Notes from the field
Failing to thrive?
—
Abstract
‘Failure to thrive’
I recently took care of an eighty-year-old patient named Emma [note 1] who was found down, unresponsive, in a large pool of bloody vomit, in her apartment. She was described in her chart as an ‘80F admitted with fall, unresponsive, recent 30 lb weight loss’. She lived alone and was considered lucky to be found relatively quickly by a friend who sometimes came to check on her. Originally from southern Europe, she had been living in Massachusetts for the past twenty years and her closest family was in California. Emma was admitted to the intensive care unit and, with the ministrations of modern medical technology, including mechanical ventilators and medications to help keep blood pressures high, she lived. This was the second time in six months that she had been admitted to the intensive care unit after being found unresponsive in her home. In the intensive care unit, they found she had a very low blood count and discovered she had a gastrointestinal bleed. She had an extensive work-up, including an endoscopy and colonoscopy, and they still could not find the source. After she was transferred to the general medical floor, I came by on my rounds to check on her every morning. She was incredibly frail, sitting with her tiny legs propped up on a footstool. Every day she would deny having any blood in her bowel movements. ‘No blood, no pain, doctor. Can I go home today?’ Or maybe it was, ‘Doctor, can I go home today?’ ‘Not just yet’, I’d reply, ‘one more thing to do’.
What was the plan for this woman, whose diagnosis had evolved from a gastrointestinal bleed to ‘failure to thrive’? As I grappled with what was at stake for her, and had to deny her request to go home every single day, I thought about how increasingly common it is for medical practitioners to use this term ‘failure to thrive’, shortened in our notes to simply ‘FTT’.
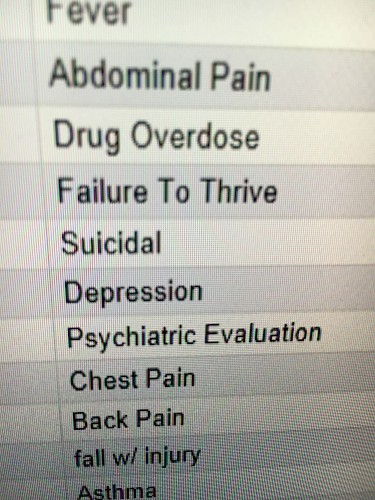
‘FTT’ is a medico-legal term initially used in a pediatric population (discussed further below), but today’s International Classification of Disease (ICD-10, published by the World Health Organization) includes diagnosis codes for hospital and clinical billing for both children (R62.51) and adults (R62.7). These are both grouped within the large diagnostic code 640: ‘Miscellaneous disorders of nutrition, metabolism, fluids and electrolytes’. With regard to children, the clinical information notes that there is ‘substandard growth or diminished capacity to maintain normal function’, at times ‘due to nutritional and/or emotional deprivation and resulting in loss of weight and delayed physical, emotional, and social development’ (WHO 2016, n.p.). FTT can be of organic, inorganic, or mixed etiologies, in which the first is understood to be a problem within the patient, the second as a problem in the patient’s environment, and the third a combination of two.
For adults, the ICD-10 definition is a ‘progressive functional deterioration of a physical and cognitive nature. The individual’s ability to live with multisystem diseases, cope with ensuing problems, and manage his/her care are remarkably diminished’ (WHO 2016, n.p.). In clinical practice, it can be used as a stand-in for unexpected weight loss. It can also be used as a proxy when clinicians and teams taking care of patients are faced with frequent admissions for patients with falls, failing to meet nutritional basic caloric needs to sustain stable weight, or otherwise existing in a tenuous or unstable living environment. It appears that within the common usage of the term FTT, medicine is actually grappling with the strong force of the social itself.
‘Lassitude, loss of energy, and joie de vivre’
Historically, the term ‘failure to thrive’ emerged in the late nineteenth century. There was an ongoing contest of ideas about what precisely constituted failure: was it related to nutrition, particular vitamin deficiencies, maternal neglect, congenital abnormalities, or physiological development of essential organs? The various stances largely reflected the cultural and political ideas and biases of the groups forwarding them. The late Victorian era was dominated by both increased attention to child welfare as well as the emergence of the idea of public health as a discipline and a means of collective intervention.
In the United States, the term ‘failure to thrive’ became popular in pediatric clinical medicine in the late 1960s, with robust use in the literature throughout the 1970s and 1980s. In the early use of the term, child psychiatrists associated the diagnosis with neglect between the mother and child (see Bullard et al. 1967) or to refer to an aberrant bond between the mother and the child (see for example Elmer 1960). Even then, it was a frustrating term to some; Henry Marcovitch (1994, 35) notes it was primarily a ‘descriptive term, not a diagnosis’, marked by ‘evidence of lassitude, loss of energy and joie de vivre’. Those working in inpatient hospital settings noted that ‘failure to thrive’ could be diagnosed by weight below the third percentile ‘with subsequent weight in the presence of appropriate nurturing’; they felt that was ‘characteristic of the child with failure to thrive to have improvement of these symptoms with hospitalization’ (Barbero and Shaheen 1967, 640), suggesting problems within the child’s home environment.
Initially, there was a strong distinction between ‘organic’ versus ‘nonorganic’ failure to thrive (read: biological versus social). Altemeier and colleagues (1985, 361) described ‘nonorganic failure to thrive’ as a ‘form of maternal neglect, because rapid improvement in both growth and development follows adequate nutrition and emotional support in the hospital’. Yet increasingly pediatricians recognized the complex interplay between a child’s position within growth curves and underlying medical conditions, parental behavior, poverty, and the overall home environment (Markowitz et al. 2008, 481).
Interestingly, the diagnosis of FTT has begun to fall out of favor. For pediatricians in particular, FTT is no longer en vogue. Parents dislike the term FTT for its vague all-encompassing nature and the implications of moral wrongdoing. There is stigma about being a parent of a child with FTT, and for that reason it is becoming increasingly abandoned as a diagnostic term in pediatrics.
But the inverse is true regarding FTT and adults. Over the past twenty years, FTT has become used in relation to the cadre of elderly people living alone who often go unseen or unheard until they arrive in the hospital in distress. As Robertson and Montagnini (2004, 343) write, ‘Failure to thrive describes a state of decline that is multifactorial and may be caused by chronic concurrent diseases and functional impairments … including weight loss, decreased appetite, poor nutrition and inactivity’. In the hospital where I work, we see patients who are elderly, who are homeless, who are dying of AIDS or cancer, who are chronically malnourished; they all variously can be diagnosed with FTT.
Arriving at the hospital in the way that Emma did adds a certain immediacy and intensification towards the social worlds of such patients by both clinicians and the family members of patients. Physicians and care teams in hospitals are routinely tasked with addressing the fates of these patients, and the way they do so shapes the course of these individuals’ lives. Emma is not unique. The New York Times profiled a person named George Bell, whose often lonely life and lonely death was chronicled in great detail, as an exemplar of an increasingly solitary, aging population (Kleinfeld 2015). Sociologist Eric Klinenberg (2001) writes about this phenomenon in his article ‘Dying Alone: The Social Production of Urban Isolation’, which analyzes the 1995 Chicago heat wave that killed over seven hundred mostly elderly, isolated Chicago residents, and which was followed by his book, Going Solo: The Extraordinary Rise and Surprising Appeal of Living Alone (2012). The appeal of being alone and living alone is woven into the American ethos of self-determination, autonomy, and independence, including the freedom to live and die in circumstances of our own choosing.
Hospitals are places where people who lack a social safety net, like Emma and George Bell, are brought. In fact, we routinely admit and discharge patients like them every day. What is my ethical obligation as a physician to these patients – to do no harm, to promote safety, to ensure the best chances of health and well-being – versus my moral obligation to honor and respect another person’s autonomy? Is it my obligation or right to deny Emma the opportunity to die in the time and place of her own choosing, as a direct result of what some might deem to be failures of self-care but in the conditions of her own determining? Sharon Kaufman (2005, 1) argues from her ethnographic work on dying in hospitals that as human beings and as physicians we have a ‘deep, internal ambivalence about death’; she argues that the process of hospitalization extends and indelibly alters the process of the ‘gray zone at the threshold between life and death’.
I am faced with this dilemma with Emma. Her hospitalization poses significant existential questions about the quality and quantity of her life and the inevitability of her death. I am faced with the immediacy and stakes of another’s life; I am implicated in either action or inaction. What am I compelled to do with the private, intimate knowledge of another’s pathology laid bare in the hospital records? As physicians every day we confront these realities of messy lives and deaths so often hidden away: ‘We stand in the thick of human experience, in the space of human problems, in the real-life local places where people live in the face of dangers, grave and minor, real and imagined’ (Kleinman 1998, 376).
On thriving
As anthropologists, we maintain faith in the belief that we can access someone else’s lifeworld, that at the very least, we can recognize the shifting beliefs and narratives that ground experience. But my professional obligation as a physician, by an uncodified, implicit, bioethical stance, is to assure as much safety as possible, to create the conditions for physical flourishing even at the expense of happiness and autonomy. Yet very rarely do our thought processes take into account ‘what is at stake’ (Kleinman and Benson 2006, e294) for people within these encounters.
In many ways, these encounters of physicians with patients labeled as ‘failure to thrive’ represent the problem of witnessing and confronting a suffering other. In my case, I feel conflicted by shifting roles and obligations as a human being, as part of a community plagued by social inequalities in which some people lack or shirk adequate social and financial supports, and as a physician with a specific professional obligation to individual patients. What am I to do if I cannot prescribe you the community supports you need? Can I write you a prescription for love, for a friend? Can I write your children a work note every day for a month so that they can spend more time with you, check on you every day, and help you bathe and shower and toilet and take your medications? Can I get you a twenty-four-hour home health aide if you and your family don’t have the resources to do so?
This genealogy of failure to thrive is perhaps ironically considered within the realm of my medical internship and residency training, where I work approximately eighty hours a week in the hospital as part of ongoing medical training. What does it mean to be well within this context? What does it mean, generally speaking, to cultivate the conditions of wellness, prosperity, happiness, or self-care of the caregivers? US doctors know our colleagues in Europe work about half the number of hours (approximately thirty-seven to forty-eight hours per week) and emerge with similar competencies as part of more effective health care and public health systems with overall better health outcomes (Temple 2014).
In the United States, ‘intern year’, the first year of medical residency training, is often discussed as one of the hardest years of a physician’s life. Sometimes it is chalked up to ‘hazing’. Intern year is largely defined by the impossibility of addressing higher-order complex social and cognitive processes in the absence of meeting biological and physiological needs such as adequate sleep and food. As young physicians training in the United States we are asked to think critically and analytically about the everyday dilemmas faced by our patients and respond to them empathetically, but this analysis is not applied to ourselves as caregivers.
On the face of it, the task of caring for FTT patients that falls onto medical trainees seems impossible. And physicians don’t like dealing with the spaces in-between. ‘Failure to thrive’ is precisely that messy in-between that both patients and their caregivers want to avoid. Yet it is a diagnostic category that reflects ongoing temporality and a dynamic, uncertain process. It is increasingly becoming a part of aging in America, reflecting social isolation and the thin threads of community and unpaid hours spent by family members grappling with the very same dilemmas. As Michael Jackson (2011, xiii) reflects on his work with the Kuranko people in Sierra Leone:
Just as human existence is never simply an unfolding from within but rather an outcome of a situation, of a relationship with others, so human understanding is never born of contemplating the world from afar; it is an emergent and perpetually renegotiated outcome of social interaction, dialogue and engagement. And though something of one’s own experience – of hope or despair, affinity or estrangement, well-being or illness – is always one’s point of departure, this experience continually undergoes a sea change in the course of one’s encounters and conversations with others. Life transpires in the subjective in-between, in a space that remains indeterminate despite our attempts to fix our position within it.
While anthropologists have tried to understand upstream sources of suffering – what is here called ‘failure to thrive’ in Emma’s case – Kleinman and Wilkinson (2016) argue that the social sciences, anthropology included, have largely failed to enact the reparative visions of society laid out by eighteenth- and nineteenth-century thinkers like Adam Smith, John Stuart Mill, John Locke, and Voltaire. So both anthropology and medicine have, in their own ways, done inadequate jobs of addressing the root causes of inequality and their consequent social suffering. The denotation of ‘failure to thrive’ should beget the question of why only some fail to thrive. In many ways, failure to thrive is the result of the unequal distribution of political and socioeconomic power and capital.
When I think about the cases of patients like Emma, I am positioned between often-conflicting worldviews and stances towards individual and social suffering. Yet in my role as a doctor, I am compelled to take action every day. These are decisions that can and do have a long-lasting impact on others’ lives, an impact that I may never entirely know the consequences of. I often wonder how we can maintain our humanity in the face of all of this, including the pressures from hospital systems to move patients quickly out of the hospital, towards an ultimate ‘disposition’. How can we attend to these patients with care, acknowledging the specificities of their individual situations and the very real constraints in their social milieus that cannot be solved with a three-day hospital admission?
As essayist Leslie Jamison (2014, 23) writes in her book The Empathy Exams, we should not necessarily lose hope in our abilities to care for others: ‘Empathy isn’t just something that happens to us – a meteor shower of synapses firing across the brain – it’s also a choice we make: to pay attention, to extend ourselves … the labor, the motions, the dance – of getting inside another person’s state of heart or mind’. This we can do confidently. We can attend patiently the particulars of individual situations. We can listen. But we must remember to do this while also addressing the overall structures of power and vulnerability, whereby those at the social margins are most affected. And we cannot forget that how these structures are assembled and interact influences our ability to attend to one another as we envision alternate ways of living, caring, and dying.
About the author
Kim Sue is a second-year resident physician in the Internal Medicine-Primary Care program at Massachusetts General Hospital, in Boston, MA. She is a graduate of the Harvard Medical School Social Science MD-PhD track (PhD 2014, medical anthropology; MD 2015). Her dissertation focused on the experiences of women with opioid addiction in the US prison system. Her current clinical interests include providing primary and mental health care for people with histories of incarceration and/or addiction.
References
Altemeier, William, Susan O’Connor, Kathryn Sherrod, and Peter Vietze. 1985. ‘Prospective Study of Antecedents of Nonorganic Failure to Thrive’. Journal of Pediatrics 106: 360–65.
Barbero, Giulio, and Eleanor Shaheen. 1967. ‘Environmental Failure to Thrive: A Clinical View’. Journal of Pediatrics 71: 639–44.
Bullard, Dexter, Helen Glaser, Margaret Heagarty, and Elizabeth Pivchik. 1967. ‘Failure to Thrive in the “Neglected” Child’. American Journal of Orthopsychiatry 37: 680–90.
Elmer, Elizabeth. 1960. ‘Failure to Thrive: Role of the Mother’. Pediatrics 25: 717–25.
Frank, D., and S. Zeisel. 1988. ‘Failure To Thrive’. Pediatric Clinics of North America 35: 1187–1206.
Jackson, Michael. 2011. Life within Limits. Durham, NC: Duke University Press.
Jamison, Leslie. 2014. The Empathy Exams. Minneapolis, MN: Graywolf Press.
Kaufman, Sharon. 2005. And a Time to Die. Chicago: University of Chicago Press.
Kleinenberg, Eric. 2001. ‘Dying Alone: The Social Production of Urban Isolation’. Ethnography 2: 501–31.
Kleinenberg, Eric. 2012. Going Solo: The Extraordinary Rise and Surprising Appeal of Living Alone. New York: Penguin.
Kleinfeld, N.R. 2015. ‘The Lonely Death of George Bell’. The New York Times, 18 October, A1.
Kleinman, Arthur. 1998. ‘Experience and Its Moral Modes: Culture, Human Conditions, and Disorder. The Tanner Lecture on Human Values’. Presentation at Stanford University, Palo Alto, CA, 13–16 April.
Kleinman, Arthur, and Peter Benson. Anthropology in the Clinic: The Problem of Cultural Competency and How to Fix It. PLoS Med 3, no. 10: e294. https://doi.org/10.1371/journal.pmed.0030294.
Kleinman, Arthur, and Iain Wilkinson. 2016. A Passion for Society: How We Think about Human Suffering. Berkeley, CA: University of California Press.
Marcovitch, Harvey. 1994. ‘Failure to Thrive’. BMJ 308: 35–38.
Markowitz, Robert, John Watkins, and Christopher Duggan. 2008. ‘Failure to Thrive: Malnutrition in the Pediatric Outpatient Setting’. Nutrition in Pediatrics. 4th ed., 479–89. Hamilton, Ontario: BC Decker Inc.
Robertson, Russell, and Marcos Montagnini. 2004. ‘Geriatric Failure to Thrive’. American Family Physician 70: 343–50.
Temple, John. 2014. ‘Resident Duty Hours around the Globe: Where Are We Now?’ BMC Medical Education 14: S1–S8.
World Health Organization. 2016. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. http://apps.who.int/classifications/icd10/browse/2014/en.
Endnotes
1 Back
A pseudonym.