complex, wrapped up both in personal politics and the country’s massive political transitions during this same period (Craig 2008, 2012). However, it is significant that, after all this time, they are now considering shifting their national organizational identity away from the Himalayan Amchi Association (HAA) toward the creation of a Nepal Sowa Rigpa Council. Prospects for accomplishing such a shift remain complicated, bound up in their reading of ethnic, cultural, and religious rights as framed in Nepal’s new and controversial constitution. However, the fact that the country’s leading representatives of this medical practice are now considering such a name change is significant. Dr. Gyatso Bista, a former chairman of the HAA put it this way, ‘Now it seems that “amchi” is too complicated, “Tibetan medicine” is too political, and “Sowa Rigpa” is becoming the most famous term’ (pers. comm. with Craig, October 2015). Corresponding to this sentiment, we have noticed in discussion with colleagues that in some ethnographic contexts – for example in Ladakh and Nepal – amchi have actually begun referring to Sowa Rigpa in colloquial speech with patients, a discursive shift away from calling what they do ‘amchi medicine’, ‘bömen’,or just ‘medicine’ (men). To our knowledge, however, this same phenomenon has not occurred within Tibetan areas in China, where the primary colloquial description remains ‘bömen’in contrast with ‘gyamen’,by which they mean Chinese-style biomedicine (M. Schrempf, e-mail message to authors, July 2016).
In neighboring Bhutan, representatives of this medical practice have historically favored designations such as ‘Buddhist medicine’ or ‘Traditional Bhutanese medicine’ (Wangchuk, Wangchuk, and Aagaard-Hansen 2007). For example, their Faculty of Traditional Medicine has been labeled ‘Buddhist’ Sowa Rigpa (nang pa’i gso rig)in Tibetan script, concurrent in this instance with the principal national language, Dzongkha. But this too may be changing. Similarly, Mongolia has taken a rather straightforward nationalist approach and simply labeled this practice ‘Traditional Mongolian Medicine’. Further north, in Buryatia and Siberia, practitioners prefer the Russian term for Tibetan medicine, ‘tibetská medicína’; the Buryat-trained Aleksej Zasuhin titled his recent book Modern Tibetan Medicine (2015) and explains that practitioners in Buryatia and Russia are aware of the term sowa rigpa – which they translate as ‘healing arts’ (целительства) or ‘knowledge of healing’ (знание исцеления), but that they prefer the term ‘tibetská medicína’ (тибетскаямедицина) since they have no issues with the politics attached to naming the medical practice ‘Tibetan’ (pers. comm. with Gerke, November 2015). These varied ways of naming a medical tradition speak of both a nationalistic appropriation of medical knowledge (as in Bhutan and Mongolia) as well as an appreciation of a medical tradition that gets firmly linked to Tibet from an outside perspective (as in Russia), a point that is also highlighted in our conversations with Qusar.
Apart from this exception, we can see evidence of the ways that Sowa Rigpa is becoming an internationally recognized term. One example of this is that representatives of Bhutanese Sowa Rigpa institutions as well as some Ladakhi amchi in India have expressed modest interest in participating in the creation of a multinational file for the recognition of, yes, Sowa Rigpa as Intangible Cultural Heritage (ICH) within the UNESCO framework (M. Schrempf, e-mail message to authors, July 2016). While the status of this bid for multilateral ICH remains unclear at present, this idea was initially developed in response to news that the Chinese Ministry of Culture was preparing a national ICH file to recognize ‘China’s Tibetan Medicine’. This is part of a broader move propagated by Chinese media to register several Tibetan cultural practices as ICH (Zhu 2015).
Despite these movements in favor of Sowa Rigpa as a stand-alone name, it is important to note that it is not just exiled Tibetans who would like to reinsert the word ‘Tibetan’ into Sowa Rigpa. Cuomo, who was trained in Lhasa and who practices today in Europe and China, thinks it is important to acknowledge the root of the medical tradition by using the term ‘Böki Sowa Rigpa’, thus highlighting her strong affiliation to a particular regional tradition that is based on a long lineage:
Sowa Rigpa itself still needs the [term] ‘Tibetan’. In the past, Tibet was quite an isolated country… . There was no need to emphasize that it is from Tibet. But now it is different… . If the culture comes from India, we always quote it and name it ‘gyagar kédu’ [rgya gar skad du, lit. ‘in Indian language’]. It is an appreciation and scholarly precise. Likewise Tibetan Sowa Rigpa. If you say ‘Sowa Rigpa’, you have to keep the BökiSowa Rikpa, because this is the origin.
While this comment is true in one sense, based on our review of medical text titles, it privileges textual recognition of identity over regional practices, and it is not always or exclusively true, just as Sowa Rigpa does not become distinctively ‘Tibetan’ in these Tibetan language sources until the twentieth century. Cuomo’s comments parallel developments in contemporary Tibetan medicine as practiced in the exile community in India. Qusar has said, ‘It is important to keep the “Tibetan” for us’. He went on to describe concerns about authorship, stating that the entire corpus of medical literature is written by Tibetans and that the written wealth of the tradition has been upheld by Tibetans for a long time. Even so, there remains, he acknowledged, a long history of inviting ‘outside influences’ into the field of theory, pharmacology, and clinical practice.
The Men-Tsee-Khang is the largest institute of Sowa Rigpa in India, founded in Dharamsala in 1961. It has extensive training, research, pharmacy, and clinical facilities (see Kloos 2010 on its history). While for physicians trained at Men-Tsee-Khang in India, the national identity of being Tibetan and practicing ‘Tibetan medicine’ is closely linked, Tibetan medical practitioners at the Central Institute of Tibetan Studies in Sarnath seemed more open to adopting Sowa Rigpa as a broader, more inclusive term. One of the physicians explained this during an informal discussion:
I do not use the translation of Sowa Rigpa, like Tibetan medicine or Buddhist medicine. There is no Hindu Ayurveda or Greek Unani. Ayurveda is Ayurveda and Sowa Rigpa is Sowa Rigpa… . There is no need to add Böki[to] Sowa Rigpa. In Nepal they call it ‘Amchi Sowa Rigpa’, in Bhutan ‘Buddhist Sowa Rigpa’. Sowa Rigpa is such vast knowledge, you can leave it as it is. Leave it big as Sowa Rigpa, so you can explore it. If you add words, you narrow it down… . So, I do not call myself a Tibetan doctor, I am a lifelong student of Sowa Rigpa. Sowa Rigpa can be explored in all the localities where it is practiced. If you use Buddhist Sowa Rigpa, Christian or Muslim patients might have a doubt about taking the medicine or consulting a doctor. Why limit ourselves? The Four Treatises is clearly a Tibetan book. We do not have to proclaim it since it is obvious to everyone who studies it. (pers. comm. with Gerke, March 2015)
Tenzin Bista, speaking as a Nepali citizen, generally agreed with this, adding, ‘Ultimately, it is less important what we call it. It is more important what we do’. Even so, he and other Nepali practitioners support the idea that ‘Tibetan medicine’ is both politically problematic and too narrow. Nepali amchi feel the pressure of Nepal’s geopolitical positioning vis-à-vis China, and the strong repression that can be leveled by the Nepali state against practices labeled as ‘Tibetan’ as well as people, acts or institutions perceived as challenging the ‘One-China’ policy. Finally, such amchi also resist the idea that their legitimacy as practitioners needs to be defined either by Tibetan government-in-exile institutions or Tibetan institutions within China. As is the case with Ladakhi practitioners, this marginalizes or negates local and regional expertise, histories, and forms of sowa rigpa practice.
In the past, not only geopolitics but also the heterogeneity of origins, diversity of practices, and variety of regional languages – despite an overlapping textual corpus and shared theoretical frameworks for understanding health and disease – have made it difficult for practitioners from across Asia to work together. Today, Sowa Rigpa is being viewed as an affective, unifying term that has the potential to allow practitioners to at once assemble around an explicitly extra- or multinational framework of identity and to retain their diverse and more localized subjectivities. A meeting during the Eighth International Congress on Traditional Asian Medicine in Korea in 2013 exemplified such possibilities. Individuals from India, Nepal, Bhutan, Mongolia, and Tibetan regions of China explicitly assembled under the umbrella of a ‘Sowa Rigpa Group’ within the International Association for the Study of Traditional Asian Medicine (IASTAM). This group was at one point called ‘Himalayan Desk’, but the name ‘Sowa Rigpa Group’ prevailed in the end, in part because Sowa Rigpa felt more inclusive and encompassing than defining the group with a geographical term. Again recalling Shneiderman’s work on the situated formation and assertion of Thangmi ethnicity (2015), here too Sowa Rigpa is being evoked through a process that involves both self-representation and the contrast with others, through the deployment of a name made more salient by the presence of foreign scholars and diverse regional scholar-practitioners, all uniting around a common set of interests and concerns. This dynamic is at once illustrative of strategic essentialism, but also more meaningful than this concept connotes.
Although the IASTAM group has been a virtual means of belonging ever since that in-person meeting, the explicit agreement to identify in this way is significant. We see parallels in these developments with Connerton’s discussions of the formation of new identities. He argues that forgetting is part of that process ‘by which newly shared memories are constructed because a new set of memories is frequently accompanied by a set of tacitly shared silences. Many small acts of forgetting which these silences help to enable over time are not random but patterned’ (2011, 37). Connerton applies this to ethnographic examples in which ancestors and kin relationships are ‘forgotten’ in the formation of new identities among demographically mobile ethnic groups across islands in the Southeast Asia Sea. Here, remembering shared identities that stretch across cultural and geographic terrain remains important when creating new relatedness. We suggest that similar acts of forgetting and remembering take place as the term ‘Sowa Rigpa’ becomes a discursive space in which practitioners from across the Himalaya and the Tibetan plateau can meet and, in some contexts, lobby for national and transnational recognition and support. And yet the forgetting this requires is an explicit de-emphasis of the term ‘Tibetan’, which continues to be felt as a form of ‘repressive erasure’ (Connerton 2011, 41) by some (especially Central Tibetans and those living in diaspora) and a move toward more inclusiveness by others (such as Ladakhi or Nepali practitioners).
It is also important to acknowledge the role that scholars of this medical practice – including ourselves – have played in facilitating this politics of naming. During our discussions with him, Qusar incisively noted: ‘Only when foreigners started looking at Tibetan medicine did they begin calling it bömen, i.e. “Tibetan medicine” or “medicine from Tibet’’’. This usage began early on, perhaps well before what Qusar is referencing here, as, in our conversation, Qusar also maintained that Russia used the term ‘bod sman’ or ‘tibetská medicína’ first, and without what he called ‘political inhibitions’, because Russia was not caught up in the political dilemmas of naming Tibetan medicine present in India or Nepal. While this might be true for Russian encounters with the ‘science of healing’ as practiced across the Tibetan Plateau and greater Himalaya, other Western scholarship has helped to create this discursive shift, making Sowa Rigpa a synonym for ‘Tibetan medicine’ or ‘amchi medicine’ when working in places like Nepal or Ladakh, and sometimes qualifying Sowa Rigpa as a ‘classical’ term.
For example, our colleague Mona Schrempf (2007, 3) writes, ‘The classical definition of Tibetan medicine is gso ba rig pa, the “knowledge and practice of healing” or the “science of healing”’. Ladakhi practitioner Dr. Padma Gurmet (2004) does the same in his epigraph at the start of this paper, and in other scholarly work. What is interesting here, of course, is the sort of ‘forgetting’ such assertions require. As we have shown, ‘Sowa Rigpa’ as a synonymfor ‘Tibetan medicine’ is a decidedly modern, rather than a classical, phenomenon. Geoffrey Samuel describes Sowa Rigpa as ‘the medical tradition of culturally Tibetan regions’ (2013, 336). Leaving aside whether or not Mongolia or Bhutan classify as such, this designation is at once accurate and yet could also be seen to privilege Tibetanness over greater Himalayan and Central Asian knowledge, expression, and adaptation of shared origin stories, moral frameworks, and theories of health and disease.
In the introduction to Medicine between Science and Religion, Vincanne Adams, Mona Schrempf, and Sienna Craig (2010, 3–10) describe a thread running through diverse practices as a ‘sowa rigpa sensibility’. This term was the authors’ attempt to recognize something beyond a shared corpus of texts, many of which could be characterized as decidedly Tibetan, toward a sense of collectively claimed skills and embodied practices that align with these textual traditions but are also shaped by local histories, institutions, and ecologies. While this work did not overtly avoid the word ‘Tibetan’, it also represented efforts to describe diverse ethnographic realities and, at the same time, to intervene into how we think about how communities’ relationships to biomedicine, science, and Buddhism. Since Adams, Schrempf, and Craig do not work in India as a primary field site, their introduction perhaps did not appreciate the extent to which the choice of the term ‘sowa rigpa sensibility’ reflected a politics of recognition occurring simultaneously in the Indian context, even as it did seem a necessary theoretical intervention, something good to think with. In this and other ways, scholarship has facilitated and reinforced a consolidation of identity toward Sowa Rigpa, if not overtly away from Tibetan medicine. Here, identity politics meet academic discourse, reinforcing Hsu’s warnings but also demonstrating that the currents of tradition of which we write are simultaneously local, national, transnational, and global in their dynamics.
Entitlement, territory, and popularization of the vernacular
Scholarship on the healing traditions of Tibet and the Himalaya has expanded exponentially over the past two decades. Popular writings on the topic in North America, Europe, and Asia have kept apace. So have opportunities to study this system and to be treated by its therapies outside of Asia. We cite as examples the export of the Men-Tsee-Khang’s Sorig line of cosmetics, teas, and supplements; the founding of Arura Medicine of Tibet (www.aruramed.org), a Tibetan medicine resource center in Charlottesville, Virginia, with the interesting Tibetan name A ri’i a ru ra bod kyi gso rig lte gnas (lit. American Centre of Arura Tibetan Sorig); and the expansion of clinical care and courses of study through online and in-person venues in Europe and North America. Sowa Rigpa has become a globalizing force – arguably a globally recognized ‘brand’ of Asian medicine. But to what ends? Where does this transition meet practitioners on the ground, in terms of recognition, authority, and support for them to do their work, particularly in Asian contexts?
As a way of posing some answers to these questions, we direct attention to the three main schools of Tibetan medicine in Europe and the United States providing Sowa Rigpa to non-Tibetan audiences. The oldest is the Shang Shung Institute (SSI), founded in 1989 in Italy by the Dzogchen teacher Chögyal Namkhai Norbu, which established its North American branch and the SSI School of Tibetan Medicine in 2005, and since 2012 also has a branch in Russia, offering a four-year Tibetan medicine resident program. The US program is directed by Dr. Phuntsog Wangmo. We note that, as names go, ‘Shang Shung’ itself connotes a sense of ancient and authentic ‘Tibetanness’ not only confined to Buddhism but also referencing Bon. SSI’s School of Tibetan Medicine has been working towards full accreditation and licensure in the United States, while clinical apprenticeships for students are facilitated in Qinghai Province (Amdo), in collaboration with the Qinghai Tibetan Medical Hospital (Craig 2014; Shang Shung Institute).
The main school in Europe, the Tibetan Medicine Education center (TME), was founded in 2006 by the Men-Tsee-Khang-trained physician Pasang Yonten Arya (www.tibetanmedicine-edu.org). Arya’s biography traverses many different regions and sources of influence, from his birth in Kyirong, Central Tibet, to his years as a Tibetan refugee in eastern Nepal, to his study of Tibetan medicine in Dharamsala and Ladakh, through his journey to the West, which began in 1991, through Russia. He now also has longstanding ties to Western Europe, especially Germany, Switzerland, and Italy, where he teaches. Notably, both SSI’s school and TME use the name ‘Tibetan medicine’ in their courses and curriculum, probably arising out of the popularity of all things Tibetan in the 1990s when these institutions were getting started. Neither institution references Sowa Rigpa directly in their online presence. And, in the case of both schools, there is an explicit recognition that the goal of these institutions is to train non-Tibetan (Western) students in Tibetan medical history, theory, and practice. In addition to these two Euro-American institutions, we note the creation of the European Association for Traditional Tibetan Medicine (www.tibet-medicine.org), and the American Tibetan Medical Association (www.americantibetanmedicine.org). Both have chosen to use ‘Tibetan medicine’ as primary identifiers, which attests to a certain continuity of the popularity of ‘Tibetan medicine’ as a trendy label, although both websites also reference Sowa Rigpa as its synonym.
A more recent player on the global platform of Sowa Rigpa is Dr. Nida Chenagtsang. Born and trained in northeastern Tibet (Qinghai Province, China), this physician and nagpa (ngags pa), or tantric household priest, is now firmly established as a European and North American-based player in the globalization of this medical system through his Sorig Institute (gso rig khang) (www.soriginstitute.org). Founded in 2008, this is a branch of the International Academy of Traditional Tibetan Medicine (IATTM), established in 2006 (www.iattm.net). While IATTM still favors the name ‘Traditional Tibetan Medicine’ (TTM), these interconnected institutions describe ‘traditional Tibetan medicine’ as the ‘modern term’ for Sowa Rigpa (Sorig Institute 2015a). In the latest IATTM establishment, opening in 2016, Sowa Rigpa features prominently: the Sowa Rigpa International College in Kathmandu affiliated with Lumbini Buddhist University in Nepal began as of August 2016 to offer an accredited five-and-one-half-year course with a Bachelor of Sowa Rigpa Medicine (BSM) degree as well as an ‘accredited degree program in the Science of Traditional Himalayan and Tibetan Medicine’ (Ngakmang Foundation). Unlike Dr. Wangmo’s program in the United States or Dr. Arya’s program in Europe, Dr. Nida’s effort is aimed at both international and Himalayan-based students, including ‘Traditional Amchis who have learned via oral tradition and have not received a formal education’ (Sowa Rigpa International College Brochure 2016). If conducted successfully this could mean a step towards official recognition of Sowa Rigpa in Nepal.
Chenagtsang describes his choice of name for the TTM Institute as follows: ‘Sorig is the actual name of Tibetan medicine, a combination of the words sowa, translated as “healing” or “nurturing”, and “rigpa” or “awareness”. It is with the guiding principle of “Healing Awareness” that we promote the lineage of Tibetan medicine in the West’ (Sorig Institute 2015b). Here, Sowa Rigpa becomes a hyper-real and truly authentic term for this practice, in part by being yoked to ‘awareness’, itself a term which resonates with cosmopolitan Buddhist sentiment – a synonym for ‘mindfulness’, if you will – in a similar way that ‘science’ is an imperfect and complicated translation of rigpa. These discursive moves mirror the ways that Chenagtsang has been teaching, training, and recruiting international students.
This is not to say that Chenagtsang has distanced himself from Tibetan medicine, either in name or in practice. Indeed, the institute also refers throughout its materials to Traditional Tibetan Medicine as ‘TTM’. This acronym is a correlate with Traditional Chinese Medicine (TCM), which, as scholars have shown (Hsu 2008; Taylor 2005; Scheid 2002), is a ‘political-technical term’, to borrow again from Qusar, that came into existence in the 1950s to serve particular state-building mandates of Maoist China. (As a related point, see Craig 2008 for an example of Nepali amchi leveraging the ambiguity in the acronym ‘TM’, which can stand conveniently either for ‘Traditional Medicine’ or ‘Tibetan Medicine’.) However, Chenagtsang’s institutional goals seem to create a global space for expanded therapeutic possibilities – possibilities that blend ‘medical’ instruction, Buddhist ritual practice, and tourism. These goals may include support for the needs of practitioners working under specific national dynamics of possibility and constraint and for their struggle to gain legal recognition for teaching, practice, and pharmaceutical production, but it is as yet unclear how these two different goals might work together. In part, he has been leveraging the ideaof Sowa Rigpa as something that cannot be claimed by one nation state. At the same time, these moves impact those practicing within particular national contexts.
As we have observed at various conferences, through ethnographic encounters with people involved in and affected by the Sorig Institute, and through a reading of the institute’s web presence, the institute’s emphasis seems to be both on promoting recognizable forms of medical education across the Himalayan and Tibetan regions, and on educating Westerners into Tibetan medical practice. The Sorig Institute offers both in-person and online English-language teachings on Tibetan therapeutics, including medicine and kunye massage, as well as Buddhist instruction for European and North American clientele. While a primary focus of these forms of instruction is the Yuthog Nyingthig, a seminal Tibetan medical text for the ritual empowerment of medicines (see Blaikie et al. 2015; Garrett 2009), other courses include ‘dream studies’, ‘mantra healing’, and introductory Tibetan language classes. The institute produces a newsletter, has hosted international congresses in Asia and Europe, and organizes forms of medical ‘study tours’ to culturally Tibetan regions of China. As detailed on their website, the recently established formal relationship with Lumbini University in Nepal as the Sowa Rigpa International College has a mission of ‘preserving the living spiritual, medical, and cultural traditions of the Tibetan and Himalayan regions’. But these combined goals are complex, not only from regulatory and sociolinguistic standpoints, but also with respect to the economic accessibility of such a diverse potential student body.
Nepal does not officially recognize or support the work of their own amchi citizens; the highest level of formal training recognized by the Ministry of Education is the kanjenpa degree, equivalent to a Community Medical Assistant within the organizational structure of the Ministry of Health and Population. It is clear from publicly available documents that the Sowa Rigpa International College hopes to attract both Nepali nationals and culturally Tibetan individuals as well as international students. The teachers at the college include Nepali nationals as well as Tibetan practitioners in exile, and at least one individual each from Sikkim and Bhutan. It is notable, however, that the institute has chosen Sowa Rigpa over Tibetan medicine as a primary descriptor for what students will learn and what they will apparently be certified to practice. It is also notable that an individual born and trained in China’s Tibet has been able to set up such a project in Nepal. Arguably, this same venture would not easily happen in either China or India, given the politics of Tibetan religious and cultural expression on the one hand, and the designation of Sowa Rigpa as an Indian system of medicine, with robust regulatory frameworks, on the other. This project is being further implemented by another spinoff organization, Sorig Khang International Nepal (with the unfortunate acronym SKIN), in which one Nepali amchi and several Tibetan doctors who make their home in Nepal are involved, as well as prominent Nepali scholars of, principally, Newari Buddhism who have helped to establish Lumbini University.
In speaking recently with some Nepali amchi about the activities undertaken by the Sorig Institute over the past few years, it has become clear that a significant number of them feel Chenagtsang’s vision does not include them, or that it is benefitting institutionally trained ‘elite’ amchi in Nepal over lineage-based practitioners. At a recent international congress organized by IATTM and held at the end of 2014 in Kathmandu, local representatives of the HAA were asked to pay significant registration fees to attend and were not included in the planning or organization of the event. This lack of recognition for the work the HAA has undertaken over the past two decades, albeit imperfectly and with attention divided between their own rural lives seeing patients and making medicines along with their more cosmopolitan and national ambitions, was interpreted by some as the form of forgetting Connerton (2011) calls ‘humiliated silence’, coupled with what he calls the forgetting of ‘annulment’. In this case, humiliated silence occurs through overt actions that illustrate the power of a global figure’s charisma and connections over the need to acknowledge or include the voices of those who are struggling to keep their practice alive in local and national contexts; annulment occurs through the global assemblage of knowledge about this practice, such that the differences between Sowa Rigpa and Tibetan medicine seem insignificant and the goals of ‘preserving the living spiritual, medical, and cultural traditions of the Tibetan and Himalayan regions’ seem shared, even if they are not.
Indeed, the only way that some Nepali amchi see Chenagtsang’s work as potentially beneficial is through the possibility that the Sorig Institute may help to financially support local practice, but this possibility also seems slim. When asked about the founding of the bachelor’s program, one Nepali amchi said, ‘Making a program for foreigners to learn about our medicine has limited benefit. It will not help to convince the Ministry of Health to support our students or to make salaries for them to work in the government health system’. This amchi did not see the college as a viable place to send the young people he is training through a kanjenpa program, for example, although other Nepali amchi hope that the new Sowa Rigpa International College may provide a place for a new generation of Nepalis and Tibetans living in Nepal to be trained as amchi – so long as they can afford the tuition fees. The core goal of seeing medical education parlay into employment as a doctor has been accomplished among amchi in Ladakh and, in different ways, throughout Tibetan regions of China, Bhutan, as well as in Mongolia and Buryatia. Such support for rural practice and the provision of health care to Himalayan and Tibetan communities remains an ethical and professional goal for many practitioners, young and old, but it is also an especially important framework within which claims for state support are made by Himalayan practitioners (see Blaikie, this volume). This raises further questions about to what ends and for whom Sowa Rigpa is practiced today.
Significantly, we note that the Men-Tsee-Khang in Dharamsala has begun a program to train what they are calling ‘Sowa Rigpa therapists’ – people who receive six months of instruction and are then sent to work in spas, primarily serving an Indian upper-class clientele (Men-Tsee-Khang). Other young amchi from Nepal are struggling to find employment in similar settings, even after more than a decade of training. Is Sowa Rigpa the name of a medical system or a ‘lifestyle practice’? What does the excision of the term ‘medicine’ in favor of the term ‘Sowa Rigpa’ accomplish? What constitutes enskillment, and who arbitrates this? In the globally appealing and seemingly inclusive turns toward Sowa Rigpa, what is forgotten?
Conclusion
In this article, we have described and analyzed the naming practices that have allowed sowa rigpa to evolve from a linguistically Tibetan way of describing allsystems of medicine to a shared if still-contested term to describe a system of maintaining health and addressing disease within and across national borders in Asia, and then again to a marker of national, transnational, and de-territorialized identity. Today we might also acknowledge Sowa Rigpa as a brand, one that is capable of going global, but that also runs the risk of further marginalizing local practitioners and glossing over serious issues regarding the cultural ownership of knowledge.
Our examination of the etymological roots and transfigurations of this term – in titles of Tibetan medical texts, selected quotes, the self-representation of contemporary institutions, and the words of practitioners themselves – reveals that the popularization of a vernacular term can have many purposes. This has been the case in other Asian medical systems, such as Japanese and traditional Korean medicine (Hsu 2013). In this sense, what we chart here for Sowa Rigpa is not unique, but it plays out in specific ways because of the political contexts, at once virtual and territorially bound, in which Sowa Rigpa practitioners find themselves. This leads to further questions: To what does naming entitle you? Who has the authority to name? Using Connerton’s (2009, 2011) work as a theoretical grounding point, we have explored the forms of ‘forgetting’ that transform the meaning of a name over time, toward distinctly contemporary goals. Based on the examples presented here we see that the term ‘Tibetan’ is often ‘forgotten’ in countries or by groups of practitioners where the label is of political disadvantage, in order to achieve contemporary global goals for Sowa Rigpa across national borders.
Within these sociocultural and geopolitical parameters, this article has begun to explore the implications of a profound yet subtle sociolinguistic development. The term sowa rigpa as used in spoken or written Tibetan language has come to stand in for the label ‘Tibetan medicine’, particularly when it is employed in English or other non-Tibetan language contexts. In some instances, it has also become a preferred marker of this medical practice, over the term ‘Tibetan medicine’. Both new uses – for example in Euro-American contexts or among Nepali amchi speaking about what they do and who they are – can be at once productive, necessary, and exclusionary.
We are bearing witness to a process by which the term sowa rigpa (as a science of healing or medical practice) has attracted a very specific meaning, becoming Sowa Rigpa as a nationally and internationally recognized ‘system’ of medicine. Sowa Rigpa exists as an official designation for eclectic currents of tradition that it once embraced and resisted. What might it mean that Sowa Rigpa has become for many practitioners from India, China, Nepal, Bhutan, and Mongolia as well as in global diasporic contexts, the universally agreeable term to label what they do and what they want to support and protect, despite its inadequacies? What does choosing notto translate but instead rely on the global popularization of a vernacular term accomplish? What does it disregard? We conclude that in letting Sowa Rigpa stand for itself, rooted in a Tibetan epistemological framework of sowa rigpa, it comes to stand for something broader than ‘Tibetan medicine’ in a way that creates connections and possibilities for collaboration between practitioners. But, in that process, it might risk shifting authority over the future of this practice to those far from the front lines of caring for people across the greater Himalayan and Tibetan region to those for whom the stakes involved in accessing this medical system are more diffuse and less grounded in place.
Acknowledgements
Sienna Craig’s research and writing of this article was supported by grants from the Clare Garber Goodman Fund, Department of Anthropology, and the Office of the Provost, Dartmouth College. Barbara Gerke’s research and writing of this article was supported by the German Research Foundation, grant nos. 53307213 and 55127201 during a postdoc at the Humboldt University of Berlin, and by the Austrian Science Foundation, grant M1870, completed at the University of Vienna.
About the authors
Sienna R. Craig (PhD Cultural Anthropology, Cornell University) is Associate Professor of Anthropology at Dartmouth. She is the author of Healing Elements: Efficacy and the Social Ecologies of Tibetan Medicine (UC Press, 2012) and Horses Like Lightning: A Story of Passage through the Himalaya (Wisdom Publications, 2008). She is the coeditor of several volumes, including Medicine between Science and Religion: Explorations on Tibetan Grounds (Berghahn, 2010) and co-edits HIMALAYA, the Journal of the Association for Nepal and Himalayan Studies (www.himalayajournal.org).
Barbara Gerke (MSc Medical Anthropology and DPhil Social Anthropology, University of Oxford) completed a German Research Foundation-funded postdoctoral project on Tibetan mercury-processing practices (2011–2015) at the Humboldt University of Berlin. She currently holds a two-year, Lise Meitner senior postdoctoral fellowship, funded by the Austrian Science Fund, at the University of Vienna (2015–2017), researching biographies of Tibetan precious pills. She is author of Long Lives and Untimely Deaths:Life-span Concepts and Longevity Practices among Tibetans in the Darjeeling Hills, India (Brill, 2012) and the editor of a special issue of Asian Medicine: Tradition and Modernity (8, no. 1, 2013) on mercury in Ayurveda and Tibetan Medicine.
References
Adams, Vincanne, Mona Schrempf, and Sienna Craig. 2010. Medicine between Science and Religion: Explorations on Tibetan Grounds. Oxford, New York: Berghahn Books.
Adams, Vincanne. 2002. ‘The Sacred in the Scientific: Ambiguous Practices of Science in Tibetan Medicine’. Cultural Anthropology 16, no. 4: 542–75.
Baker, Ian, Romio Shrestha (Illustrator), and Deepak Chopra (Preface). 1997. The Tibetan Art of Healing. San Francisco: Chronicle Books.
Blaikie, Calum. 2016. ‘Positioning Sowa Rigpa in India: Coalition and Fracture in the Quest for Recognition’. Medicine Anthropology Theory 3, no. 2: 50–86.
Blaikie, Calum, Sienna Craig, Gerke B., and T. Hofer. 2015. ‘Co-Producing Efficacious Medicines: Collaborative Event Ethnography with Himalayan and Tibetan Sowa Rigpa Practitioners’. Current Anthropology 56, no. 2: 178–205. http://dx.doi.org.10.1086/680464.
Central Council of Tibetan Studies. 2013. Btsan byol bod mi’i bod kyi gso ba rig pa’i sman pa’i lhan chogs kyi khrims yig. Accessed 8 December 2015.http://tibmedcouncil.org/wp-content/uploads/2015/01/legal-code-2014.pdf.
Clark, Barry. 1995. The Quintessence Tantras of Tibetan Medicine. Ithaca, NY: Snow Lion Publications.
Clifford, Terry. 1984. Tibetan Buddhist Medicine and Psychiatry: The Diamond Healing. Wellingborough: Aquarian.
Connerton, Paul. 2009. How Modernity Forgets. Cambridge: Cambridge University Press.
Connerton, Paul. 2011. The Spirit of Mourning: History, Memory, and the Body. Cambridge: Cambridge University Press.
Craig, Sienna. 2008. ‘Place and Professionalization: Navigating Amchi Identity in Nepal’. In The World of Tibetan Medicine: Contemporary Trends in the Politics of Medical Knowledge and Practice, edited by Laurent Pordié, 62–90. London: Routledge.
Craig, Sienna. 2012. Healing Elements: Efficacy and the Social Ecologies of Tibetan Medicine. Berkeley: University of California Press.
Craig, Sienna. 2014. ‘Tibetan Medicine in the World: Local Scenes, Global Transformations’. In Bodies in Balance: The Art of Tibetan Medicine, edited by Theresia Hofer, 110–25. Seattle: University of Washington Press.
Dastidar, Avishek G. 2015. ‘AAYUSH or AYUSSH? AYUSH Minister to Consider’. The Indian Express, 19 December. Accessed 3 June 2016. http://indianexpress.com/article/india/politics/aayush-or-ayussh-ayush-minister-to-consider/.
Donden, Yeshi, and Jeffrey Hopkins. 1986. Health through Balance: An Introduction to Tibetan Medicine. 1st ed. Ithaca, NY: Snow Lion Publications.
Dorjee, Pema, with Eleanor Lincoln Morse. 2009. Tibetan Healing Science: Bod Kyi Sowa Rigpa. Charleston, SC: CreateSpace Independent Publishing Platform.
Drakpa Gyaltsen (Grags pa rgyal mtshan, 1147–1216). 1993. Gso Dpyad Rgyal Po’i Dkor Mdzod. Lankru’u: Kan su’u mi rigs dpe skrun khang.
Drikung Chökyi Drakpa (’Bri gung Chos kyi grags pa, 1595–1659). 1999. ’Bri Gung Gso Rig Gces Bsdus. Pe cin: Mi Rigs Dpe Skrun Khang.
Fjeld, Heidi, and Theresia Hofer. 2010-11. ‘Women and Gender in Tibetan Medicine’. Asian Medicine: Tradition and Modernity 6, no. 2: 175–216. http://dx.doi.org.10.1163/15734218-12341234.
Garrett, Frances. 2009. ‘The Alchemy of Accomplishing Medicine (sman sgrub): Situating the Yuthog Heart Essence Ritual Tradition’. Journal of Indian Philosophy 37, no. 3: 207–30.
Gerke, Barbara. 2011. ‘Correlating Biomedical and Tibetan Medical Terms in Amchi Medical Practice’. In Medicine between Science and Religion: Explorations on Tibetan Grounds, edited by Vincanne Adams, Mona Schrempf, and Sienna Craig, 127–52. Oxford: Berghahn Books.
Glover, Denise M. 2006. ‘Tibetan Medicine in Gyalthang’. Tibet Journal 30, no. 4: 31–54.
Glover, Denise M. 2005. ‘Up from the roots: contextualizing medicine plant classifications of Tibetan doctors in Rgyalthang, PRC’. PhD diss., University of Washington.
Gyatso, Janet. 2004. ‘The Authority of Empiricism and the Empiricism of Authority: Medicine and Buddhism in Tibet on the Eve of Modernity’. Comparative Studies of South Asia, Africa and the Middle East 24, no. 2: 83–96.
Gyatso, Janet. 2015. Being Human in a Buddhist World: An Intellectual History of Medicine in Early Modern Tibet. New York: Columbia University Press.
Hofer, Theresia. Forthcoming. Medicine on the Margins: Agency, Memory and Reform in Tibet. Seattle: University of Washington Press.
Hsu, Elisabeth. 2008. ‘The History of Chinese Medicine in the People’s Republic of China and Its Globalization’. East Asian Science, Technology and Society: An International Journal 2: 465–84. http://dx.doi.org.10.1215/s12280-009-9072-y.
Hsu, Elisabeth. 2013. ‘Afterword: On Naming and the Politics of Practice’. In ‘Tibetan Medicine: Contemporary Issues’, ed. Geoffrey Samuel and Colin Millard, special issue, East Asian Science, Technology and Society: An International Journal 7: 505–11. http://dx.doi.org.10.1215/18752160-2371167.
Ingold, Tim. 2000. The Perception of the Environment: Essays on Livelihood, Dwelling, and Skill. London: Routledge.
Ingold, Tim. 2011. Being Alive: Essays in Movement, Knowledge and Description. London and New York: Routledge, 2011.
Jampa Trinlé (Byams pa ’phrin las), Wang Lei, and Cai Jingfeng. 1987. Tibetan Medical Thangka of the Four Medical Tantras. Lha sa: People’s Publishing House of Tibet.
Jampa Trinlé (Byams pa ’phrin las). 1996. Krung Go’i Bod Kyi Gso Ba Rig Pa [China’s Tibetan Medicine]. Pe cin: Krung go’i bod rig pa dpe skrun khang.
Jampa Trinlé (Byams pa ’phrin las). (1990) 2000. Gangs ljongs gso rig bstan pa’i nyin byed rim byon gyi rnam thar phyogs bsgrigs[Namthar of Famous Individuals in the Transmission of the Snowland’s Sowa Rigpa]. Pe cin: Mi rigs dpe skrun khang.
Jampa Trinlé (Byams pa ’phrin las). 2008. Bod Lugs Gso Rig Rgyud Bzhi’i Sman Thang / Tibetan Medical Thangka of the Four Medical Tantras. Translated and compiled by Byams-Pa ’Phrin-Las, Wang Lei (English version translated and annotated by Cai Jingfeng). Lha sa: Bod ljongs mi dmangs dpe skrun khang.
Jampa Trinlé (Byams pa ’phrin las). 2013. China’s Tibetan Medicine. Beijing: Science Press.
Kloos, Stephan. 2010. ‘Tibetan Medicine in Exile: The Ethics, Politics, and Science of Cultural Survival’. PhD diss., University of California San Francisco and Berkeley.
Kloos, Stephan. 2013. ‘How Tibetan Medicine in Exile Became a “Medical System”’. East Asian Science, Technology and Society 7: 1–15. http://dx.doi.org.10.1215/18752160-2333653.
Kloos, Stephan. 2016. ‘The Recognition of Tibetan Medicine in India’. Medicine Anthropology Theory 3, no. 2: 19–49.
Kunchok Gyaltsen, Constance Gewa, Heather Greenlee, Jessica Ravetz, Meredith Aikman, and Anne R. Pebley. 2007. ‘Socioeconomic Status and Maternal Child Health in Rural Tibetan Villages’.Working Paper, California Center for Population Research On-Line.Seattle, WA: Tibetan Healing Fund. http://repositories.cdlib.org/ccpr/olwp/CCPR-Special-07.
Langford, Jean M. 2002. Fluent Bodies: Ayurvedic Remedies for Postcolonial Imbalance. Durham and London: Duke University Press.
Men-Tsee-Khang, trans. 2008. The Basic Tantra and the Explanatory Tantra from the Secret Quintessential Instructions on the Eight Branches of the Ambrosia Essence Tantra. Dharamsala: Men-Tsee-Khang.
Men-Tsee-Khang. 2015. ‘Training and Recruitment for Sowa Rigpa Therapists’. Accessed 10 November. http://www.men-tsee-khang.org/new-news/vana-ad.pdf.
Ngakmang Foundation. 2015. ‘Nepal’. Ngakmang Foundation website. Accessed 18 November. https://ngakmangfoundation.org/nepal/.
Nomad RSI. 2015. ‘Ladakh Society for Traditional Medicine’. Accessed 18 November. http://nomadrsi.org/lstm/?page_id=6.
Padma Gurmet. 2004. ‘Sowa Rigpa: Himalayan Art of Healing’. Indian Journal of Traditional Knowledge 3, no. 2: 212–18.
Parfionovitch, Yuri, Gyurmed Dorje, and Fernand Meyer. 1992. Tibetan Medical Paintings: Illustrations to the Blue Beryl Treatise of Sangye Gyatso (1653–1705). London: Serindia.
Pha khol. 1989. ‘Yan Lag Brgyad Pa’i Snying Po Bsdus Pa’. In Bstan ’Gyur Nang Gig So Ba Rig Pa’i Skor Gyi Dpe Tshogs: Gso Rig Pa’i Rtsa ’Grel Bdam Bsgrigs, edited by Rdo rje rgyal po, 112–756. Pe cin: Mi rigs dpe skrun khang.
Pordié, Laurent and Calum Blaikie. 2014. ‘Knowledge and Skills in Motion: Layers of Tibetan Medical Education in India’. Culture, Medicine and Psychiatry 38, no. 3: 340–68. http://dx.doi.org.10.1007/s11013-014-9389-4.
Pordié, Laurent. 2008. ‘Hijacking Intellectual Property Rights: Identities and Social Power in the Indian Himalayas’. In Tibetan Medicine in the Contemporary World: Global Politics of Medical Knowledge and Practice, edited by Laurent Pordié, 132–59. London: Routledge.
Rangjung Dorje [Karmapa] (Karma pa rang byung rdo rje, 1284–1339). 2006. ‘Sman Gyi Bstan Bcos Dman Ming Rgya Mtsho’. InGsung ’Bum/Rang Byung Rdo Rje. Tibetan Buddhist Resource Center Library W30541. 11: 445–514. Zi ling: Mtshur phu mkhan po lo yag bkra shis.
Samuel, Geoffrey. 2008. ‘The Politics of Tibetan Medicine and the Constitution of an Object of Study: Some Comments’. In Tibetan Medicine in the Contemporary World. Global Politics of Medical Knowledge and Practice, edited by Laurent Pordié, 251–63. London: Routledge.
Samuel, Geoffrey. 2013. ‘Introduction: Medicine and Healing in Tibetan Societies’. East Asian Science, Technology and Society: An International Journal 7, no. 20: 335–51. http://dx.doi.org/10.1215/18752160-2333224.
Sangye Gyatso [Desi] (Sangs rgyas rgya mtsho). 1982a. Gso Ba Rig Pa’i Bstan Bcos Sman Bla’i Dgongs Rgyan Rgyud Bzhi’i Gsal Byed Bai Dur Sngon Po'i Ma Lli Ka. Lha sa: Bod ljongs mi dmangs dpe skrun khang.
Sangye Gyatso [Desi] (Sangs rgyas rgya mtsho). 1982b. Gso Ba Rig Pa’i Khog ’Bugs Vaidurya’i Me Long. New Delhi: Institute of Tibetan Classics.
Sangye Gyatso [Desi] (Sangs rgyas rgya mtsho). 2010. A Mirror of Beryl: Historical Introduction to Tibetan Medicine. Translated by Gavin Kilty. Boston MA: Wisdom Publications.
Saxer, Martin. 2013. Manufacturing Tibetan Medicine: The Creation of an Industry and the Moral Economy of Tibetanness. Oxford, New York: Berghahn Books.
Schaeffer, Kurtis R. 2003. ‘Textual Scholarship, Medical Tradition, and Mahayana Buddhist Ideals in Tibet’. Journal of Indian Philosophy 31: 621–41. http://dx.doi.org/10.1023/A:1026397405584.
Schaeffer, Kurtis R. 2010. ‘Chronological Medical Texts Lists’. Tibetan Medicine Resources. Accessed 4 August 2016. http://tibetanmedicine.chass.utoronto.ca/chronological-medical-texts-list/.
Schaeffer, Kurtis R. 2011. ‘Forms of Knowledge’. In Forms of Knowledge in Early Modern Asia: Explorations in the Intellectual History of India and Tibet, 1500–1800, edited by Sheldon Pollock, 291–310. Durham, NC: Duke University Press.
Scheid, Volker. 2002. Chinese Medicine in Contemporary China: Plurality and Synthesis. Durham and London: Duke University Press.
Scheid, Volker. 2007. Currents of Tradition in Chinese Medicine 1926–2006. London: Eastland Press.
Schrempf, Mona. 2007. ‘Refocusing on Tibetan Medicine’. In Soundings in Tibetan Medicine. Anthropological and Historical Perspectives. Proceedings of the 10th Seminar of the International Association for Tibetan Studies (IATS) Oxford 2003, edited by M. Schrempf, 1–6. Leiden: Brill.
Shan, Zhu 2015. ‘Tibet: four level intangible cultural heritage system’. China Tibet News, 17 September. http://english.chinatibetnews.com/wh/whtp/201509/t20150917_816753.html, accessed 4 August 2016.
Shang Shung Institute. 2016. ‘History of the [Shang Shung Institute] School [of Tibetan Medicine]’. Accessed 3 August. http://www.tibetanmedicineschool.org/history/.
Shneiderman, Sara. 2015. Rituals of Ethnicity: Thangmi Identities between Nepal and India. Philadelphia: University of Pennsylvania Press.
Sorig Institute 2015a. ‘Curricula’. Accessed 10 November. http://www.soriginstitute.org/classes/tibetan-medicine-program.
Sorig Institute 2015b. ‘About Sorig Institute’. Accessed 10 November. http://www.soriginstitute.org/soriginstitute.
Tashigang, Tashi Y., ed. 1989. Sman Dpyad Zla Ba’i Rgyal Po the Somarajabhaisajyasadhana, an Indian Medical Work by Nagarjuna, in Its Tibetan Translation by Hashang Mahayana and Vairocana; Reproduced from a Set of Prints from the Sde-Dge Blocks from Library of Tashigang. Leh (Jammu and Kashmir): Tashi Y. Tashigang [self-published].
Taylor, Kim. 2005. Chinese Medicine in Early Communist China, 1945–1963: A Medicine of Revolution. London: Psychology Press.
Tenzin Kunsel. 2015. ‘Recognition of Sowa-Rigpa Medicine by the Government of India’. Paper given at the Annual South Asia Meetings, Madison, WI, 24 October 2015.
THL Tibetan to English Translation Tool. 2010. ‘The Tibetan & Himalayan Library’. http://www.thlib.org/reference/dictionaries/tibetan-dictionary/translate.php.
Tibetan Medicine Education Institute. 2016. Homepage. Accessed 5 June. http://www.tibetanmedicine-edu.org/index.php.
Travers, Alice. 2015. ‘Between Private and Public Initiatives? Private Schools in Pre-1951 Tibet’. HIMALAYA 35, no. 2: 118–35.
Van Schaik, Sam. 2011. Tibet: A History. New Haven, CT: Yale University Press.
Wangchuk, Phurpa, Dorji Wangchuk, and Jens Aagaard-Hansen. 2007. ‘Traditional Bhutanese Medicine (Gso-Ba Rig-Pa): An Integrated Part of the Formal Health Care Services’. The Southeast Asian Journal for Tropical Medicine and Public Health 38, no. 1: 161–67.
Yan, Zhen, and Cai Jingfeng. 2005. China’s Tibetan Medicine. Beijing: Foreign Language Press.
Yuthog Yönten Gonpo (G.yu thog yon tan mgon po). 1967. Cha Lag Bco Brgyad Sarnath, India: Sar na tha’i legs bshad gter mdzod khang.
Yuthog Yönten Gonpo (G.yu thog yon tan mgon po). 1982. Bdud Rtsi Snying Po Yan Lag Brgyad Pa Gsang Ba Man Ngag Gi Rgyud. Lha sa: Bod ljongs mi dmangs dpe skrun khang.
Zasuhin, Aleksej. 2015. Moderne Tibetische Medizin. Munich: Knaur.
Endnotes
1 Back
See also translation by Kilty 2010, 86–87.
2 Back
This paper is dedicated to Dr. Pema Dorjee (1950–2015), a medical scholar-practitioner trained at the Men-Tsee-Khang in Dharamsala; former director of the Men-Tsee-khang branch clinics in Kolkata and Salugara, West Bengal, India; and the first chairperson of the Council of Tibetan Medicine in Dharamsala from 2004 to 2007. Dr. Pema Dorjee dedicated his tremendous skills and energy to the cultivation of Tibetan medical knowledge across generations and to the alleviation of human suffering.
3 Back
This is based on an electronic search of the e-text. Since Tibet was not a unified nation for most of its history, one more often finds regional names in the medical literature, such as mnga’ ris, dbus gtsang, and mdo kham. We did not scan the text for those area names.
4 Back
Note that in this brief exercise we limit ourselves to the representations of the terms in the titles, not the analysis and use of the terms in the content of those works.
5 Back
Example: In the King of the Moon (Sman dpyad zla ba’i rgyal po, Tashigang 1989:1/3 and 323/12), usually dated to the eighth to ninth centuries, sorig is part of the name ‘medical treatise’ (gso rig bstan bcos). In the biography of Yönten Gonpo the Elder by Kongpo Derge, Sorig appears in the name of a medical school. Apparently, Sorig Dropeling was a medical college in the tenth/eleventh century (Dr. Pempa, pers. comm. with Gerke, March 2015).
6 Back
Example: bömen appears twice in the text of the Eighteen Implementations ([Cha lag bco brgyad] Yönten Gonpo 1967: 297/10 and 352/27). Sangye Gyatso’s Mirror of Beryl mentions ‘the nine famous Tibetan doctors’ and ‘the other eight Tibetan [doctors]’ (bod sman mkhas pa mi dgu and bod sman gzhan brgyad; Sangye Gyatso 1982b: 174/19, 175/17).
7 Back
Note also the name of the large series Bod kyi gso ba rig paʼi gnaʼ dpe phyogs bsgrigs dpe tshogs, which published more than sixty works through the Nationalities Publishing House in Beijing to date; these are largely edited reprints of classical works.
8 Back
The term ‘treatise’ (bstan bcos), the Tibetan for the Sanskrit ‘shastra’, indicates a general religious commentary in the tradition of the ten sciences described above, but also denotes an exposition, in this case on medicine, and commonly appears in titles of Tibetan works.
9 Back
He used the term sowa rigpa in the title of his two major works on medicine: The Blue Beryl (Sangye Gyatso 1982a, full title: Gso ba rig pa’i bstan bcos sman bla’i dgongs rgyan rgyud bzhi’i gsal byed bai dur sngon po’i ma lli ka) and his classic on medical history, Mirror of Beryl (Sangye Gyatso 1982b, full title: Gso ba rig pa’i khog ’bugs vaidurya’i me long, translated by Kilty, see Sangye Gyatso 2010).
10 Back
We note, for example, that Pasang Yonten Arya published a text in Tibetan in 1988 titled History of Tibetan Medicine (Bod kyi gso ba rig pa’i lo rgyus kyi bang mdzod g.yu thog bla ma dran pa’i pho nya). This book has still not been translated into English or other languages, although he says that this is his ‘favorite’ on his website http://www.tibetanmedicine-edu.org/index.php/publications.