Ordinary medicine
The power and confusion of evidence
—
Abstract
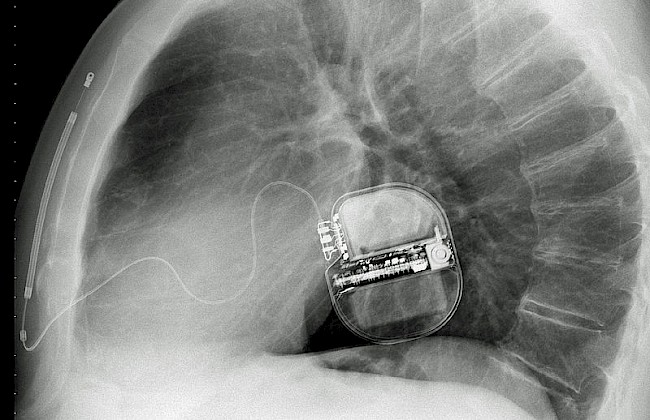
Photo credit: PaulT http://commons.wikimedia.org/wiki/File:Subcutaneous_ICD_XRay.jpg
There is a hidden chain of connections among science, politics, industry, and insurance that organizes evidence making and drives the US health care system. Hidden as well is the ethos that supports those connections and impacts governance.
The multibillion-dollar biomedical research engine, with its emphasis on the clinical trials enterprise, is where evidence making begins. The infrastructure and high value of evidence-based medicine and clinical trials prioritize thinking about what constitutes responsible health care. And they are the dominant apparatuses of truth making in medicine.
How does this work? Trial ‘findings’ are converted into ‘best evidence for treatment’. And then, that evidence generates treatment standards. This is how scientific innovation organizes physicians’ work, health-care finances, and patients’ and families’ expectations about what is normal and needed. The cultural capital of evidence-based medicine, clinical trials, and the standards they set creates a unique quandary in contemporary medicine: When, where, and how to draw the line between too much and enough intervention? And how should one live with the tools medicine offers?
Evidence-based medicine is itself complicated by three interrelated developments that permeate American life, which are inherent in the global biomedical economy and that control the quandary of drawing that line. First, there is the increased role and influence of private industry. In 1980, 32 percent of clinical research was funded by private pharmaceutical, device, and biotechnology companies. Today, 65 percent of biomedical research is funded by private industry, whose goal is always to increase market share. Second, all those clinical trials have generated more evidence of therapeutic value and an ever-increasing number of standard treatment options. Third, the United States’ national priority of new technologies has influenced our collective perspective on the timing of death. Today in the United States, most deaths, regardless of a person’s age, have come to be considered premature.
All of the outcome studies, practice guidelines, and teaching tools within the vast evidence-based medicine matrix have a single goal: to provide a stronger scientific foundation for clinical practice. Yet that ‘scientifically based’ (and especially numerically based) matrix omits the social, nonscientific, and messyfeatures of health care delivery that influence what doctors do and what happens to patients. Consider the following five decidedly nonscientific features:
Physicians sometimes act against their own best judgment and recommend or prescribe interventions despite their known lack of efficacy.
Patients and families ask for treatments that have not been proven to show benefit in studies, and physicians, not infrequently, acquiesce to their requests.
The pharmaceutical and medical device industries are slow to remove drugs and devices from the marketplace that lack benefit (or that prove to be harmful), and doctors may be slow to refuse to use them.
Once a treatment is reimbursed by Medicare, the dynamics of hospital and medical center economics and physician-prescribing patterns make it nearly impossible for all concerned to say ‘no’ to it. Medicare reimbursement thus shapes both standard making and ethical necessity. It becomes the ethics of managing life.
Whether treatments that benefit some carefully selected trial participants will also benefit a more diverse group of patients, especially children and older persons, is always a question and often a troubling one for doctors.
All these factors weave through the framework of what we call evidence-based medicine, shaping the work of health professionals and the practices of patients and families.
So how does evidence-based medicine play out in the clinic and in real lives? I draw from the example of the implantable cardiac defibrillator, the ICD, a little tool like a pacemaker implanted under the skin, designed to correct a potentially fatal heart rhythm. This is a therapy that has shifted from being ‘unthinkable’ a decade ago to being routine and standard for older persons in the United States today. It became thinkable, and doable, when two things happened: evidence from clinical trials showed good survival rates, and Medicare and private insurers began to reimburse for its use.
As devices such as ICDs become smaller and techniques for implanting them become safer, physicians and the public have learned to view them as standard interventions that one does not easily refuse. In the United States these developments produce a sense that life extension is open-ended as long as one treats risk. That is the prevailing, ordinary logic that drives so much treatment. But when do we stop treating risk?
The ICD was used sparingly until 2002 for those who had already survived a potentially lethal heart attack and were at high risk for another life-threatening cardiac event. Then its use began to rise substantially. Why? Nine clinical trials of ICD use were conducted between 2002 and 2005, each one showing varying degrees of benefit among patient populations that had not experienced a potentially life-threatening heart rhythm. Taken together, the findings from those nine trials provided increasing ‘evidence of benefit’ of the ICD for survival, and that evidence led Medicare, in 2005, to expand the eligibility criteria for reimbursement to include primary prevention for those who had never suffered a potentially fatal cardiac rhythm. The floodgates opened.
Now these devices have become the standard of care for patients with moderate to severe heart disease. The important thing about the ICD is that, in treating a potentially lethal arrhythmia, it prevents sudden death (the silent heart attack in the night), the kind of death many say they actually want in late life. Yet the device is difficult to refuse, even in very late life. Why? Because evidence organizes its expanded use, and because it seems to go against medical progress and common sense to say ‘no’ to it. It has become an ordinary part of the medico-socio-ethical landscape. The effects of this logic most affect the oldest patients.
Today, more than 110,000 patients in the United States receive ICDs each year. There is no question of the unequivocal ‘good’ of this device for preventing young people from dying. Yet most people receiving ICDs are older and sicker, with underlying cardiac disease, and the electrical shocks from ICDs do not necessarily extend an older person’s life or improve its quality. Indeed, the ICD transforms the immediate risk of death into the near certainty of progressive heart failure. The hope of this life-extending treatment comes up against a prolonged, unwanted kind of late life and dying.
Consider Sam Tolleson, who, like some other patients with ICDs, endured the pain of the device’s shocks and the knowledge that his debility was being prolonged. At age eighty-eight, when I met him, Mr. Tolleson had been living with cardiac disease for twenty-five years. Tall and thin with piercing blue eyes and a shock of thick white hair, he used oxygen and walked slowly, bent over his walker. He graciously welcomed me to sit down in his apartment and chat. Following a second heart attack at age eighty, he awoke in the hospital and was told that physicians had implanted a pacemaker that included a defibrillator. The physicians were following standard practice, doing what was appropriate both to stabilize his heart rate (the pacemaker) and prevent sudden death from a future heart attack (the ICD). Mr. Tolleson noted that it wasn’t until sometime after getting the defibrillator that he learned what it would do.
About two years before we met, when he was eighty-six, the ICD had begun to shock his potentially lethal cardiac rhythms back to normal. Over a period of several months, Mr. Tolleson was shocked fifteen times. ‘There is no question’, he offered, ‘that those shocks extended my life. It’s very likely that one of those episodes, without the defibrillator, would have been my last’. The first ten shocks were, he reported, ‘spread out, over weeks’. But when he received five shocks in one day, he decided that he had had enough. ‘They were more and more painful. The very thought that I was going to have another one – I couldn’t take it’.
So he made an appointment to have the defibrillator part of the device turned off. This choice is highly unusual. It simply does not occur to most patients or their families that the device, once placed under the skin, can easily be deactivated and that patients can make that choice. Most physicians never discuss that possibility with patients. Mr. Tolleson noted, ‘Both the doctor and the technician [from the device company] were reluctant to turn it off. But I convinced them … and that distressed my family too. The family was very upset with me. I have three children, and they all cried. I had to talk with them about it, and I felt terrible after I talked with them’. He continued, ‘Perhaps I should just have done what they wanted me to do: keep the ICD. But life is getting harder all the time’.
Mr. Tolleson died two days after our conversation.
Scientific evidence, routine reimbursement, standard of care, specialist expertise, industry’s goal to sell devices, and medicine’s mandate to extend life are all strong forces. Mr. Tolleson found himself needing to defend his decision to turn off the defibrillator, both to his family and to the medical staff. He had crossed the line he did not wish to cross.
Since 20 percent of those on the receiving end for the ICD are now over eighty, and the proportion over age ninety is growing (in some places greater than 10 percent) the device is reshaping the aging experience and the transition to death for significant numbers of people. It staves off death but does not improve health. It turns life-threatening disease into a chronic condition enabling people to grow older, in need of more intervention, more risk awareness, and more prevention – all at the same time. This is where evidence has come to rest in the case of the ICD: in the kind of death we are asked to choose, and in a new, uncomfortable engagement with one’s own role in the timing of death.
To conclude: make no mistake, this technology extends wanted life for many people. That is, of course, the crux of the matter. It has also opened up an ever-expanding market for other cardiac devices, because when this one no longer does the job, one can graduate to the LVAD – the left ventricular assist device, or heart pump, which costs ten times as much. Each device triggers quandaries about how one can or should live in relation to medical treatment, especially as one ages. Nowhere am I seeking to make a case for or against the use of the ICD or any other therapy. Rather, the questions for me are: How have clinical norms and our very lives been caught up in the perfect storm of ordinary, evidence-based medicine? How and why do evidence-based therapeutics bring increasing numbers of patients and families, politicians, and indeed our entire society to face the quandary of drawing the line, and to complain loudly about the systems that create that line? How, as more of us come to want, need, or acquiesce to these treatments, do the profound effects of evidence on medical practice and everyday life organize our ‘postprogress predicament’?
About the author
Sharon Kaufman, PhD, is Professor Emerita of Medical Anthropology and Chair of the Department of Anthropology, History and Social Medicine at the University of California, San Francisco. Her work explores topics at the intersection of medical knowledge and society’s expectations for health. She has examined the changing culture and structure of US medicine; health care delivery at the end of life; the relationship of biotechnologies to ethics, governance, and medical practice; and the shifting terrain of evidence in clinical science.