‘They overworked us’
Humiliation and claims to recognition of volunteer nurses in the aftermath of the Ebola epidemic in Sierra Leone
—
Abstract
Introduction
In August 2016, a few months after the Ebola epidemic in Sierra Leone was officially declared over, I met Fatmatu[note 1] and some of her colleagues at a hospital in Freetown with the aim of talking about the changes in the country’s health care system. There is broad agreement that the weak health care systems of Sierra Leone, Liberia, and Guinea were unprepared to contain the Ebola outbreak, which facilitated the accelerated spread of the virus, wreaking havoc in the three countries (Beisel 2014; Abramowitz 2014; cf. Richards 2016). In Sierra Leone alone, approximately ten thousand people contracted the virus in the course of the prolonged epidemic, which lasted from 2014 until 2016. Around four thousand lost their lives. Prominent global health experts such as Peter Piot (2014) have concluded that stronger health care systems are a precondition for achieving global health. In Sierra Leone, health workers play a crucial role toward this goal, as they carry most of the burden of providing professional care at hospitals and rural health units (Wurie, Samai, and Witter 2016). Thus, when I talked to Fatmatu and her colleagues, I presumed that the announced restructuring of the health care system would improve their working conditions. But, as this article shows, I was completely mistaken in my assumption about health workers.
According to various medical anthropologists, the role of health workers in African countries cannot be grasped using the categories and definitions that prevail in human resource management discourses (see, for example, Geissler 2012; Brown and Prince 2015; Prince and Brown 2016a). Most notably, as Ruth Prince and Hannah Brown argue (2015), such categories fail to recognize the large number of invisible volunteers, who are not paid but whose voluntary labor is essential for maintaining health systems in many African countries (Brown and Prince 2015). Indeed, when I asked Fatmatu and her colleagues if they were receiving a decent pay, assuming that this would be an important dimension of their working conditions, they answered flatly, ‘We are volunteers’. They were not paid a wage although they had been trained as nurses and worked like any other nurse on the payroll. Shouting in anger, they added that they had to pay for their own transportation to get to work. Others simply walked: ‘I use my own rubber tires’, George joked, pointing to his shoes.
Fatmatu and her colleagues had been volunteering at holding centers and Ebola treatment units (ETUs) across Sierra Leone during the epidemic, working, as they put it, for the ‘sake of the country’. During the heat of the epidemic, the country’s president had promised, as an attempt to motivate volunteer nurses to keep working in the ETUs, that they would receive a formal employment contract once the Ebola epidemic ended. However, after the last holding centers and ETUs had been closed, the nurses were still waiting desperately for that promise to be fulfilled. The nurses were upset when the promise of being ‘absorbed into the system’ was not fulfilled, telling me, ‘We will never forget what they did to us’.
At first I was not sure how these comments and the situation should be understood: Were such working conditions not typical for under-resourced health care systems in the global South? Can one count on promises made by the government? Was the angry response of volunteer nurses, holding on to these promises, an emotional overreaction? Should both the promises of the government and the anger of the volunteer nurses be taken with a grain of salt?
My subsequent conversations with volunteer nurses suggested otherwise. Just a few days after our first conversation, I met Fatmatu again at the hospital triage area, where she was selling shoes to her colleagues. She explained apologetically, ‘This is what I am doing to make a living’. Such extra income-generating activities had become a matter of public controversy in the country after the end of the Ebola outbreak in 2016, and the Ministry of Health and Sanitation ordered hospitals to remove all volunteer nurses from their premises. The volunteer nurses were shocked, infuriated, and humiliated by this new order, which, they felt, epitomized the way their government had treated them.
Moral emotions and misrecognition
To explain the volunteer nurses’ responses, I argue that neither existing understandings of voluntary labor nor moral theories of justice capture the effects of institutional humiliation. There are two aspects of this argument: first, this type of volunteerism cannot be accounted for by modernist notions of work, labor, and employment, which impute that voluntary labor is a personally satisfying way of spending one’s leisure time (Prince and Brown 2016b). Rather, the motives of Sierra Leonean nurses to volunteer in the ETUs and more generally to start their careers at hospitals as volunteer nurses are multiple: gaining work experience, fashioning a productive self, or receiving occasional payments through donor-funded projects. Most importantly, volunteering is motivated by a hope that one’s work will be at one point rewarded with permanent employment. When the volunteer nurses were told to stop working and leave the wards immediately, they may not have been wronged in a legal sense. But this perspective is too narrow because it does not consider how this dismissal negated the volunteers’ claims for recognition (Prince 2015). As I aim to show, they felt they were treated disrespectfully, especially after they had risked their lives in the ETUs, doing work that no one else was willing to do.
Secondly, drawing on recent anthropological discussions of volunteers, health workers, and the problem of recognition (Prince 2015; Street 2016), this article focuses on humiliation as an extreme form of misrecognition, in order to grasp the feelings of injustice experienced by volunteer nurses. Following philosophical and anthropological works on recognition and ethics, I argue that these feelings of humiliation are more than simply subjective responses. These feelings are moral emotions identifying and ‘validating’ the injuries resulting from suppressed or denied claims to recognition (Honneth 1996; Fraser and Honneth 2003; Keane 2016).
According to the philosopher Axel Honneth (1996, 2007), humiliation can be understood as an intense form of experiencing disrespect that shows how the desire for social recognition is a fundamental human vulnerability.[note 2] The philosopher Avishai Margalit (2009) considers a ‘decent society’ to be one that does not humiliate those who depend on its institutions. Not all kinds of maltreatment, however, can be seen as humiliation. Instead, humiliation refers specifically to those practices of denigration and disrespectful attitudes that damage a person’s sense of self-respect (Margalit 2009, 288). The way one is treated, the words that are uttered, and those that are not said shape the experience of humiliation. As Judith Butler (1997) argues forcefully, words are not just a means of representation but can injure and humiliate in the moment of their utterance by subordinating the addressee.
Margalit’s (2009) definition of humiliation and Honneth’s (1996; 2007) work on social recognition lead us to understand that humiliation cannot be grasped within existing moral theories of justice, which are used to justify global health interventions (Pogge 2002, 2005).[note 3] Following Webb Keane’s (2016) call for an anthropology of ethics, I wish to emphasize that humiliation is a matter of sensibility (Margalit 2009; see also Throop 2012), an affect through which those who are humiliated register and validate the maltreatment they have been undergoing. Following this sensibility allows us to see how the social exclusion of nurse volunteers from hospitals was experienced as a rejection of their common humanity (summarized in the sentiment that ‘no one should be treated that way’). My hope is that this discussion, drawing on this scholarly body of work on humiliation, will direct our attention to the question of how global health might contribute to building of decent institutions.
Research methodology
This paper draws on interviews conducted between July and August 2016 in the course of an ongoing collaborative field research project on frontline health workers in the aftermath of the Ebola epidemic in Sierra Leone. The main part of my discussion of humiliation draws on focus group discussions with volunteer nurses who had been working in the ETUs and had been formally trained as nurses. While this article does not address the experience of sprayers, cleaners, burial boys, ambulance drivers, and other frontline health workers active in the Ebola response, I hope that it alerts us to the highly uneven distribution of recognition of the large number people whose contribution brought the Ebola epidemic to an end.
The focus group discussions were conducted in the course of doing collaborative field research for the project ‘Trust in medicine after the EVD epidemic’.[note 4] These focus group discussions were not planned as part of the original research design, but Fatmatu connected our research group to several of her dismissed colleagues, and we decided to organize conversations about their experiences. Four focus group discussions were conducted, with four to eight volunteer nurses participating in each. In addition, my exploration of humiliation includes eight key informant interviews with health workers and public health officials in Freetown, Bo District, and Kenema District.
Participant observation in hospitals was also conducted in the course of the field research, but is not discussed in this account of volunteer nurses and their experiences of humiliation. I agree with Claire Waterton and Brian Wynne (1999) that focus group discussions are not to be mistaken for a method that captures participants’ deepest beliefs and values.[note 5] Instead, focus group discussions show that the formation of emotions, beliefs, and ideas is relational (ibid.). In this sense, the data presented here attempts to capture the dynamics of recalling and reenacting the feelings of pain and anger. Our interlocutors demanded that we try to imagine the shock they felt when they had been told to leave the hospital. This demand, I suggest, essentially appeals to sensibilities about their experience rather than persuasion about the causes of their exclusion.
Pin-code nurses, volunteer nurses, and ‘appreciation’
There is no clear account of how many volunteer nurses work in the health care system in Sierra Leone. A survey conducted by UNICEF at the height of the Ebola outbreak in 2014 counted 3,500 registered health workers (nurses, midwives, maternal and child health aides, community health officers) for the 1,136 primary health care units in the country. Next to this group of formally employed health workers, the report captured 2,039 ‘other health personnel’, 4,544 ‘other non-technical staff’, and 10,993 community health workers, none of whom were paid a salary by the government (UNICEF 2014, 44).
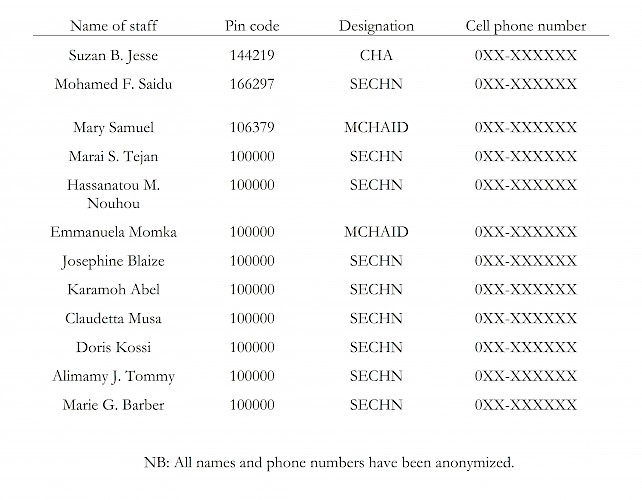
To give an idea of the ratio of unpaid to paid nurses it is helpful to take a brief look at one of the staff lists of a typical primary health unit (see table 1). At this primary health unit only three nurses were on the government’s payroll; the rest were all volunteers. The pin codes, in the second column, were widely used to distinguish between paid and unpaid staff. In this list, salaried nurses were given a unique six-digit pin code, while all volunteers were given the number ‘100000’. In everyday conversations health workers used the term ‘pin code nurses’ to refer to salaried nurses, and volunteers phrased their demands for a formal employment with the question: ‘When do they give us a pin code?’ All health workers of this hospital, whether on payroll or not, were trained in nursing. Most had been certified either as a ‘state enrolled community health nurse’ (SECHN) or as a ‘maternal child health aid’ (MCHAID). Only one health worker held a diploma as a ‘community health assistant’ (CHA); no one at this rural primary health unit held the higher diploma of ‘state registered nurse’ (SRN).
The ratio of paid and unpaid nurses is characteristic for the larger region, where volunteers are the ‘human infrastructure of development and health programs’ (Prince 2015, 86).[note 6] As Frederica, one of the volunteer nurses, stressed: ‘We don’t work like you people know: when you work in hours you get paid by hours. [Here] when they say your payment is US$100 for the month, you work morning till night for US$100. Unless you change your paper and add education to the paper you had’.
In terms of the workload, having a nursing certificate versus a degree did not make a difference. ‘It is just on the paper’, as my interlocutors insisted. In smaller rural health facilities, everyone had to do everything. In fact, as the following sections will elaborate in more detail, volunteer nurses perceived themselves as working more than pin-code nurses. They could not afford not to volunteer, if they wanted to be formally employed in the future. Indeed, the matrons of the hospitals (also called the ‘in-charge nurse’) taught them, as Sia put it, ‘[we] had to work harder than the salaried nurses, [we] had to surpass them’, in order to be absorbed into the system at some point.
Public health officials in Freetown, whom I questioned about volunteers’ demands for formal employment, surmised that there was confusion among volunteers, that they didn’t understand that voluntarism neither implies payment nor future employment. Anthropologists, by contrast, have shown that the confusion is not in the volunteers’ expectations, but rather reflects a fundamental contradiction in the field of global health (Kelly and Geissler 2011). According to Prince and Brown (2016b), the modernist distinction between salaried labor and volunteering as a way of spending one’s free time does not apply to all forms of volunteering. Instead, as the authors note, in a context of chronic unemployment, volunteering ‘becomes a space in which those who are excluded from the arenas of work, or in a marginal position in relation to labor markets, can gain public recognition and presence’ (Prince and Brown 2016b, 22).
During the Ebola epidemic, volunteers working in hospitals or designated holding centers and ETUs received a ‘risk allowance’ from the government ranging from 800,000 to 1,000,000 Sierra Leonean Leone (SLL) per month (between US$180 and US$200). Risk allowances had been increased to these levels, which significantly exceeded the normal salary of nurses, after volunteer nurses went on strike. One volunteer nurse, Mariatu, defended the nurses’ demands for an adequate risk allowance by noting her humanitarian reasons and her commitment to the job: ‘I wouldn’t work if I didn’t have humanitarian reasons. Because we have immaterial [non-monetary] feelings, we know that we have to commit ourselves to do the job, so we did it … and we did it very well’.
I asked Foday if he believed that his work in the ETU was recognized. His response illuminates how financial remuneration and public recognition are inextricably linked as ‘appreciation’: ‘People will say, “This man works for money: they give him a lot of money, that is why he was working”. Others will say, “This man is a good man. He took a risk during the outbreak; he worked for the country and he was around trying to put things in place”. People will appreciate you’. The term ‘appreciation’ covers a broad range of meanings and practices in the absence an adequate income. Volunteer nurses and salaried nurses may expect various kinds of remuneration from organizations and patients (per diem stipends, small payments, gifts, etc.) in order to survive. Before the Ebola epidemic, both salaried and volunteer nurses had taken such payments for granted, which they described as a show of appreciation and a way for patients to say ‘thank you’.
The ambivalence of ‘appreciation’, encompassing both financial payments and words of gratitude, underscores how voluntary labor reveals ‘site[s] of struggles about identity, social value, and recognition, in particular, as most of these claims to recognition often remain unfulfilled’ (Prince 2015, 86). Volunteer nurses who had worked in the ETUs missed the recognition they were expecting: to be given pin codes as formally employed nurses. When I asked Frederica if she believed that nurses were valued, she answered angrily that they had been exploited and abused as volunteers: ‘They overworked us. After being trained for four years, nothing … not in payroll. We need to have our own apartment for ourselves … standard life as a nurse. That would make us happy. Who can we turn to?’ In this statement, Frederica expressed her feeling that nobody was recognizing the injustice of forcing volunteer nurses out of the hospitals.
In order to understand this injustice, it is necessary to examine the injuries resulting from the unfulfilled claims to recognition. The flipside of social recognition, as Honneth (1996, 2007) lays out, is the experience of disrespect in the form of insults, denigration, and abuse. According to Margalit (2003), humiliation is an extreme form of disrespectful treatment, since it impairs the fundamental experience of self-respect.
Weighing work and words
When I asked the volunteer nurses why they had been dismissed from the hospitals, they first responded that they really did not know or understand what had happened. Other volunteer nurses had received a memo the month before that stated that all volunteer nurses were to ‘stop working with immediate effect’. Some of the volunteers did not immediately realize the import of this memo. Aminata, one of the volunteer nurses, recounted:
We thought it was just something that could be amended within a few days’ time. So, we checked. After two, three days we checked again, hoping the problem would have been resolved. But last time we went [to the hospital] it was still the same. In fact, it was even worse. If we are caught there we will be in trouble. By then we decided to sit down [stay at home], without attempting to go there for work.
None of them could give the precise reason for this decision. The volunteer nurses insisted that what they knew was only hearsay and rumors. This was, in their eyes, part of the problem: they had not received a proper explanation to which they could have reacted. They had heard that a volunteer nurse had been complaining that they were the only ones working on the hospital wards, and this complaint had incited an investigation, which brought a broad range of malpractices to light.
The Sierra Leone Telegraph reported in September of 2016 on an investigation that found:
there is a culture of laissez faire and corruption by nurses and paramedical staff who often turn down appeals to treat dying patients because they cannot pay bribes. Nurses speak to their patients in very harsh tones and would not attend to them on time if none of them knows or is related to them. Nurses at the Ear, Nose and Throat Department including the Eye Clinic, collect money from patients before issuing them registration cards and deceive people into believing that it is a normal and legal practice. (Thomas 2016)
‘And it is not a lie’, one of the volunteers acknowledged, ‘the pin-code nurses are doing their things. But at the end of the month, they will go and receive a salary’. According to the volunteer nurses, officials had been compelled by the results of the investigation to prohibit volunteers from doing the work of employed nurses. Aminata told me: ‘They [pin-code nurses] have relaxed because the volunteers are working. So they decided to stop volunteers so that the pin code nurses [would] work’.
The volunteer nurses understood well why their salaried colleagues were frequently absent. Their meager salary, the rapidly increasing cost of living, and other everyday problems did not motivate them to go to work. The volunteers had the same problems, but they could not just ‘go to the in-charge [nurse] and make excuses’ as the nurses on salary supposedly did.
Indeed, the volunteers perceived themselves as working harder and being more reliable, in comparison to the nurses on the payroll, while suffering under the same economic and financial constraints. Without an income, they could not even pay for the transport to get to work. But if they did not arrive on time to sign in with the matron, they would be marked as absent for the day. Sia explained, ‘For us, if you are absent for a day, oh, they will keep shouting your name. “You were the people that were meant to come to work”’.
One might expect the situation to change in the near future, as donor funding is pouring into the country to rebuild the health care system. Some volunteer nurses had heard that the government might ‘give a pin code’ to the volunteers in 2018. But such rumors only aggravated their anger. Aminata exclaimed: ‘Imagine, we have been volunteering for three years. Three years! No transport allowance, no nothing. We walk to the hospitals’. Sia continued: ‘Imagine from 2012 up to now, no salary, no pin code. Maybe politicians’ talk. We heard they are going to give, they did not say they are giving’.
As the volunteers explained, most of them had started to volunteer at a hospital in 2013 and 2014. They described the pin code situation as resulting from competition: the nursing schools in the country were simply producing too many nurses in relation to the number of existing paid posts. The chances of being formally employed and of receiving a pin code were better for nurses with a degree and for midwives. Thus nurses with a certificate declaring them a ‘state enrolled community nurse’ pursued a higher diploma as ‘state registered nurse’ to increase their chances. But going for a higher diploma meant additional costs. As students, they had to pay a tuition fee of three million Sierra Leonean Leone (approximately US$650) each year for three years of study, in addition to the fee of about SLL300,000 (approximately US$65) to obtain a nursing license that allowed one to practice at a hospital.
But even nurses with advanced degrees had difficulties. The whole employment process was very informal. Everyone had to start as a volunteer before receiving a pin code. One of the nurses on salary, whom I asked to describe her employment process, ironically deemed herself to be lucky for having sacrificed two months of salary only to bribe officials to get a pin code. Others had to pay even more, as she pointed out. The amount to be paid apparently depended on one’s connections and negotiating position.
During the Ebola outbreak, when volunteer nurses were promised that they would receive a pin code if they went to work in the ETUs, this seemed to be an opportunity to be seized. As Fatu, one the volunteers who had gone to the ETUs, recounted: ‘They promised us faithfully that after Ebola they are going to give us a pin code, and a package’. They all remembered the exact date of this promise, 19 September 2014, whereupon they had agreed and had undergone three days of training before going to work in one of the ETUs. They quietly recalled their own naiveté in trusting the government’s promise that they would receive a pin code. When the volunteer nurses did not receive a pin code after the work at the ETUs had ended, instead of protesting they started to volunteer at the hospitals. Aminata said, we ‘told ourselves quietly “let’s just work”’.
When one is degraded
After the last ETUs were closed in March 2016, many of the volunteers waited desperately to be put on the government payroll system. Not all returned to volunteer at the hospitals; some, for instance, were lucky to find a job with a nongovernmental organization. But some did decide to return, instead of ‘sitting at home and doing nothing’, as Frederica said. They went back and volunteered again on the wards. Fatu recalled: ‘We never complained. We still appreciate the work because after training you need to improve your skills. We love our job. Sitting at home will not make you understand. Because nursing is an everyday practice. The more you are involved, the more you get an experience’.
Furthermore, they continued to work hard despite not having received a pin code. Aminata said, ‘We started working there, we don’t give problems. Though you will find that one or two people will give problems. But the majority of us, we devote ourselves to work, we keep time, even though we don’t get a salary, because we want to improve ourselves. We want to know much about this nursing’.
So when the volunteers in the hospitals heard that a memo was out instructing all volunteer nurses to leave the hospitals immediately, they were shocked:
Frederica: It was a surprise for me to hear that there was a memo out there saying we have to stop working. As for me, I was shocked.
Aminata: Yes. Because this was not our … our agreement.
Frederica: … After three years, the only thing we hear is that all volunteers have to stop.
The volunteers were not only grieving over the unfulfilled promise of formal employment that would give a meager, irregularly paid, but at least permanent income. They also felt humiliated because they had been told to leave the hospitals simply by way of a memo, without even a meeting in which the memo was explained to them. They felt that they did not deserve such disrespectful treatment, after having risked their lives at the ETUs.
The volunteer nurses described being dismissed from the hospital in the following words.
Fatu: I want to say something: when this memo came out, as for my opinion, the institution had to call us for a meeting, explain to us why this happened, but they never did. They just go and post the memo: ‘All volunteers out, with immediate effect’. So it is like there is no regard for us. It is embarrassing!
Sung-Joon Park: Embarrassing?
Sia: Very, very disgraceful.
Aminata: Yes!
Fatu: Painful! We will never forget what they did to us… . There is no ‘Thank you’, there is only disgrace, there is shame.
Fatu: They maltreated us!
SJP: And you think nobody should do that? You would not treat someone else like this?
Fatu: It is not decent to treat someone like that. Especially if you know that people are hard working. If someone has been working, at least they deserve some amount of respect.
To describe the humiliation, they pointed to the fact that the relatives of colleagues who had lost their lives during the Ebola epidemic were not compensated. They recalled angrily how public authorities accused a colleague who had been infected in the ETUs of being careless. Health workers had felt enormous emotional stress from various sides as they worked hard to treat the sick: landlords had threatened to throw them out of their homes; they made up excuses when they went to work in the ETUs because their families had been scared; and some were too scared to even touch their own children (McMahon et al. 2016). The volunteers explained that they worked out of love for their country, which seemed like a bad joke after their dismissal. But not everyone took it with irony. One nurse described in an empty tone how her friend had to remind her again and again not to forget that her life had a meaning for the country.
The humiliation experienced by volunteer nurses reflects an extreme form of misrecognition. In addition to the order to leave the hospital, the way they were treated created feelings of disrespect and humiliation. Promises were broken and, more importantly, it appeared that nobody was willing to recognize their work at the ETUs. What made this maltreatment a form of institutional humiliation was the fact that the volunteer nurses were essentially excluded from the system of recognition from which their sense of respect and worth depended.
What appreciation means
Volunteer nurses were dismissed from the hospitals because they were not paid and therefore suspected of attempting to extract money from patients. But the volunteer nurses with whom I spoke all emphasized that they were not the only ones receiving payments. These payments were a sign that patients appreciated the work they were doing. They meant something. It was like saying, ‘Thanks for what you did for me’. These tokens of appreciation could take the form of cash, material gifts, or simply words of gratitude. But one could always expect something, as Frederica reasoned, ‘If you save the patient, maybe you don’t know where you will meet. “Oh, I know that nurse, she saved my life. If you have something to struggle with, he or she will help you”’.
The volunteer nurses insisted that these tokens of appreciation be distinguished from health workers’ requests for payment before performing a duty. They recounted that they themselves were asked to make payments to other health workers when they went to the hospital. For instance, one volunteer nurse was asked to pay an extra SLL50,000 for an ultrasound check during her pregnancy, which her colleagues in the focus group discussion considered to be shameless. Within a wider system of informal payments, volunteer nurses felt that they were being made to take all the blame for the various malpractices detected by the investigation. As Aminata said, this went so far that people on the street would point their finger at her and shout derisively ‘Nurse!’
During the Ebola epidemic, nurses working in the ETUs were heavily criticized by the public for having demanded an increase in their risk allowance from the government. According to Alice Street (2016), this criticism was premised on the misconception of nurses as selfless caregivers and not as employees with rights and duties. As she points out, nurses were expected to attend to every patient with empathy and they were criticized if they pursued their own self-interest. Such a conception of health workers as altruistic caregivers ignores the fact that their work receives neither an adequate degree of financial nor social recognition (Street 2016, 333). The work of volunteer nurses at the ETUs was both risky and emotionally demanding: they had to care for dying patients, wash patients to make them feel more comfortable, and deal with highly infectious human waste. When the institutions failed to appreciate this care as meaningful work, the nurses felt that they had been abused, literally, for doing the dirty work in the ETUs.
Distrust
The ambiguities surrounding the term ‘appreciation’ reflect the intermingling of formal and informal practices in the Sierra Leonean health care system. Understanding these forms of appreciation as recognition allows us to see how a lack of appreciation, or misrecognition, can have far-ranging consequences.
At one point, I asked the volunteer nurses if they would work again at an ETU in the case of another Ebola outbreak. Some rejected the idea outright and joked that they would rather run away. Others responded angrily.
Frederica: They think we have forgotten the promises they made to us. But we have not forgotten.
Aminata: They hurt us. I will never forgive them for what they did to us.
Frederica: If Sierra Leoneans are going to promise us that they will give us a pin code, I will [still] not go. There is no trust. I can’t risk my life if there is no trust. Because we have entered into an agreement, but they never fulfilled. Breach of contract. So I don’t think I will risk myself again.
Other nurses answered that they would work if they were given a pin code, but they would have to receive the pin code before they would start to work. As Tenneh explained: ‘Even if there is an outbreak now. Our children are suffering. We were scared to go and work there. Because we have seen what had happened before, what they did to us, so we do not have any confidence. There is no trust’.
I wondered if perhaps the promise of employment, made in the heat of the epidemic, was never meant to be a serious offer. This was contested, however, by the volunteer nurses. Frederica said:
They know that – it will not be easy to be forgotten, but the reason behind it is that … they ignore the situation because they know no one is there to fight for us. That is the main issue. We have no one to help us, to tell those people ‘You made a promise’ to these nurses. … We have no one. … We have nobody to fight for us. They can do anything they like at any time. Because if – we have a strong somebody, he or she will go say, ‘No, you made a promise to these people. And you have to give them what you have promised them’.
These broken relations of trust cannot be repaired without taking into account the feelings of humiliation brought about by institutionalized forms of misrecognition. The promise ‘We will give you a pin code’ is a performative act that requires trust in order to become effective. In the context of the Ebola epidemic, it was a promise made to compel volunteers to work at the ETUs. Not fulfilling the promise is not immoral per se, but it undermines the trust that was given in the first place. Moreover, dismissing the nurses by memo, without convening a meeting to discuss the matter, was seen as an act of disrespect.
Conclusion
I began this article by noting that current public health discourses emphasize the importance of health workers in stronger health systems. According to various expert panels convened to discuss the future of global health after the Ebola epidemic, robust health care systems are assumed to be better prepared for possible outbreaks and thus contribute to a more secure future (Gostin et al. 2016). By implication, this is expected to enhance people’s trust in biomedical measures, hospitals, and health workers, all frequently articulated objectives of the post-Ebola reconstruction of health care systems in West Africa (see, for example, Dhillon and Kelly 2015).
I have contrasted these policy recommendations with a discussion of the lived realities of institutionalized subordination and misrecognition. I have focused on the feelings that arise when authorities do not keep their word, when language hurts, and when institutions humiliate those who depend on them.
These institutionalized practices of humiliation are not only encountered in Sierra Leone. In fact, the report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola, published in the Lancet (Moon et al. 2015), included an appendix written by four authors in the name of fifty-eight signatories that asked critically how nurses and other frontline health workers could have been excluded from the scientific discourse about the future of global health (Glaser et al. 2016). It is worth citing an extended passage from this appendix:
Who speaks for the nurses whose lives were sometimes placed at risk during the outbreak through the hubris of politicians, administrators, and physicians that underestimated the extent of the outbreak? When the policy makers, researchers, and high level clinicians are gone, there will still be nurses serving in remote posts in central and west Africa, placing their lives at risk as a result of exposure to Ebola, HIV, tuberculosis, and other diseases for want of masks, goggles, gloves, bleach, or, simply, running water. (Glaser et al. 2016, 848)
In this analysis of institutionalized maltreatment, I paid specific attention to the nurses’ explanations of their frustration, anger, disappointment, and humiliation, and the maltreatment that destroyed their trust in public health authorities. Such maltreatment goes against the basic ethical premise that nobody deserves to be treated as an instrument only to be cast away afterwards.
One cannot begin to comprehend the injustice that volunteer nurses experienced in the aftermath of the Ebola epidemic without an understanding of the moral emotions of disrespect and humiliation. And we cannot grasp the ethical implications to be inferred from these experiences of misrecognition without a phenomenological interest in how injuries are felt, sensed, and articulated in everyday interactions.
Rights-based conceptions of justice used to justify global health interventions typically don’t take emotions into account. Yet, anthropologists are painfully aware of the degrading conditions upon which international aid, scientific cooperation, and humanitarian interventions are premised (Kleinman, Das, and Lock 1997; Rottenburg 2009). The sensibilities for these institutionalized humiliations cannot be replaced by seemingly more objective accounts citing scientific evidence and arresting pictures, which anthropologist have discussed critically (Kleinman 2006; Scheper-Hughes 2008).
In my discussion of the highly emotional experiences of volunteer nurses, I have attempted to cast some of these moral emotions to examine the institutionalized structures of misrecognition and subordination. Following Honneth (1996), we can conceive of these emotional reactions as a pre-theoretical basis for social critique, which grows out of the specific treatment one expects to deserve. From a moral theoretical perspective, these expectations may be so subjective that it seems impossible to establish a common principle of decent treatment. Still, the moral language used in everyday life usually provides an elaborated repertoire for reflecting on the various nuances of disrespect and humiliation, as I have tried to capture here. This language reflects what various anthropologists describe as the ethical domain, which transpires through practices of evaluating and judging each other with the aim of making ourselves accountable to others (Keane 2016; Lambek 2016). In this case, volunteer nurses evaluated the immanent contradictions of work and recognition in the aftermath of the Ebola epidemic in Sierra Leone, and articulated the moral emotions incited by these contradictions. Their feelings of being humiliated were legitimated by more complex moral sentiments that a promise ought to be kept, that hardworking nurses deserve respect, and that no human being should be treated as an object.
Acknowledgements
This paper is the result of the ongoing collaborative research project ‘Trust in Medicine after the EVD epidemic’ (2016–2019) funded by the priority program ‘German-African Collaborations in Infectiology’ of the German Research Foundation. The field research benefitted greatly from the invaluable help of Almudena Mari-Saez. I am grateful for comments by Uli Beisel, Susan L. Erikson, Lorenz Gosch, and Zoe Goldstein. A first draft of this paper was presented at the Future Health Measures workshop organized by Richard Rottenburg and Abou Farman (7–8 August 2016, Berlin).
About the author
Sung-Joon Park is an anthropologist working at the Martin-Luther-University Halle-Wittenberg in Germany. His research interests are in the field of anthropology of biomedicine, science and technology studies (STS), pragmatist philosophy, and phenomenology. He conducted fieldwork in South Africa and Uganda studying mass HIV treatment programs, post-traumatic stress disorder, and scientific infrastructures. Herein he explores question of hope, trust, and time. His new study, a collaborative research project, is concerned with Ebola epidemics and the formation of trust and distrust.
References
Abramowitz, Sharon Alane. 2014. ‘How the Liberian Health Sector Became a Vector for Ebola’. Fieldsights - Hot Spots, Cultural Anthropology. 7 October 2014. http://www.culanth.org/fieldsights.
Beisel, Uli. 2014. ‘On Gloves, Rubber and the Spatio-Temporal Logics of Global Health’. Somatosphere. 6 October 2014. http://somatosphere.net/2014/10/rubber-gloves-global-health.html.
Brown, Hannah, and Ruth J. Prince. 2015. ‘Introduction: Volunteer Labor Pasts and Futures of Work, Development, and Citizenship in East Africa’. African Studies Review 58, no. 2: 29–42. https://doi.org/10.1017/asr.2015.36.
Butler, Judith. 1997. Excitable Speech: A Politics of the Performative. New York: Routledge.
Calain, Philippe, and Marc Poncin. 2015. ‘Reaching out to Ebola Victims: Coercion, Persuasion or an Appeal for Self-Sacrifice?’ Social Science & Medicine 147: 126–33. https://doi.org/10.1016/j.socscimed.2015.10.063.
Dhillon, Ranu S., and J. Daniel Kelly. 2015. ‘Community Trust and the Ebola Endgame’. New England Journal of Medicine 373: 787–89. https://doi.org/10.1056/NEJMp1508413.
Fraser, Nancy. 2000. ‘Rethinking Recognition’. New Left Review 3: 107–120.
Fraser, Nancy, and Axel Honneth. 2003. Redistribution or Recognition? A Political-Philosophical Exchange. London: Verso.
Geissler, Paul Wenzel. 2012. ‘“We Are Not Paid – They Just Give Us”: Liberalisation and the Longing for Biopolitical Discipline around an African HIV Prevention Trial’. In Rethinking Biomedicine and Governance in Africa: Contributions from Anthropology, editedby Julia Zenker and Richard Rottenburg, 197–228. Bielefeld: Transcript.
Glaser, Elizabeth, Sheila Davis, Cecelia Flomo, Anne Sliney, and Mary W. Tiah. 2016. ‘The Harvard-LSHTM Panel on the Global Response to Ebola Report’. Lancet 387, no. 10021: 848. https://doi.org/10.1016/ S0140-6736(16)00391-3.
Gostin, Lawrence O., Oyewale Tomori, Suwit Wibulpolprasert, Ashish K. Jha, Julio Frenk, Suerie Moon, Joy Phumaphi, et al. 2016. ‘Toward a Common Secure Future: Four Global Commissions in the Wake of Ebola.’ PLoS Medicine 13, no. 5: e1002042. https://doi.org/10.1371/journal.pmed.1002042.
Honneth, Axel. 1996. The Struggle for Recognition: The Moral Grammar of Social Conflicts. Cambridge, MA: MIT Press.
Honneth, Axel. 2007. Disrespect: The Normative Foundations of Critical Theory. Cambridge: Polity Press.
Keane, Webb. 2016. Ethical Life: Its Natural and Social Histories. Princeton, NJ: Princeton University Press.
Kelly, Ann H., and Paul Wenzel Geissler. 2011. ‘Introduction: The Value of Transnational Medical Research’. Journal of Cultural Economy 4, no. 1: 3–10. http://doi.org/10.1080/17530350.2011.535329.
Kleinman, Arthur. 2006. What Really Matters: Living a Moral Life amidst Uncertainty and Danger. New York: Oxford University Press.
Kleinman, Arthur, Veena Das, and Margaret M. Lock. 1997. Social Suffering. Berkeley: University of California Press.
Lambek, Michael. 2015. ‘Living as If It Mattered’. In Four Lectures on Ethics, edited by Veena Das, Didier Fassin, and Webb Keane, 5–52. Chicago: HAU Books.
Margalit, Avishai. 2009. The Decent Society. Cambridge, MA: Harvard University Press.
McMahon, Shannon A., Lara S. Ho, Hannah Brown, Laura Miller, Rashid Ansumana, and Caitlin E. Kennedy. 2016. ‘Healthcare Providers on the Frontlines: A Qualitative Investigation of the Social and Emotional Impact of Delivering Health Services during Sierra Leone’s Ebola Epidemic’. Health Policy Plan 31: 1232–39. https://doi.org/10.1093/heapol/czw055.
Moon, Suerie, Devi Sridhar, Muhammad A. Pate, Ashish K. Jha, Chelsea Clinton, Sophie Delaunay, Valnora Edwin, Mosoka Fallah, David P. Fidler, and Laurie Garrett. 2015. ‘Will Ebola Change the Game? Ten Essential Reforms before the Next Pandemic. The Report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola’. Lancet 386 (10009): 2204–21. https://doi.org/10.1016/S0140-6736(15)00946-0.
Piot, Peter. 2014. ‘Ebola’s Perfect Storm’. Science 345, no. 6202: 1221. https://doi.org/10.1126/science.1260695.
Pogge, Thomas. 2002. World Poverty and Human Rights: Cosmopolitan Responsibilities and Reforms. Cambridge: Polity Press.
Pogge, Thomas. 2005. ‘Human Rights and Global Health: A Research Program’. Metaphilosophy 36, nos. 1/2: 182–209. https://doi.org/10.1111/j.1467-9973.2005.00362.x.
Prince, Ruth J., and Hannah Brown. 2016a. Volunteer Economies: The Politics and Ethics of Voluntary Labour in Africa. Rochester, NY: James Currey.
Prince, Ruth J., and Hannah Brown. 2016b. ‘Introduction’. In Volunteer Economies: The Politics and Ethics of Voluntary Labour in Africa, editedby Ruth Prince and Hannah Brown, 1–28. Rochester: James Currey.
Prince, Ruth J. 2015. ‘Seeking Incorporation? Voluntary Labor and the Ambiguities of Work, Identity, and Social Value in Contemporary Kenya’. African Studies Review 58, no. 2: 85–109. https://doi.org/10.1017/asr.2015.39.
Richards, Paul. 2016. Ebola: How a People's Science Helped End an Epidemic. London: Zed Books.
Rottenburg, Richard. 2009. Far-fetched Facts: A Parable of Development Aid. Cambridge, MA: The MIT Press.
Scheper-Hughes, Nancy. 2008. ‘A Talent for Life: Reflections on Human Vulnerability and Resilience’. Ethnos 73, no. 1: 25–56. https://doi.org/10.1080/00141840801927525.
Street, Alice. 2016. ‘Making People Care’. Lancet 387, no. 10016: 333–34. https://doi.org/10.1016/S0140-6736(16)00119-7.
Thomas, Abdul Rashid. 2016. ‘Disturbing Evidence of Deplorable Healthcare Delivery in Sierra Leone’. Sierra Leone Telegraph, 11 September. http://www.thesierraleonetelegraph.com/?p=13681.
Throop, Jason C. 2012. ‘Moral Sentiments’. In A Companion to Moral Anthropology, edited by Didier Fassin, 150–69. Chichester, England: John Wiley & Sons.
UNICEF. 2014. ‘Sierra Leone Health Facility Survey 2014. Assessing the Impact of the EVD Outbreak on Health Systems in Sierra Leone Survey Conducted 6-17 October 2014’. https://www.unicef.org/emergencies/ebola/files/SL_Health_Facility_Survey_2014Dec3.pdf.
Waterton, Claire, and Brian Wynne. 1999. ‘Can Focus Groups Access Community Views?’ In Developing Focus Group Research: Politics, Theory, and Practice, edited by Jenny Kitzinger and Rosaline S. Barbour, 127–43. London: SAGE Publications.
Wurie, Haja R., Mohamed Samai, and Sophie Witter. 2016. ‘Retention of Health Workers in Rural Sierra Leone: Findings from Life Histories’. Human Resources for Health 14, no. 3: 1–15. https://doi.org/10.1186/s12960-016-0099-6.
Endnotes
1 Back
All names in this text are pseudonyms.
2 Back
I find Honneth’s (2007) discussion of disrespect, from which his notion of recognition has been derived, and Margalit’s (2009) work on humiliation as an encroachment of one’s of self-respect more helpful than other frameworks, such as Nancy Fraser’s (2000; see also the discussion between Fraser and Honneth 2003), which focus on multicultural recognition and identity politics. For Honneth and Margalit, an understanding of disrespect and humiliation requires us to extend conventional moral theories toward an understanding of the affective dimensions of recognition that precede more abstract modes of cognition.
3 Back
For a discussion of the difficulties of moral theories of justice to grasp the distinctive ethical challenges posed by the Ebola response, see Calain and Poncin (2015).
4 Back
Interviews were conducted by Sung-Joon Park (Martin-Luther-University Halle-Wittenberg, Germany). Sylvanus Spencer (Fourah Bay College, Sierra Leone) facilitated the focus group discussions. Two doctoral students, Sophie Weißenhorn (Martin-Luther-University Halle-Wittenberg, Germany) and Michael Abu Sam (Fourah Bay College, Sierra Leone), assisted with the focus group discussions.
5 Back
I thank Paul Richards for this reference to this literature on focus group discussions.
6 Back
According to our interlocutors, a state enrolled community health nurse would normally receive a monthly salary of about SLL400,000 (US$100). A state registered nurse earned an estimated SLL650,000 (US$150).