Orchestrating home
Experiences with spousal stroke care
—
Abstract
Introduction
The shift in health care from institutional (hospitals, clinics) to community settings has become a focal point in welfare policies over the past four decades in most industrialised countries (Heaton 1999; Henderson 2005; Williams 2002). The home is central to this. In Australia, most rehabilitation following intensive in-hospital treatment now takes place domestically, provided largely by informal (and thus un- or underpaid) carers, with some support from formal (paid) care services (Anderson et al. 2000; Dollard et al. 2004; Dow 2004; Dow and McDonald 2007; Mayo et al. 2000; Pearson et al. 2012; Walters et al. 2010). In such arrangements, home-based care is perceived – at a political and a local level – as both cost efficient for public health care systems and beneficial for the well-being of the patient (Martin et al. 2005; Williams 2002, 2004). Policy makers, health care providers, and the broader community see family members as integral to this notion of home as a preferred site of care, and over the past three decades they have introduced significant initiatives that rely heavily on family members providing the bulk of care (Dow and McDonald 2007). These trends are particularly pronounced for stroke rehabilitation, which often involves long and fluctuating care trajectories.
While home may have certain therapeutic qualities, and is usually the place where people with chronic conditions prefer to live (Manderson and Warren 2013), home is taken for granted as an a priori entity that naturally and unproblematically provides continuity and stability. This assumption neglects the fact that many people who have had a stroke face various struggles at home. Everyday routines in home spaces become time consuming and difficult, familial and social relationships are disrupted, and a lack of mobility can lead people to feel they are trapped in the house, impacting on their social and emotional well-being (Achten et al. 2012; Meijering, Nanninga, et al. 2016; Nanninga et al. 2014; Salter et al. 2008). The home environment in and of itself, then, is not necessarily conducive to the elements of recovery that may be especially important, including the social and emotional domains of a sense of belonging, continuity, control, and hope (Benz 2003; Carlsson et al. 2009; Cott et al. 2007; Erikson et al. 2010; Gallagher 2011; Graven et al. 2013; Vanhook 2009).
Also assumed in home-based care is the capacity and willingness of carers, particularly spouses, to transfer the therapeutic qualities of an institutional setting to the home (Burton 2000; Dow and McDonald 2007). The shift to the home setting changes the nature of rehabilitation itself (see, for example, Pollack and Disler 2002) from a specialised medical practice to an endeavour delivered by committed but often untrained carers, who may (or may not) receive some support from community-based allied health professionals. Rehabilitation also changes with the site shift from an enterprise that is carefully monitored and benchmarked (Gubrium et al. 2003) to one that is self-directed and self-managed through lifestyle adjustments and home-based activities (Dow 2004; Essue et al. 2010; Pritchard et al. 2015). These care activities are often performed by spouses, and can have a large impact on their lives, as they themselves deal with uncertainty, grief over the lost past, and changes in various roles within and outside the family (Bäckström and Sundin 2009; Bendz 2003; Greenwood et al. 2009; Lawrence and Kinn 2013; McCarthy and Bauer 2015; Quinn et al. 2014).
In this article, we consider the role of spousal carers in the creation and maintenance of home as a therapeutic place. We posit that the physical place of home is not therapeutic in and of itself, but rather depends on carers’ constant work to reconfigure the physical, symbolic, and practical elements of home. This is not a straightforward process, as tensions arise in trying to integrate the new, post-stroke therapeutic landscape with pre-stroke conceptualisations and lived realities of home life. To understand this transition from home as an idealised concept to an emergent therapeutic environment following stroke, we begin by mapping the literature on the role of place in facilitating health, particularly the concept of ‘therapeutic landscapes’ (Gesler 1992, 1996), and then illustrate how the conceptualisation of home is shaped through the active and ongoing efforts of carers.
Therapeutic landscapes and home
The health-promoting capacities of place have been extensively discussed in relation to the concept of therapeutic landscapes, originally defined by Gesler (1992) as places reputed to have the power to facilitate healing, such as Lourdes, a pilgrimage site (Gesler 1996). The notion of therapeutic landscape has since been employed to study experiences of healing, recovery, health, and well-being across a variety of settings (Gesler 2005; Williams 1999, 2007), including hospitals and clinics (Curtis et al. 2007; Wood et al. 2013), respite centres (Conradson 2005), hospice day care locations (Moore et al. 2013), community gardens (Milligan et al. 2004), yoga studios (Hoyez 2007), and places of day-to-day routines such as home (Dyck and Dossa 2007; English et al. 2008; Martin et al. 2005; Williams 2002). These studies highlight how ‘physical and built environments, social conditions and human perceptions combine to produce a [therapeutic] atmosphere’ (Gesler 1996, 96).
The therapeutic potential of a site is always relational, and cannot be assumed to hold the same therapeutic values for all people. Individual settings may be therapeutic or detrimental depending on the person’s relationship with the particular site, the others present, and the objects that occupy the space (Conradson 2005; Donovan and Williams 2007; Meijering, Lettinga, et al. 2016; Milligan and Bingley 2007; Wakefield and McMullan 2005). This relational aspect of therapeutic landscapes means that they are actively produced through their physical design (see for example Curtis et al. 2007; Wood et al. 2013), discursive construction (for example, Hoyez 2007), and/or situated activities and practices (see for example Dyck and Dossa 2007; Laws 2009). How these social processes interact with the physical, social, affective, or symbolic properties of a place dictates whether or not the place is experienced as a therapeutic landscape (Conradson 2005; English et al. 2008; Martin et al. 2005).
The concept of home is underlain by the notion that it is a particular, special type of place, one that is more than the dwelling itself. The meanings of home are also shaped by social and psychological factors, including gender, socioeconomic status, class, ethnicity and family structure, and by personal relationships with home (both as an idea and with regards to a particular setting) (Mortenson et al. 2016; Williams 2002; 2004; Sixsmith et al. 2014). In its ideal form, home is considered a safe, protected place where individuals feel in control and are able to express a sense of self in an intimate and supportive environment (Milligan 2009; Warren 2009). It is often contrasted with institutional settings (Martin et al. 2005), although such settings can be therapeutic landscapes if their design and activities produce a sense of home (Moore et al. 2013; Tyreman 2011; Warren and Manderson 2008). Home is more than a symbolic representation of self, as various embodied and affective performances and practices take place within the space (Blunt 2005; Foley 2011; Yates-Doerr and Carney 2015). Given the centrality of its meanings to one’s identity, home has primacy in facilitating the recovery of an identity disrupted through illness (Bury 1982; Becker 1997; Williams 2002) and potentially in providing a sense of continuity, belonging, and control to a life otherwise disrupted (Rowles 2008; Wiles et al. 2012). Yet, while these ideas emphasise the stability of home, these are places that are dynamic, negotiated, and contested. Experiences of home may change from therapeutic to nontherapeutic – even detrimental – for an individual during illness or upon the onset of a chronic condition that leads to bodily limitations (Meijering, Nanninga, et al. 2016), for their informal carers (Donovan and Williams 2007), and for those who must adapt to home modifications (Aplin et al. 2013; Tanner et al. 2008).
In conceptualising the production of home spaces as ongoing, we draw on Hand and Shove’s (2004) description of domestic space as ‘orchestrated’, and explore how social, material, and practical elements co-produce the experience of home. In this framework, the home is not a pre-existing container in which cultural norms are enacted, but rather a space in which ‘materials, images, and forms of competence “hang together” at different points in time and space’ (Hand and Shove 2004, 235). The home as it is experienced emerges and re-emerges out of relations between materials, meanings, and practices. Constitutive elements are continually made and remade, and the dynamism of these domestic spaces is made visible through such choreographies. New elements do not simply replace existing elements; they may or may not be appropriated into existing configurations depending on their fit with other constitutive elements in maintaining the integrity and coherences of a place. Hand and Shove (2004, 250) use the notion of an ‘orchestrating concept’ to describe a mechanism of integration, a kind of ‘force field’ that holds together the constitutive elements, resulting in a certain configuration at a given time.
In this article, we contend that the therapeutic value of home is derived through processes of orchestration, whereby spousal carers work to create for their stroke-affected partner a sense of being at home and of the continuity that this offers. We focus on how these orchestrations are forced upon our participants by the sudden – often completely unanticipated – stroke event and subsequent discharge from rehabilitation. In so doing, carers attempt to incorporate the therapeutic potential of a home space while trying to remain faithful to the orchestrating concept of the home as a continuation of the pre-stroke home. As we elucidate below, such efforts are not unproblematic.
Methods
Our analysis draws upon ethnographic research with thirteen women and four men who provided care for their spouses who had had a stroke while still of working age (roughly between eighteen and sixty-five years of age), and so were considered, clinically and in the research literature, ‘younger’ stroke survivors.[note 1] Conducted in Victoria, the southeasternmost state of mainland Australia, between 2011 and 2014, our research explored how stroke, a disease commonly associated with old age, impacted on the lives of spousal carers, including in terms of parenting, paid employment, and intimate and social relationships. Researchers have suggested that the biographical impact of stroke has different meanings and salience for younger survivors and their families (see for example Lawrence and Kinn 2013) compared to older people, who consider stroke as a not-unexpected part of ageing (Faircloth et al. 2004; Pound et al. 1998). We wanted to understand how undertaking various stroke care responsibilities and technologies also affected spouses.
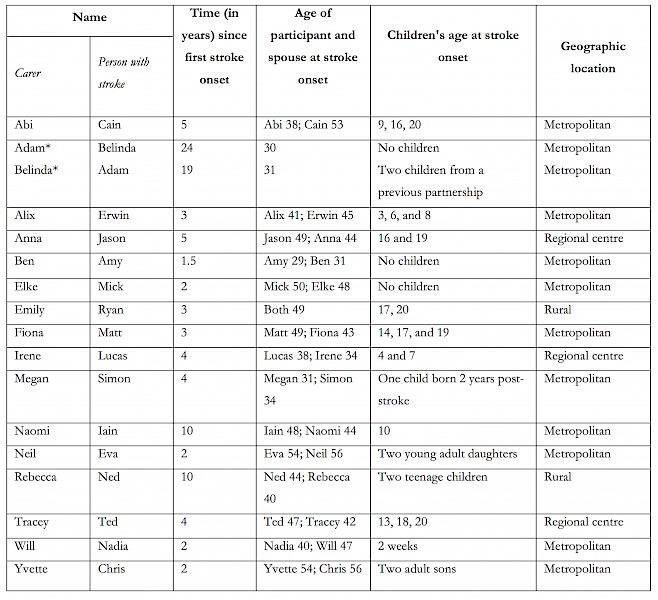
Participants were aged between thirty-one and fifty-six years of age when their partners (aged twenty-nine to fifty-six) experienced stroke (see appendix for the demographic characteristics of the study sample). All participants were interviewed at least one year after their partner’s stroke and all but four within six years afterwards, although the time that had elapsed since the first stroke event varied between participants (range: one and one-half to twenty-four years; median: four years). They resided across the state, in urban, regional, and rural areas, and all lived in single-detached dwellings, the most common form of housing in Australia (Australian Bureau of Statistics 2012). All were recruited through community-based stroke support groups.
In-depth interviews took place in participants’ homes, cafés, and public library meeting rooms during 2012 and 2013; interviews were audio-recorded and subsequently transcribed verbatim. Participants were asked a mixture of retrospective, current, and prospective questions about: their relationships with their partners, other family members including children, and people in their social networks; difficulties and rewards involved in their role as carers; formal and informal support systems including welfare support; employment and financial situations; and whether and how the caring role affected their lives. Although they were not specifically asked during the interviews to describe what ‘home’ meant to them, all participants discussed changes to physical, symbolic, and affective aspects of home following their spouses’ strokes, often without prompting. These data were supplemented by observation in their homes to contextualise participants’ accounts of care practices at home. The project was approved by the Monash University Human Research Ethics Committee. All participants are referred to by pseudonyms.
Primary data analysis was conducted by the first author using an approach informed by Charmaz’s (2007) constructivist grounded theory. Following initial coding and focused coding processes, substantive codes were identified to capture emerging themes and concepts. These codes were not created based on the frequency of similar statements; rather, codes were clustered to explore different properties and dimensions of the phenomenon they represented (Charmaz 2007). The coding framework was developed iteratively through constant comparison and as new data were collected. The ongoing and dynamic nature of care activities at home became apparent during analysis, and at this stage the concept of orchestration, as articulated by Hand and Shove (2004), came to be salient in understanding participants’ accounts. Subsequent data analysis was then undertaken using a more ‘abductive’ approach (Timmermans and Tavory 2012) in order to pay closer attention to how the sense of being at home was created and maintained. The second and third authors provided ongoing reflection and discussion regarding the analytical framework and findings.
Orchestrating home: Changing material, practical, and symbolic elements of home
Various technologies of care were integrated into the physical space of home. These included extensive bathroom modifications: widening doorways and passageways, and installing and/or placing specialised care equipment in different spaces in the home. These physical changes were made to enable a degree of independence for the stroke-affected partners around the house; reflecting this, rehabilitation professionals and government subsidy schemes tend to focus on this aspect of functional independence associated with care technologies (Sakellariou 2015; Pavey et al. 2015). Some participants discussed how these technologies, incorporated into the home environment, were instrumental in facilitating their partners’ socioemotional well-being. Rebecca’s house illustrates this.
Ned, Rebecca’s husband, had had a stroke at age forty-four, when they were living with their two teenage children on a farm, two hours’ drive from the closest regional centre (‘Hakea’) where rehabilitation facilities and other medical services were available. Rebecca (then aged forty) returned to her work as a schoolteacher three months after the stroke but, given Ned’s mobility restrictions, she also continued to work their farm. These double duties became overwhelming, even with help from their children and Ned’s brothers on weekends and school holidays. At the same time, their house was not ‘disability-friendly’. This had been irrelevant prior to Ned’s stroke, as Rebecca noted: ‘Our old house had … very narrow passages, narrow showers and a very hard toilet to get into, [but] you don’t look at your house that way until something happens’.
The particular physical configurations and geographical location of their home no longer aligned with the practical considerations required to meet Ned’s needs. Previously taken-for-granted everyday routines were now difficult, and new routines needed to be incorporated, such as visits to medical and rehabilitation facilities (see also Meijering, Nanninga, et al. 2016). This discordance threatened the symbolic dimension of home for both Rebecca and Ned (Blunt 2005; Healey-Ogden 2013). Although Rebecca tried to reinforce the symbolic elements of home by increasing her presence there, reducing her work hours and staying at home more frequently, there were limits to what could be done without making changes to the physical environment. So, they decided to sell their farm and build a new house on Rebecca’s parents’ property on the outskirts of Hakea. This would ensure better access to medical facilities and reduce the ‘huge pressure put on our family’ by multiple demands: farm work, frequent long drives to rehabilitation facilities, Rebecca’s work, visits to her gravely ill father, and their children’s school and sporting activities.
Their new home was noticeably open in its design: full-wall windows let in the sunlight and provided a vista of hills from the living room, passageways and doors were wide, and the bathroom areas were spacious. Rebecca explained that their new accessible house had been custom built to meet Ned’s needs, with consideration given to his capacity for social engagement. The wider spaces and smooth (rather than carpeted) floors not only facilitated Ned’s movement around the house, but also allowed other people with mobility restrictions to visit. This occurred regularly as they became active members of a stroke support group. Rebecca explained, ‘This house is built sort of like a nursing home… . It’s got wheelchair access, wider [doorways] and the passages, so if we have people in wheelchairs come here, they can get around with ease’.
This engagement was important for Ned. Prior to his stroke, Ned had been a socially active and outgoing person, and a prominent member of the local football club, with whom he was often found drinking beer. Following the stroke and subsequent move to Hakea, his friendship group primarily consisted of those from the stroke support group. The new house enabled some continuity in Ned’s identity as a socially engaged person. Being able to have their friends around the house also contributed to his emotional stability, as he had experienced depression and his psychological well-being was one of Rebecca’s major concerns. His emotional lability affected her career aspirations, and she refused a promotion: ‘If I work full time, the wheels start falling off at home and depression starts kicking in with Ned’.
In order to manage his depression, Ned needed to be occupied, especially when Rebecca was not around. Living near Rebecca’s parents and their farm kept Ned busy and involved in farming activities, something he had previously enjoyed. Rebecca explained, ‘My mother runs her cattle, but she needs a backup. She rings Ned up and says, “I’ve got to get the vet out”, and it’s really good for Ned, because it gives him something to do, so he feels important’. By helping out on the farm, Rebecca reasoned, Ned could experience a sense of continuity with his pre-stroke identity, albeit without the responsibility and burden of running a farm. Home as a therapeutic landscape, therefore, was orchestrated based on Rebecca’s belief that its physical and social location gave Ned a sense of purpose and satisfaction as well as aesthetic pleasure (Milligan et al. 2004).
The house’s large windows provided Ned further opportunities to interact with the open country landscape without having to physically leave the house. This feature was deliberately incorporated with the aim to reducing the sense of isolation that he had experienced after his stroke when he was home alone. Rebecca explained: ‘He is here twenty-four hours a day, and that’s why it’s so open, so he can see out… He takes great enjoyment in watching the birds, the kookaburras and everything else’. Through its physical features, the house not only facilitated Ned’s everyday functional needs, but also allowed Rebecca to accommodate what she believed were Ned’s psychosocial needs by creating possibilities for him to continue doing things he desired (Johansson et al. 2009; Sakellariou 2015). These physical aspects of the home interacted with and facilitated the symbolic, ideational, and practical dimensions of home. Such enacted ‘atmospheres’ of sociality, belonging, and optimism contributed to Ned’s recovery (Duff 2015; Gesler 1996), insofar as recovery was understood as a process of resuming previously valued activities and social connections (Graven et al. 2013).
A stroke also prompted changes in the use of existing domestic spaces, particularly to enhance the mobility and maintain the fitness of the person who had had the stroke. After Mick had a stroke at age fifty, his wife Elke (then age forty-eight) transformed a section of their house that had previously been dedicated to entertaining into a space for rehabilitation, stocked with a seemingly endless array of physical and speech rehabilitation equipment and books, most purchased on the Internet and paid for out-of-pocket (rather than from medical insurance). In this space, Elke spent a significant amount of time conducting home rehabilitation exercises with Mick. In an interview two years after Mick’s stroke, when asked about the room, she explained:
That used to be a billiard room. [Now it’s a] rehab room [for when] it’s really hot and you can’t go for a walk, or if I wanted him to be more active – and I don’t want him to sit a lot, or on the couch and watch TV. He has to do other stuff in between. Then he will walk around the billiard table, just to keep moving.
The room was located away from the living room, behind a sunroom, and this configuration kept the rehabilitation equipment and activities separate from the rest of the home, creating a space akin to a home office. This separated their home life from the rehabilitation activities that could at times be strenuous and/or boring. Elke described how she had tried to frame rehabilitation as a kind of work: ‘I said to him, “before [the stroke] you went to work, Monday to Friday, 7am to 4pm, and now this is your work. It’s just harder”’. This way of reimagining ‘work’ as a home-based activity allowed Elke to encourage Mick to experience a sense of continuity by connecting his past to the present. The orchestrating concept of the idealised, pre-stroke home was mobilised to incorporate elements of the home as a therapeutic landscape into the home as a pre-stroke space. This mobilisation at the same time shifted the orchestrating concept by redefining the home as a space of both ‘work’ and ‘living’.
However, this repurposing of existing domestic space for rehabilitation activities did not necessarily lead to the medicalisation of home (Aplin et al. 2013; Tamm 1999; Moore et al. 2010). Rather, the separation of the rehabilitation room from the rest of the home space was fluid and, at times, blurry – in the ‘rehab’ room, a basket of unfolded laundry awaited folding, and memorabilia injected a sense of self-expression, collective identity, and biographical history (Tanner et al. 2008). In integrating multiple meanings into the one space, the rehabilitation activities did not signal a replacement of one identity with another (husband to patient, wife to physiotherapist). Elke placed caregiving within a larger context of a long-term relationship and its changes:
Things obviously change all of sudden, and you have less spare time for you. That’s what you do when you are married. That’s your job, basically, to look after your partner if something happens. And if things change, things change. You deal with it then. It might be different, or harder, but that’s the way it is.
While Elke provided care as part of her role as wife, she also worked to integrate the spatial, practical, and material configurations of home into the relations constituting home. This involved maintaining a balance between care activities, their intimate relationship, and other aspects of home life.
Home as an assemblage of orchestrating efforts is marked by an ‘uneven mosaic of development, fracture, and continuity’ (Hand and Shove 2004, 249). Changes to the home were often made to fit and align with other changing symbolic and practical elements following a stroke, which facilitated the shaping of home (by the carer) as a therapeutic landscape (for their partner). Home as a physical site was necessarily re-organised, not only to minimise the risk of accidents but also to produce a therapeutic landscape that provided a sense of continuity, sociability, and safety. However, whether or not these practices contributed to a therapeutic landscape depended on delicate and balancing orchestrating acts. For carers, this involved a range of orchestrating efforts to soothe any discordance between the material, symbolic, and practical dimensions of home. As we discuss below, this process of orchestration involved considerable negotiation, often creating tensions.
Tensions in home orchestration
Some of the consequences of stroke could not be accommodated without a certain degree of sacrifice on the part of the spouse of the person who had a stroke. When such a compromise was made, some of the markers of home were surrendered. After he had a stroke, Ryan (aged forty-nine), could not stand being in a noisy environment, as it exacerbated his fatigue and restricted his capacity to communicate, which was already limited by aphasia (an impairment of language that affects the production and/or comprehension of speech). Instructed by Ryan’s speech therapist that he be allowed to speak as often and as long as possible at home, his wife Emily (also forty-nine) forced herself to be patient when he was trying to verbalise his thoughts. This was not easy, especially when she was tired after work or trying to concentrate on her own hobbies of knitting and sewing, because, she said, it sometimes took ‘five minutes for him to think of the word and get it out’. This also meant that they could not have music at home when Ryan was around. Emily lamented, ‘I love my music but I can’t have it on in the background, because the background noise frustrates and distracts him and he can’t think about what he wants to say… . I’ve had to forego some things [to accommodate his needs]. When I’m out in the craft room and he’s not there, I turn my music up full bore’.
Home as a therapeutic place for Ryan needed to be orchestrated through Emily’s patience and sacrifice. This meant that home was neither stable nor confined in a certain space-time. When she needed respite from her orchestrating efforts, Emily’s home shrank to the craft room, because music to her was an important component of what it meant to be at home (see also Mayes et al. 2010). When Ryan was present, music had to be replaced by other components of home, most notably, Ryan himself. In this way, home was fluid and constantly changing.
The examples of Emily and Ryan and Elke and Mick demonstrate how adopting new routines, extending their spousal identity to accommodate their delivery of care, and reorganising spaces can enable the therapeutic potential of home. However, this was not always straightforward; for some, it created new tensions that required negotiation. For example, Rebecca faced many difficulties as she tried to sell the farm and create a better home for Ned: navigating town politics, whereby she was expected to sell the farm to another townsperson at a below-the-market value; facing gossip when she refused an offer from a neighbour; juggling caring for Ned, paid employment, parenting, organising the move, and tending to her gravely ill father; and dealing with complicated financial and tax issues. Ben (aged thirty-three) also struggled to find a balance after his wife Amy (aged twenty-nine) had experienced stroke eighteen months earlier. He struggled with how much to engage in rehabilitation exercises at home and how much to empathetically listen to her struggles without being critical or too assertive:
There’s been times where she just wants me to stop being on her back, and just be her husband rather than her therapist. But that’s quite hard, because if I don’t, I feel that she won’t do all the therapy, and she won’t recover as best as she can. So that’s a difficult balancing act sometimes. [I should be] just listening and chatting about nontherapy things and caring for her emotional side more than her physical side, I guess.
The tensions in spousal relationships that can occur in the process of rehabilitation, especially in the first few years (Banks and Pearson 2004; Graven et al. 2013), were evident in Ben’s account. Given Amy’s age, Ben was hopeful about her continued and steady physical recovery. However, he agonised over the possibility that his emphasis on physical recovery reminded her of health care professionals, who were predominantly focused on functional recovery (Bendz 2003). This practice contradicted with the symbolic elements of home that he did not wish to compromise based on what he thought Amy desired: continuity in her role as a wife, and the sense of safety and belonging associated with home (Erikson et al. 2010). This meant that Ben had to carefully manage his desire to reshape home as a site of physical therapy while not hindering Amy’s experience of home as a broader therapeutic landscape (Conradson 2005). The dilemma that Ben faced, then, was how to make a transition without compromising the link to the orchestrating concept of the idealised pre-stroke home.
Changed and new routines affected symbolic and affective elements of home, and this created tensions. We now draw on Will and Nadia’s experience to illustrate how material changes can precipitate conflict. Two weeks after giving birth to their daughter Sarah, Nadia (aged forty) had a stroke and thereafter experienced continued aphasia, hemiplegia (paralysis of one side of the body), and seizures. The paralysis and seizures increased Nadia’s risk of falling. She was unable to drive a car and so was confined to the home most of the time, where she required indirect supervision. Previously taken-for-granted everyday activities were thus redefined as potential sources of risk (Meijering, Nanninga, et al. 2016), especially given the changes to the landscape of home as their daughter grew, and as toys cluttered the floor, increasing the possibility of falls. Her husband, Will (aged forty-seven), was self-employed and often worked irregular hours; he was on call 24/7, and was sometimes required to attend to his clients at short notice. Although he sought to arrange his work to accommodate Nadia and Sarah’s routines and needs, he was also mindful of his clients’ needs and the importance of their patronage. At the same time, the unpredictable nature of Nadia’s health meant that Will was always mindful of her safety, especially when he was away from home: ‘The biggest danger is that if Nadia has a fall and I am not [at home], she can’t get up because she is not quite strong enough on her right leg to pick herself up’. Will’s concern was grounded in a prior experience of her falling, as he recalled: ‘It was just a simple fall in the bathroom where she was just reaching down in the cupboards to get something – and she just lost her balance and couldn’t get up… She managed to crawl her way to [get help]’.
Nadia’s fall increased the couple’s anxiety about everyday activities at home, and their fear about future accidents rendered home neither secure nor predictable (Alaszewski et al. 2006). Will desired to protect Nadia’s well-being, provide a sense of safety, and support her feeling of being ‘at home’. He employed several practices and activities to alleviate the threat of falling and so to restore the integrity of home as a therapeutic landscape. First, he used some of Nadia’s government-funded disability support to employ a private in-home childcare worker, Sharon, to care for Sarah. While caring for Sarah, Sharon provided direct and indirect supervision for Nadia, and so contributed to preserving home as a safe space. However, Sharon was not funded on a long-term basis, and so this sense of security was tenuous. In the face of this uncertainty, Will sought another strategy to rectify the situation: a personal alarm that would notify him if Nadia had a fall.
Although the personal alarm might have brought Will some peace of mind, this was not to be, because, he explained: ‘[Nadia] refuses to wear the personal alarm around her neck if she’s home by herself. She feels that that’s for old people’. Nadia saw the alarm as an intrusion into her home; given the images of frailty, dependence, and agedness that the personal alarm connoted (Aceros et al. 2015), it did not blend with other constituting elements of home for her. Because the affective and symbolic dimensions of home needed to be salient both for Will and Nadia, it was not implemented. This led Will to develop another strategy: video surveillance cameras that streamed directly to his phone. He was pleased with this, explaining: ‘All I do is just glance on it, and see if she’s alright. If she’s on the floor, I can call the ambulance’. The surveillance cameras and the mobile phone app gave home a sense of security once more. At the same time, these devices made home proximate, regardless of how far away Will was when working. The monitoring systems became a part of home, although, Will said, the cameras had to be defended from stern criticism from relatives: ‘Nadia’s godparents are dead against it, saying it’s an invasion of privacy. But, I said, “well, I didn’t have choice, really”’. Having finally found a strategy to ensure some degree of security at home, Will was not willing to relinquish this, despite opposition. This account highlights the many efforts spouses may undertake in trying to make the home space ‘home’, even in ways that destabilise their own experience of home.
Such efforts were severely constrained by finances. Physical modifications, particularly the purchase of aids and equipment not covered by public subsidies (also constrained by funding limits and complicated application processes), were expensive. Affording them was often even more difficult when the partner who had had a stroke was no longer working. Alix was forty-one when her husband Erwin had a stroke at the age of forty-five and was unable to return to work. They had a mortgage and three young children, and found the costs involved in modifying the home and purchasing care technologies exorbitant: ‘Everything is just ridiculously expensive. You get a lifetime grant of A$4,000 to modify your home. It costs you A$1,500 to widen the doorway. Now, to renovate the whole bathroom, you are looking at A$10,000. Then if you move, well, bad luck. You can’t do it again’.[note 2] Erwin’s stroke severely affected his mobility and he required various assistive technologies, including an electric wheelchair that could only fit through widened doorways. Financial support from the government was limited and purpose-built equipment was imported at a premium price, and the costs associated with fitting out the house and purchasing the wheelchair tested their financial capacity.
The costs and their impacts were cumulative over time for all participants, and the uncertain health status of the person who had had a stroke further complicated the installation of and payment for care technologies. Naomi’s husband Iain suffered a second stroke within a year of his first relatively minor stroke at age forty-eight; it was the second of four strokes, as well as multiple TIAs (transient ischemic attacks) that he had over ten years. Iain’s continuing deterioration meant that the funds from public subsidies were soon exhausted. Naomi described the extent of expenses: ‘Last year, we put in a bathroom downstairs for him… . [Because] Iain was coming home [from hospital], I couldn’t wait for A$4,000 worth of funding [from the subsidy]… . I spent probably A$40,000 altering the house, and buying additional equipment’.
A few weeks prior to this interview, after another stroke, Naomi decided to move Iain into high-level residential care. With severe limitations to his mobility, she felt that she was no longer able to lift him in and out of bed. In the context of material limitations, home for Iain, in his deteriorating condition, could no longer provide a therapeutic landscape as neither care technologies nor Naomi could keep pace with changes in his capabilities and needs. This highlights the limits of orchestration: despite a spouse’s efforts, a person’s impairments may not allow for them to be in their own home. Indeed, the therapeutic landscape was not static, but rather fluid, shaped by social, material, and temporal contexts (Meijering, Lettinga, et al. 2016).
Conclusion
In this article, we have paid particular attention to the orchestration of home in the context of spousal stroke care. Despite their relative youth, the full physical recovery of the stroke-affected partners was unlikely, and they required continuing long-term care (see also Cott 2004). The occurrence of stroke for both participants and their partner disrupted what Rowles (2000, 59S) termed the ‘choreography of being-in-place’ in relation to home, which refers to the routines, relationships, and meanings that meld to create a sense of being at home. This disruption meant that home could no longer be taken for granted as a place that provided a sense of continuity, safety, stability, and identity (Meijering, Nanninga, et al. 2016; Nanninga et al. 2014; Tamm 1999). While in clinical and rehabilitation contexts home is often narrowly conceptualised as a physical space (Healey-Ogden 2013), the work to accommodate stroke-affected partners prompted readjustments at affective, practical, and relational levels in addition to physical adaptations. Their recovery was interwined with social and emotional recovery, senses of relational and biographical continuity, belonging, and hope (Erikson et al. 2010; Graven et al. 2013; Warren and Manderson 2008).
As participants explained, home was not a self-contained, fixed entity that existed naturally or inevitably. Instead, making and sustaining home required constant orchestration to (re)configure various materials, meanings, and practices, to ensure they fit and align. Through this orchestration, home as a therapeutic landscape for the stroke-affected partner emerged. However, this process was not straightforward. New elements interacted with existing elements and a new configuration of home emerged. When new care and rehabilitation technologies and practices were integrated, this was carefully done in a way to enable a therapeutic landscape that still integrated the idealised pre-stroke home. These orchestrating efforts were situated in wider discourses of normality (see also Moser 2005), for stability only made sense in the context of what was considered normal. The value of care technologies, for example, depended on whether these could generate a sense of wider social engagement and autonomy (see also Pavey et al. 2015). Home as a therapeutic landscape mattered to people because it was the sense of being at home that enabled them, in the face of uncertainty, to replicate or resume various domains of life that were previously meaningful to them.
Spouses had to negotiate care responsibilities with other commitments, including parenting, paid employment, and financial obligations. These had an ongoing impact on their capacity to engage in orchestrating home for their stroke-affected partners. They too had to resolve tensions that arose as a consequence of their partners’ condition. While carers attempted to bridge the transition from the orchestrating concept of the pre-stroke home to that of a therapeutic landscape, the resulting configuration was at times not what they envisioned, and there were limits to what they could do in influencing this transition. For instance, despite their best intentions, the changes that both Ben and Will initiated were not welcomed by Amy and Nadia, who wished to maintain their identities tied to the orchestrating concept of the pre-stroke home. Iain’s deteriorating physical and cognitive conditions challenged Naomi’s attempt at orchestration; as his presence in the home became no longer possible, so too did his participation in the processes of orchestration.
In articulating participants’ orchestration efforts, our aim is not to draw a managerialist picture of spousal carers. Rather, as we have demonstrated, the orchestration of home as a therapeutic landscape is conducted by individuals embedded in various networks – spousal carers, their stroke-affected partners, social and care professionals, family and neighbours – and institutions including the disability and healthcare system, market economy, and discourses around health, age and gender. Orchestration is relational and dependent on these networks, emerging through a web of interactions amongst individuals, materials, and cultural and institutional norms, expectations, and practices.
There are some limitations to the study. All participants were recruited through support groups. This meant that they and their partners were more likely to be inclined or capable to seek social support outside the home space and/or received a greater degree of such support, more so than those who were not members of such groups. The experiences of the home may be different for those who are not able or willing – for a myriad of reasons that are outside the focus of this paper – to access the particular kind of social support available to many of our participants. Also, because the greater number of participant carers were women (reflecting gendered patterns of care), we have not provided systematic analysis of how gender interacts with the experiences of home orchestration. Even so, this is captured in some of the participants’ accounts. Ben, for example, reflected on the deficiencies in his emotional care, while Rebecca mentioned how the burden of financially managing the farm impacted on her capacity to maintain symbolic and practical elements of home. Both these tasks are gendered (Cheal 2002; Navaie-Waliser et al. 2002). Furthermore, we have not explored in detail how the length of time since the occurrence of stroke impacts on participants’ experiences. Naomi’s need to continually introduce physical modifications to home in response to Iain’s ongoing deterioration highlights the temporality and variability of health conditions. Even so, by attempting to connect the past and future in maintaining a home, people experience hope, despair, normalcy, disruption, and purpose (Gomersall and Madill 2015; Seymour 2002), and the examples that we present in this article illustrate how people manage these connections.
In demonstrating the efforts to orchestrate home as a desirable site of long-term care, we have drawn attention to the simultaneous multiplicity of home spaces. While spousal carers orchestrate home as a therapeutic landscape for their partner, this does not necessarily mean that they also experience home as a therapeutic landscape. As Wakefield and McMullan (2005) have demonstrated for cities as sites of both healing and hurt, we suggest that home is potentially a site of both healing and struggle, both for spousal carers and for those who have had a stroke.
Acknowledgments
The research reported in this article was funded by the National Heart Foundation/National Stroke Foundation Postgraduate Scholarship Program (PP11M-6167). Dr Narelle Warren was supported by a National Health and Medical Research Council Australian Research Training Award (606785). The authors thank Dr Margaret Winchester, the editorial staff of MAT, and the anonymous reviewers for their valuable and thoughtful comments on earlier drafts of this article.
Appendix
Summary of participant characteristics
Note: Both Adam and Belinda had experienced stroke and therefore considered themselves as carer for the other.
About the authors
Mutsumi Karasaki is a postdoctoral researcher at the Department of Sociology, University of Amsterdam. In his PhD project at Monash University, which he completed in 2015, he examined experiences of people whose spouse had a stroke at a relatively young age. His research interests focus on the intersections between family care and institutional and policy practices, with specific emphasis on disability and early childhood care.
Narelle Warren is Lecturer in the School of Social Sciences, Monash University. She is a medical anthropologist whose research is focused on understanding the relationship between the lived experience of neurological conditions, biomedical representations of the brain, and temporality, from both the perspectives of people living with such conditions and their informal caregivers. She is a co-editor, with Lenore Manderson, of Reframing Quality of Life and Physical Disability: A Global Perspective (Springer, 2013), an anthropological exploration of the concepts of well-being and quality of life.
Lenore Manderson is Distinguished Professor of Public Health and Medical Anthropology in the School of Public Health, The University of the Witwatersrand, Johannesburg, South Africa, and Professor of Anthropology, Brown University, Providence, RI, USA. She is editor and author, with Elizabeth Cartwright and Anita Hardon, of the Routledge Handbook of Medical Anthropology (2016), and has been editor of the international journal Medical Anthropology: Cross-Cultural Studies in Health and Illness since 2010.
References
Aceros, Juan C., Jeannette Pols, and Miquel Domènech. 2015. ‘Where Is Grandma? Home Telecare, Good Aging and the Domestication of Later Life’. Technological Forecasting and Social Change 93: 102–111. https://doi.org/10.1016/j.techfore.2014.01.016.
Achten, Diana, Johanna M. A. Visser-Meily, Marcel W. M. Post, and Vera P. M. Schepers. 2012. ‘Life Satisfaction of Couples 3 Years After Stroke’. Disability and Rehabilitation 34, no. 17: 1468–72. https://doi.org/10.3109/09638288.2011.645994.
Alaszewski, Andy, Helen Alaszewski, and Jonathan Potter, J. 2006. ‘Risk, Uncertainty and Life Threatening Trauma: Analysing Stroke Survivor’s Accounts of Life after Stroke’. Forum: Qualitative Social Research 7, no. 1: Article 18. http://www.qualitative-research.net/index.php/fqs/article/view/53/109.
Anderson, Craig, Cliona Ni Mhurchu, Sally Rubenach, Michael Clark, Carol Spencer, and Adrian Winsor. 2000. ‘Home or hospital for stroke rehabilitation? Results of a Randomized Controlled Trial: II: Cost Minimization Analysis at 6 Months’. Stroke; A Journal of Cerebral Circulation 31, no. 5: 1032–37. https://doi.org/10.1161/01.str.31.5.1032.
Aplin, Tammy, Desleigh de Jonge, and Louise Gustafsson. 2013. ‘Understanding the Dimensions of Home that Impact on Home Modification Decision Making’. Australian Occupational Therapy Journal 60, no. 2: 101–109. https://doi.org/10.1111/1440-1630.12022.
Australian Bureau of Statistics. 2012. Year Book Australia, 2012. Canberra: Australian Bureau of Statistics.
Bäckström, Britt, and Karin Sundin. 2009. ‘The Experience of Being a Middle-Aged Close Relative of a Person Who Has Suffered a Stroke, 1 Year after Discharge from a Rehabilitation Clinic: A Qualitative Study’. International Journal of Nursing Studies 46, no. 11: 1475–84. https://doi.org/10.1016/j.ijnurstu.2009.04.009.
Banks, Pauline, and Charlotte Pearson. 2004. ‘Parallel Lives: Younger Stroke Survivors and Their Partners Coping with Crisis’. Sexual and Relationship Therapy 19, no. 4: 413–29. https://doi.org/10.1080/14681990412331298009.
Becker, Gay. 1997. Disrupted Lives: How People Create Meaning in a Chaotic World. Berkeley, CA: University of California Press.
Bendz, Mona. 2003. ‘The First Year of Rehabilitation after a Stroke – from Two Perspectives’. Scandinavian Journal of Caring Sciences 17, no. 3: 215–22. https://doi.org/10.1046/j.1471-6712.2003.00217.x.
Blunt, Alison. 2005. ‘Cultural Geography: Cultural Geographies of Home’. Progress in Human Geography 29, no. 4: 505–15. https://doi.org/10.1191/0309132505ph564pr.
Burton, Christopher R. 2000. ‘Re-Thinking Stroke Rehabilitation: The Corbin and Strauss Chronic Illness Trajectory Framework’. Journal of Advanced Nursing 32, no. 3: 595–602. https://doi.org/10.1046/j.1365-2648.2000.01517.x.
Bury, Michael. 1982. ‘Chronic Illness as Biographical Disruption’. Sociology of Health & Illness 4, no. 2: 167–82. https://doi.org/10.1111/1467-9566.ep11339939.
Carlsson, Gunner E., Anders Möller, and Christian Blomstrand. 2009. ‘Managing an Everyday Life of Uncertainty: A Qualitative Study of Coping in Persons with Mild Stroke’. Disability and Rehabilitation 31, no. 10: 773–82. https://doi.org/10.1080/09638280802638857.
Charmaz, Kathy C. 2007. Constructing Grounded Theory: A Practical Guide through Qualitative Research. Thousand Oaks, CA: Sage.
Cheal, David. 2002. Sociology of Family Life. New York: Palgrave.
Conradson, David. 2005. ‘Landscape, Care and the Relational Self: Therapeutic Encounters in Rural England’. Health & Place 11, no. 4: 337–48. https://doi.org/10.1016/j.healthplace.2005.02.004.
Cott, Cheryl A. 2004. ‘Client-Centred Rehabilitation: Client Perspectives’. Disability and Rehabilitation 26, no. 24: 1411–22. https://doi.org/10.1080/09638280400000237.
Cott, Cheryl A., Rose Wiles, and Rachel Devitt. 2007. ‘Continuity, Transition and Participation: Preparing Clients for Life in the Community Post-Stroke’. Disability and Rehabilitation 29, no. 20–21: 1566–74. https://doi.org/10.1080/09638280701618588.
Curtis, Sarah, Wil Gesler, Kathy Fabian, Susan Francis, and Stefan Priebe. 2007. ‘Therapeutic Landscapes in Hospital Design: A Qualitative Assessment by Staff and Service Users of the Design of a New Mental Health Inpatient Unit’. Environment and Planning C: Government and Policy 25, no. 4: 591–610. https://doi.org/10.1068/c1312r.
Dollard, Joanne, Jacquie Smith, David R. Thompson, and Simon Stewart. 2004. ‘Broadening the Reach of Cardiac Rehabilitation to Rural and Remote Australia’. European Journal of Cardiovascular Nursing 3, no. 1: 27–42. https://doi.org/10.1016/j.ejcnurse.2003.10.002.
Donovan, Rhonda, and Allison Williams. 2007. ‘Home as Therapeutic Landscape: Family Caregivers Providing Palliative Care at Home’. In Therapeutic Landscapes, edited by A. Williams, 199–218. Hampshire, England: Ashgate.
Dow, Briony. 2004. ‘The Shifting Cost of Care: Early Discharge for Rehabilitation’. Australian Health Review 28, no. 3: 260–65. https://doi.org/10.1071/ah040260.
Dow, Briony, and John McDonald. 2007. ‘The Invisible Contract: Shifting Care from the Hospital to the Home’. Australian Health Review 31, no. 2: 193–202. https://doi.org/10.1071/ah070193.
Duff, Cameron. 2015. ‘Atmospheres of Recovery: Assemblages of Health’. Environment and Planning A 48, no. 1: 58–74. https://doi.org/10.1177/0308518x15603222.
Dyck, Isabel, and Parin Dossa. 2007. ‘Place, Health and Home: Gender and Migration in the Constitution of Healthy Space’. Health & Place 13, no. 3: 691–701. https://doi.org/10.1016/j.healthplace.2006.10.004.
English, Jennifer, Kathi Wilson, and Sue Keller-Olaman. 2008. ‘Health, Healing and Recovery: Therapeutic Landscapes and the Everyday Lives of Breast Cancer Survivors’. Social Science & Medicine 67, no. 1: 68–78. https://doi.org/10.1016/j.socscimed.2008.03.043.
Erikson, Anette, Melissa Park, and Kerstin Tham. 2010. ‘Belonging: A Qualitative, Longitudinal Study of What Matters for Persons after Stroke during One Year of Rehabilitation’. Journal of Rehabilitation Medicine 42, no. 9: 831–38. https://doi.org/10.2340/16501977-0608.
Essue, Beverly M., Tanisha Jowsey, Yun-Hee Jeon, Masoud Mirzaei, Carmen L. Pearce-Brown, Clive Aspin, and Tim P. Usherwood. 2010. ‘Informal Care and the Self-Management Partnership: Implications for Australian Health Policy and Practice’. Australian Health Review 34, no. 4: 414–22. https://doi.org/10.1071/ah09795.
Faircloth, Christopher A., Craig Boylstein, Maude Rittman, Mary Ellen Young, and Jaber Gubrium. 2004. ‘Sudden Illness and Biographical Flow in Narratives of Stroke Recovery’. Sociology of Health & Illness 26, no. 2: 242–61. https://doi.org/10.1111/j.1467-9566.2004.00388.x.
Foley, Ronan. 2011. ‘Performing Health in Place: The Holy Well as a Therapeutic Assemblage’. Health & Place 17, no. 2: 470–79. https://doi.org/10.1016/j.healthplace.2010.11.014.
Gallagher, Patti. 2011. ‘Becoming Normal: A Grounded Theory Study on the Emotional Process of Stroke Recovery’. Canadian Journal of Neuroscience Nursing 33, no. 3: 24–32.
Gesler, Wilbert M. 1992. ‘Therapeutic Landscapes: Medical Issues in Light of the New Cultural Geography’. Social Science & Medicine 34, no. 7: 735–46. https://doi.org/10.1016/0277-9536(92)90360-3.
Gesler, Wilbert M. 1996. ‘Lourdes: Healing in a Place of Pilgrimage’. Health & Place 2, no. 2: 95–105. https://doi.org/10.1016/1353-8292(96)00004-4.
Gesler, Wilbert M. 2005. ‘Therapeutic Landscapes: An Evolving Theme’. Health & Place 11, no. 4: 295–297. https://doi.org/10.1016/j.healthplace.2005.02.003.
Graven, Christine, Danielle Sansonetti, Natasha Moloczij, Dominique Cadilhac, and Lynette Joubert. 2013. ‘Stroke Survivor and Carer Perspectives of the Concept of Recovery: A Qualitative Study’. Disability and Rehabilitation 35, no. 7: 578–85. https://doi.org/10.3109/09638288.2012.703755.
Greenwood, Nan, Ann Mackenzie, Geoffrey C. Cloud, and Nikki Wilson. 2009. ‘Informal Primary Carers of Stroke Survivors Living at Home–Challenges, Satisfactions and Coping: A Systematic Review of Qualitative Studies’. Disability and Rehabilitation 31, no. 5: 337–51. https://doi.org/10.1080/09638280802051721.
Gomersall, Tim, and Anna Madill. 2015. ‘Chronotope Disruption as a Sensitizing Concept for Understanding Chronic Illness Narratives’. Health Psychology 34, no. 4: 407–16. https://doi.org/10.1037/hea0000151.
Gubrium, Jaber F., Maude R. Rittman, Christine Williams, Mary Ellen Young, and Craig A. Boylstein. 2003. ‘Benchmarking as Everyday Functional Assessment in Stroke Recovery’. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 58, no. 4: S203–11. https://doi.org/10.1093/geronb/58.4.s203.
Hand, Martin, and Elizabeth Shove. 2004. ‘Orchestrating Concepts: Kitchen Dynamics and Regime Change in Good Housekeeping and Ideal Home, 1922–2002’. Home Cultures 1, no. 3: 235–56. https://doi.org/10.2752/174063104778053464.
Healey-Ogden, Marion J. 2013. ‘Being “at Home” in the Context of Home Care’. Home Health Care Management & Practice 26, no. 2: 72–79. https://doi.org/10.1177/1084822313508646.
Heaton, Janet. 1999. ‘The Gaze and Visibility of the Carer: A Foucauldian Analysis of the Discourse of Informal Care’. Sociology of Health & Illness 21, no. 6: 759–77. https://doi.org/10.1111/1467-9566.00182.
Henderson, Julie. 2005. ‘Neo-liberalism, Community Care and Australian Mental Health Policy’. Health Sociology Review 14, no. 3: 242–54. https://doi.org/10.5172/hesr.14.3.242.
Hoyez, Anne-Cécile. 2007. ‘The “World of Yoga”: The Production and Reproduction of Therapeutic Landscapes’. Social Science & Medicine 65, no. 1: 112–24. https://doi.org/10.1016/j.socscimed.2007.02.050.
Johansson, Karin, Staffan Josephsson, and Margareta Lilja. 2009. ‘Creating Possibilities for Action in the Presence of Environmental Barriers in the Process of “Ageing in Place”’. Ageing and Society 29, no. 1: 49–70. https://doi.org/10.1017/s0144686x08007538.
Lawrence, Maggie, and Sue Kinn. 2013. ‘Needs, Priorities, and Desired Rehabilitation Outcomes of Family Members of Young Adults Who Have Had a Stroke: Findings from a Phenomenological Study’. Disability and Rehabilitation 35, no. 7: 586–95. https://doi.org/10.3109/09638288.2012.711895.
Laws, Jennifer. 2009. ‘Reworking Therapeutic Landscapes: The Spatiality of an “Alternative” Self-Help Group’. Social Science & Medicine 69, no. 12: 1827–33. https://doi.org/10.1016/j.socscimed.2009.09.034.
Manderson, Lenore, and Narelle Warren. 2013. ‘“Caring for” and “Caring about”: Embedded Interdependence and Quality of Life’. In Reframing Disability and Quality of Life: A Global Perspective, edited by Narelle Warren, and Lenore Manderson, 179–94. Dordrecht: Springer.
Martin, Graham P., Susan A. Nancarrow, Hilda Parker, Kay Phelps, and Emma L. Regen. 2005. ‘Place, Policy and Practitioners: On Rehabilitation, Independence and the Therapeutic Landscape in the Changing Geography of Care Provision to Older People in the UK’. Social Science & Medicine 61, no. 9: 1893–904. https://doi.org/10.1016/j.socscimed.2005.04.001.
Mayes, Rachel, Rosemary Cant, and Lindy Clemson. 2010. ‘The Home and Caregiving: Rethinking Space and Its Meaning’. OTJR: Occupation, Participation, Health 31, no. 1: 15–22. https://doi.org/10.3928/15394492-20100122-01.
Mayo, Nancy E., Sharon Wood-Dauphinee, Robert Côté, David Gayton, Joseph Carlton, Joanne Buttery, and Robyn Tamblyn. 2000. ‘There’s No Place Like Home: An Evaluation of Early Supported Discharge for Stroke’. Stroke; A Journal of Cerebral Circulation 31, no. 5: 1016–23. https://doi.org/10.1161/01.STR.31.5.1016.
McCarthy, Michael J., and Elizabeth Bauer. 2015. ‘In Sickness and in Health: Couples Coping with Stroke Across the Life Span’. Health Social Work 40, no. 3: e92–100. https://doi.org/10.1093/hsw/hlv043.
Meijering, Louise, Ant T. Lettinga, Christa S. Nanninga, and Christine Milligan. 2016. ‘Interpreting Therapeutic Landscape Experiences through Rural Stroke Survivors’ Biographies of Disruption and Flow’. Journal of Rural Studies, online 11 June. https://doi.org/10.1016/j.jrurstud.2016.06.004.
Meijering, Louise, Christa S. Nanninga, and Ant T. Lettinga. 2016. ‘Home-Making after Stroke. A Qualitative Study among Dutch Stroke Survivors’. Health & Place 37: 35–42. https://doi.org/10.1016/j.healthplace.2015.11.006.
Milligan, Christine. 2009. There’s No Place Like Home: Place and Care in an Ageing Society. Farnham, UK: Ashgate Publishing.
Milligan, Christine, and Amanda Bingley. 2007. ‘Restorative Places or Scary Spaces? The Impact of Woodland on the Mental Wellbeing of Young Adults’. Health and Place 13 no. 4: 799–811. https://doi.org/10.1016/j.healthplace.2007.01.005.
Milligan, Christine, Anthony Gatrell, and Amanda Bingley. 2004. ‘“Cultivating Health”: Therapeutic Landscapes and Older People in Northern England’. Social Science & Medicine 58, no. 9: 1781–93. https://doi.org/10.1016/S0277-9536(03)00397-6.
Moore, Andrew J., Christine Anderson, Bernie Carter, and Jane Coad. 2010. ‘Appropriated Landscapes: The Intrusion of Technology and Equipment into the Homes and Lives of Families with a Child with Complex Needs’. Journal of Child Health Care 14 no. 1: 3–5. https://doi.org/10.1177/1367493509360275.
Moore, Andrew J., Bernie Carter, Anne Hunt, and Kay Sheikh. 2013. ‘“I Am Closer to This Place” – Space, Place and Notions of Home in Lived Experiences of Hospice Day Care’. Health & Place 19: 151–58. https://doi.org/10.1016/j.healthplace.2012.11.002.
Mortenson, Ben W., Andrew Sixsmith, and Robert Beringer. 2016. ‘No Place Like Home? Surveillance and What Home Means in Old Age’. Canadian Journal on Aging 35, no. 1: 103–14. https://doi.org/10.1017/S0714980815000549.
Moser, Ingunn. 2005. ‘On Becoming Disabled and Articulating Alternatives’. Cultural Studies 19, no. 6: 667–700. https://doi.org/10.1080/09502380500365648.
Nanninga, Christa S., Louise Meijering, Marleen C. Schönherr, Klaas Postema, and Ant T. Lettinga. 2014. ‘Place Attachment in Stroke Rehabilitation: A Transdisciplinary Encounter Between Cultural Geography, Environmental Psychology and Rehabilitation Medicine’. Disability and Rehabilitation 37, no. 13: 1125–34. https://doi.org/10.3109/09638288.2014.955136.
Navaie-Waliser, Maryam, Aubrey Spriggs, and Penny H. Feldman. 2002. ‘Informal Caregiving: Differential Experiences by Gender’. Medical Care 40, no. 12: 1249–59. https://doi.org/10.1097/00005650-200212000-00012.
Pavey, Amanda, Narelle Warren, and Jacquelyn Allen-Collinson. 2015. ‘“It Gives Me My Freedom”: Technology and Responding to Bodily Limitations in Motor Neuron Disease’. Medical Anthropology 34, no. 5: 442–55. https://doi.org/10.1080/01459740.2015.1035782.
Pearson, Mark, Harriet Hunt, Chris Cooper, Sasha Shepperd, Ray Pawson, and Rob Anderson. 2012. Intermediate Care: A Realist Review and Conceptual Framework: Final Report. Southampton, UK: National Institute for Health Research, Service Delivery and Organisation Programme.
Pollack, Michael. R., and Peter B. Disler. 2002. ‘2: Rehabilitation of Patients after Stroke’. The Medical Journal of Australia 177, no. 8:452–56.
Pound, Pandora, Patrick Gompertz, and Shah Ebrahim. 1998. ‘Illness in the Context of Older Age: The Case of Stroke’. Sociology of Health & Illness 20, no. 4: 489–506. https://doi.org/10.1111/1467-9566.00112.
Pritchard, Elizabeth, Narelle Warren, Anna Barker, Ted Brown, and Terry Haines. 2015. ‘Personal Life Approach: An Interactive Way of Understanding Older Adults’ Participation in Activities Following Hospitalization’. Gerontologist 56, no 3: 504–13. https://doi.org/10.1093/geront/gnu115.
Quinn, Karen, Craig Murray, and Caroline Malone. 2014. ‘Spousal Experiences of Coping with and Adapting to Caregiving for a Partner Who Had a Stroke: A Meta-synthesis of Qualitative Research’. Disability and Rehabilitation 36, no. 3: 185–98. https://doi.org/10.3109/09638288.2013.783630.
Rowles, Graham D. 2000. ‘Habituation and Being in Place’. OTJR:Occupation, Participation and Health 20, no. 1 (suppl): 52S–67S. https://doi.org/10.1177/15394492000200S105.
Rowles, Graham D. 2008. ‘Place in Occupational Science: A Life Course Perspective on the Role of Environmental Context in the Quest for Meaning’. Journal of Occupational Science 15 no. 3, 127–35. https://doi.org/10.1080/14427591.2008.9686622.
Sakellariou, Dikaios. 2015. ‘Home Modifications and Ways of Living Well’. Medical Anthropology 34, no. 5: 456–69. https://doi.org/10.1080/01459740.2015.1012614.
Salter, Katherine, Chelsea Hellings, Norine Foley, and Robert Teasell. 2008. ‘The Experience of Living with Stroke: A Qualitative Meta-synthesis’. Journal of Rehabilitation Medicine 40, no. 8: 595–602. https://doi.org/10.2340/16501977-0238.
Sixsmith, Judith, Andrew Sixsmith, Agneta Malmgren Fänge, Doerte Naumann, Csaba Kucsera, Signe Tomsone, Maria Haak, Synneve Dahlin-Ivanoff, and Ryan Woolrych. 2014. ‘Healthy Ageing and Home: The Perspectives of Very Old People in Five European Countries’. Social Science & Medicine 106: 1–9. https://doi.org/10.1016/j.socscimed.2014.01.006.
Seymour, Wendy. 2002. ‘Time and the Body: Re-embodying Time in Disability’. Journal of Occupational Science 9, no. 3: 135–42. https://doi.org/10.1080/14427591.2002.9686501.
Tamm, Maare. 1999. ‘What Does a Home Mean and When Does It Cease to Be a Home? Home as a Setting for Rehabilitation and Care’. Disability and Rehabilitation 21, no. 2: 49–55. https://doi.org/10.1080/096382899297963.
Tanner, Bronwyn, Cheryl Tilse, and Desleigh de Jonge. 2008. ‘Restoring and Sustaining Home: The Impact of Home Modifications on the Meaning of Home for Older People’. Journal of Housing for the Elderly 22, no. 3: 195–215. https://doi.org/10.1080/02763890802232048.
Thrift, Amanda G., Helen M. Dewey, Jonathan W. Sturm, Velandai K. Srikanth, Amanda K. Gilligan, Seana L. Gall, Richard A. L. MacDonell, John J. McNeil, and Geoffrey A. Donnan. 2009. ‘Incidence of Stroke Subtypes in the North East Melbourne Stroke Incidence Study (NEMESIS): Differences Between Men and Women’. Neuroepidemiology 32, no. 1: 11–18. https://doi.org/10.1159/000170086.
Timmermans, Stefan, and Iddo Tavory. 2012. ‘Theory Construction in Qualitative Research: From Grounded Theory to Abductive Analysis’. Sociological Theory 30, no. 3: 167–86. https://doi.org/10.1177/0735275112457914.
Tyreman, S. 2011. ‘Homelikeness and Health: An Introduction to the Theme’. Medicine, Health Care and Philosophy 14, no. 3: 287–89. https://doi.org/10.1007/s11019-011-9315-2.
Vanhook, Patricia. 2009. ‘The Domains of Stroke Recovery: A Synopsis of the Literature’. Journal of Neuroscience Nursing 41, no. 1: 6–17. https://doi.org/10.1097/JNN.0b013e31819345e4.
Wakefield, Sarah, and Colin McMullan. 2005. ‘Healing in places of decline: (Re)imagining Everyday Landscapes in Hamilton, Ontario’. Health & Place 11, no. 4: 299–312. https://doi.org/10.1016/j.healthplace.2004.05.001.
Walters, Darren L., Antti Sarela, Anita Fairfull, Kylie Neighbour, Cherie Cowen, Belinda Stephens, Tom Sellwood, Bernadette Sellwood, Marie Steer, Michelle Aust, Rebecca Francis, Chi-Keung Lee, Sheridan Hoffman, Gavin Brealey, and Mohan Karunanithi. 2010. ‘A Mobile Phone-based Care Model for Outpatient Cardiac Rehabilitation: The Care Assessment Platform (CAP)’. BMC Cardiovascular Disorders 10: 5. https://doi.org/10.1186/1471-2261-10-5.
Warren, Narelle. 2009. Markers of Midlife: Interrogating Health, Illness and Ageing in Rural Australia. Saarbrücken, Germany: Lambert Academic Publishing.
Warren, Narelle, and Lenore Manderson. 2008. ‘Constructing Hope: Dis/continuity and the Narrative Construction of Recovery in the Rehabilitation Unit’. Journal of Contemporary Ethnography 37, no. 2: 180–201. https://doi.org/10.1177/0891241607312493.
Wiles, Janine L., Annette Leibing, Nancy Guberman, Jeanne Reeve, and Ruth E. S. Allen. 2012. ‘The Meaning of “Ageing in Place” to Older People’. Gerontologist 52: 357–66. https://doi.org/10.1093/geront/gnr098.
Williams, Allison. 1999. Therapeutic Landscapes: The Dynamic between Wellness and Place. Lanham, MD: University Press of America.
Williams, Allison. 2002. ‘Changing Geographies of Care: Employing the Concept of Therapeutic Landscapes as a Framework in Examining Home Space’. Social Science & Medicine 55, no. 1: 141–54. https://doi.org/10.1016/S0277-9536(01)00209-X.
Williams, Allison. 2004. ‘Shaping the Practice of Home Care: Critical Case Studies of the Significance of the Meaning of Home’. International Journal of Palliative Nursing 10, no.7: 333–42. https://doi.org/10.12968/ijpn.2004.10.7.14575.
Williams, Allison. 2007. Geographies of Health: Therapeutic Landscapes. London: Ashgate Publishers.
Wood Victoria J., Sarah E. Curtis, Wil Gesler, Ian H. Spencer, Helen J. Close, James Mason, and Joe G. Reilly. 2013. ‘Creating “Therapeutic Landscapes” for Mental Health Carers in Inpatient Settings: A Dynamic Perspective on Permeability and Inclusivity’. Social Science & Medicine 91: 122–29. https://doi.org/10.1016/j.socscimed.2012.09.045.
Yates-Doerr, Emily, and Megan Carney. 2016. ‘Demedicalizing Health: The Kitchen as a Site of Care’. Medical Anthropology 35, no. 4: 305–21. https://doi.org/10.1080/01459740.2015.1030402.
Endnotes
1 Back
The median age of first-ever stroke in Australia is seventy-two for men and seventy-seven for women (Thrift et al. 2009).
2 Back
Alix and her family had to move house after Erwin’s stroke. The mortgage was too expensive with the reduced household income, maintenance of the property was too burdensome for Alix, the house was sited on a slope, and it was too difficult for Erwin to manoeuvre in the house. They bought a much smaller house on flat land.