NGOs, partnerships, and public-private discontent in Nepal’s health care sector
—
Abstract
The aspiration and ambiguity of public-private partnerships (PPPs) in Nepal’s health care sector
In 1995, the well-known Nepali physician and health care scholar Dr. Hemang Dixit (1995, 146) wrote in his book Nepal’s Quest for Health that ‘while some health services are provided by nongovernmental organizations [NGOs], healthcare delivery is by and large a government affair’. Things have changed a good deal, with Nepal’s Social Welfare Council reporting just shy of forty thousand[note 1] NGOs registered in the country in 2014 (figure 1), comprising what the late Nepali anthropologist Saubhagya Shah (2002, 156) referred to as a veritable ‘NGOdom’.[note 2]
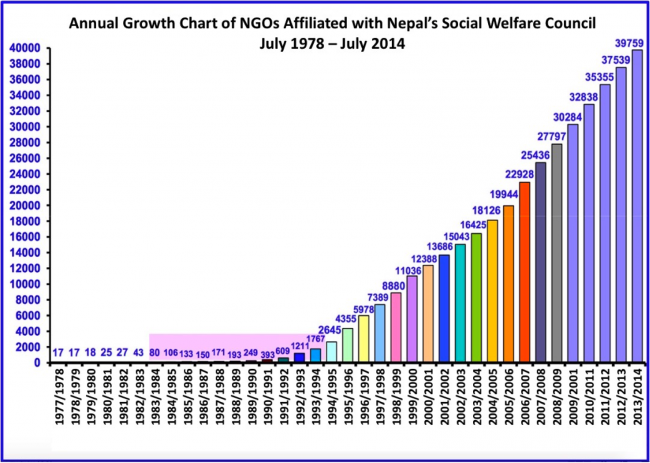 Figure 1. The monotonic rise of NGOdom in Nepal Source: Adapted from Social Welfare Council (http://www.swc.org.np/wp-content/uploads/2015/08/by-yearwise.pdf)
Figure 1. The monotonic rise of NGOdom in Nepal Source: Adapted from Social Welfare Council (http://www.swc.org.np/wp-content/uploads/2015/08/by-yearwise.pdf)This play on words signals an emergent nongovernmental government (Fassin 2007; Ferguson and Gupta 2002) that has mushroomed in Nepal following the liberalization of the economy in the 1980s (Rankin 2004), the arrival of multiparty democracy in the 1990s, and a global trend that continues to see funds for international (health) development and aid routed away from the public sector towards nonstate actors like NGOs (Escobar 1995; Kamat 2004; Karkee and Comfort 2016; Pfeiffer 2003).[note 3] This trend has been accompanied by a corollary growth in new forms of partnerships between branches of the Nepali government and any number and combination of nonstate actors, which include NGOs, community-based organizations (CBOs), bilateral development agencies, academic research centers, multinational institutions, pharmaceutical manufacturers, for-profit entities, and philanthropies. These partnerships have dramatically reconfiguredNepal’s contemporary health care and public health landscapes, made up of an increasingly ‘unruly mélange’ (Buse and Walt 1997) of public and private players, as well as what in the past two decades or so have become known as ‘public-private partnerships’, or PPPs.
PPPs represent one kind of global health assemblage (Ong and Collier 2005): emergent, transnational forms of collaboration and intervention between public and private entities that cohere around stated goals of improving health, treating disease, and fortifying health care delivery systems (Brown et al. 2012; Buse and Harmer 2007; Cueto 2013; Geissler 2013; Rajak 2011). From multinational initiatives to single-country collaborations, these assemblages sometimes assume new forms (Ong and Collier 2005, 11), but are really characterized more by their shifting centers of power, technical and financial infrastructures and administrative systems, and the ‘uneasy, unstable interrelationships’ upon which they rest (ibid., 12). Ultimately, the heuristic of ‘assemblage’ is useful here to get at the inherent inequalities (Crane 2010) and tensions in, and constituent of, (public-private) partnerships in global health. Assemblage similarly points to the ‘para-statal spaces’ (Geissler 2015, 1) that are created by these new arrangements, capturing that ‘peculiar sense of things changing without losing their form’. Put another way, these partnerships are ‘more of the same thing, and yet something very different’ (Geissler 2015, 1).
A growing body of social science literature examines the proliferation of PPPs in global health and how they have altered the landscape in both promising and problematic ways. For example, scholars have studied how PPPs have injected large amounts of money into national budgets, generally for disease-specific and vertical health programming (Peters and Phillips 2004; Pfeiffer 2013; Ramiah and Reich 2005; Ravishankar et al. 2009); created new modes of health governance, including taking on core responsibilities of the public sector (Brown 2015; Gerrets 2015; Kapilashrami and O’Brien 2012; Ruckert and Labonté 2014); and generated new standards and forms of evaluation and accountability (Adams 2016; Cueto 2013; Packard 2016; Taylor and Harper 2015; WHO 2008) that are typically unconcerned with community definitions of, or concerns over, notions of ‘scale’,[note 4] ‘success’, or ‘impact’.
Scholars have also critically examined how larger-scale PPPs such as the US President’s Emergency Plan for Aids Preparedness (PEPFAR), the Global Alliance for Vaccines and Immunizations (GAVI), and the Global Fund to Fight AIDS, Tuberculosis, and Malaria (GFATM) have created new partnership modalities that perpetuate inequalities or competition (Kapilashrami and O’Brien 2012; Storeng and Béhague 2014a; Taylor and Harper 2014), or contribute to subverting or co-opting efforts aimed at strengthening health systems more broadly (Kenworthy 2016; Pfeiffer 2013; Ruckert and Labonté 2014; Storeng 2014). As the World Health Organization (WHO 2008, 3–4) concedes, ‘In their worst manifestations, [PPPs] … distorted national health and development priorities and diverted health workers away from other important health challenges’. Here, we follow a similar line of thinking to ask: what if, even on a smaller scale, NGO-based PPPs continue to do the same thing?
In Nepal, PPPs have similarly emerged as prominent models of collaboration to fund, deliver, and scale health care services and infrastructure; increase ‘good governance’; catalyze innovation and research; and improve access, equity, and quality of health care services. Nepal’s ‘State Non-State Partnerships Policy for the Health Sector’ was written in 2012 to pave the way for introducing PPPs to ‘improve the health status of the people, especially women, children, the poor and the marginalised sections of the population’ (MoHP 2012, 4). However, this draft policy document has yet to be formally approved, owing in large part to the political instability in the country, which has seen a revolving door of administrations come and go, roughly twenty-seven incarnations of government in twenty-six years.
The draft PPP policy essentially leaves it up to individual entities to determine contractually ‘the scope of services, beneficiary groups, mutual obligations and responsibilities, the risks for each partner, the time-span, performance and outcome indicators, supervision and monitoring, quality, and efficiency of service delivery’ (MoHP 2012, 4). In the Nepali context, then, the idea of PPPs necessarily involves embracing both the promise and the ambiguity of these arrangements, as it takes three already-vague concepts (‘public’, ‘private’, and ‘partnership’) and hyphenates them into a potentially even more nebulous arrangement.[note 5] The often-fuzzy operational boundaries between these partnerships (Mitchell 2014; Richter 2004; Roehrich et al. 2014) – as well as their potential breadth in scope and composition – make them appealing and fundable arrangements in the global public health marketplace, particularly in Nepal. As one senior leader from the United States Agency for International Development (USAID) noted during a meeting in Kathmandu about a funding call for applications: ‘Creative consortiums sell’.[note 6]
Drawing on our collective experiences of working in a public–private partnership between the NGO Possibleand the Ministry of Health in Nepal, we discuss the contested space of this collaboration at a particular moment during Nepal’s ‘struggle for a public sector’ (Pfeiffer 2013). At this moment, a new national rhetoric concerning the constitutionally guaranteed right to free primary health care confronts the day-to-day experience of Nepali people ‘navigating the diagnostic maze’ (Harper 2014) of public, private, and now public-private providers. Here, we take up the call by other anthropologists to ethnographically examine the local, cultural politics of smaller forms of public-privatization (Brada 2011; Kenworthy 2016; Storeng and Béhague 2016). This approach is important because smaller NGOs play increasingly bigger roles in partnering with governments and generating the success stories of global health agendas, including demonstrating their ‘impact’through quantitative metrics and performance indicators (see for example Adams et al. 2015; Biehl and Petryna 2013; Storeng and Béhague 2014b), which may or may not be accountable to the communities where they work.
To further locate the emergence of PPPs in the Nepali context, we situate this look at one such partnership within the context of a booming fee-for-service health care industry in the country (Maru and Uprety 2015) – including throngs of NGOs – an epidemic of private, for-profit medical colleges, and the roll-out of a national insurance scheme. We describe the PossiblePPP as just one approach to partnership that seeks to combat this broader trend towards the commodification of health and health care in the country through seeking to strengthen the public sector. However, our model still seems to tap into some of the anxieties inherent in new forms of public-privatization of global health work (Kenworthy 2016) in Nepal. We then offer an ethnographic discussion of events that unfolded last year at a hospital managed through the PPP when a child passed away after being admitted. This tragic incident offers an important departure point for opening up important discussions about some of the tensions at the center of public-private partnerships, which are mirrored and amplified by growing Nepali public discontent and a loss of faith in an increasingly privatized health care landscape.
This story is simultaneously set against the backdrop of a broader global trend towards the privatization of health care services and global health science research (Broad 2014; Plumer 2005), as corporations, philanthropies, and entrepreneurial organizations – even NGOs – based on Silicon Valley start-up culture emerge as increasingly important actors in the field of global health (Kenworthy, MacKenzie, and Lee 2016; Rajak 2011). Indeed, from performance-based financing schemes (Eichler et al. 2013; Kapilashrami and O’Brien 2012; Renmans et al. 2016), shell NGOs (Crane this issue), crowdfunding (Kenworthy this issue) and speculative pandemic financing (Erikson 2015a, 2015b), to the entrée of philanthrocapitalism behemoths like the Bill & Melinda Gates Foundation ‘creating cures for market failures’ (Sparke 2011; see also Birn 2014), the global public health and health care landscape is increasingly business-like. We will suggest that the effects, and affects, of this arc are felt in places like Nepal, where there emerges a sense that, despite rhetoric to the contrary, health (care) is a commodity to buy and sell.
The privatization of Nepal’s health care sector
Nepal’s 1991 National Health Policy was part of the country’s move towards economic liberalization, and it opened the door further for the growth of private investment in the health care sector (Mishra and Acharya 2013). As a result, the private sector has grown significantly in recent years to include informal (in other words, unlicensed) practitioners; pharmacists; fee-for-service hospitals, clinics, and nursing homes; and for-profit medical colleges/teaching hospitals. This trend towards privatization has paralleled the increased availability of pharmaceuticals in Nepal (Harper 2014; Subedi 2001), a growing medical voluntourism industry (Citrin 2010), and a nongovernmental government (Fassin 2007; Ferguson and Gupta 2002) that poses a growing challenge to national efforts to fund, coordinate, deliver, and regulate national health care systems (cf. Pfeiffer 2003). Regulation is especially challenging in rural areas (Harper 2014, 29), and in recent years there has been a spate of coverage in Nepali media outlets highlighting government attempts to crack down on ‘fake doctors’ in what was officially termed ‘Operation Quack’ (Lamichhane 2016b). In one widely publicized instance, among many, a doctor had been working without any medical license for years in a NGO-run hospital in one of Nepal’s most remote districts (Rai 2013).[note 7]
By way of numbers, in 1990 there were only sixteen private hospitals in Nepal, a figure that soared to 301 in 2014 (MoHP 2015). Two-thirds of all hospital beds in the country are private, and 60 percent of Nepali doctors are employed in the private sector (MoHP 2010, 2013); this estimate also likely excludes public-sector physicians who moonlight in private clinics or pharmacies (where drugs are typically more expensive, see for example Mishra et al. 2015b). Government health expenditure per capita is US$16, with the private sector accounting for 70 percent of total health expenditure in Nepal, and 81 percent of that comes from out-of-pocket payments (Mishra et al. 2015a; Saito et al. 2014).[note 8] One study conducted in 1997 in western Nepal suggested that medical expenses were one of the most common causes of debt (Robertson and Mishra 1997, cited in Harper 2014, 29), and a more recent one conducted in Kathmandu found that more than one in seven households self-reported catastrophic expenditures on health in the previous thirty days (Saito et al. 2014).[note 9]
This scenario is a far cry from the promise made in Nepal’s new constitution, promulgated in 2015, which now guarantees that ‘Every citizen shall have the right to free basic health services from the State, and no one shall be deprived of emergency health services’ (emphasis added). It goes on to note that, ‘Every citizen shall have equal access to health services’. Delivering on this promise is a herculean undertaking that will likely see the private sector tapped more and more. An additional problem here is that this right does not extend to the estimated four million people living in Nepal without citizenship documents (Latschan 2015), who would similarly not be eligible for the new national health insurance program, which is currently being implemented in a handful of districts alongside the development of plans for large-scale implementation. The insurance program is actually aimed at extending universal coverage for health care services, in line with the United Nation’s Sustainable Development Goals, and at reducing rising out-of-pocket expenditures, yet we suggest it is also simultaneously bound up in the broader trend towards commodification of health and health care in Nepal.
Nepal’s national insurance program was spearheaded by a public-private partnership between the Korean International Cooperation Agency, the German Society for International Cooperation, and the Nepal Health Sector Programme. The then-named Social Health Security Development Committee (SHSDC),[note 10] the unit that oversaw the pilot insurance program in Nepal, was employing insurance enrollment officers that walk house to house to register individuals for the program, who each pay 2,500 Nepalese rupees (NPR), equal to US$25, with up to NPR50,000 ($US500) promised in coverage at empaneled public-sector health care facilities. According to early reports, the program was running at a deficit as it struggled to raise the premiums required to sustain itself (Aryal 2016).[note 11] To be sure, there are many reasons for this, one of which is the presence of a substantial private health care sector, which, though certainly more expensive, tends to be less bureaucratic. We suspect the bigger barrier to enrollment has been people’s experiences of unfilled promises made by the government or other ‘well-trained strangers’ who show up at their door, such as NGO workers, enumerators conducting surveys, and politicians (cf. Sanders and McKay 2013, 112). Perhaps the promise of NPR50,000 tomorrow for the price of NPR2,500 today still seems a bit too good to be true.
 Figure 2. A national health insurance program in Nepal: Your Health is Our Concern Source: A computer screen capture of an insurance program promotional video entitled ‘Gajjabko Card,’ or ‘The Amazing Card’.
Figure 2. A national health insurance program in Nepal: Your Health is Our Concern Source: A computer screen capture of an insurance program promotional video entitled ‘Gajjabko Card,’ or ‘The Amazing Card’.Nepal’s medical education sector has been centripetally pulled into this larger drive towards privatization, with grave consequences for regulating quality – as well for how the broader public views the quality – of its health care providers. About two thousand students annually enroll in seventeen private medical colleges offering Bachelor of Medicine, Bachelor of Surgery (MBBS) programs (compared to only three public medical colleges), with nearly all located in urban centers and typically catering to those who can afford to pay. Except for the mandatory full scholarships that private medical colleges must provide for students selected by the government, seats in private medical schools tend to be reserved for students who can pay the costs of admission, with tuition ranging from NPR3–5 million, or $US30,000–50,000. It is also widely known that behind-the-scene ‘donations’ may also help to relax selection criteria or waive qualifying exams. A widely read article in the Nepali Times highlighted undercover reporting done by the Centre for Investigative Journalism, which secretly recorded one administrator bragging about connections in the Supreme Court, and their ability to effectively bribe the Nepal Medical Council and the Secretary of Health to ensure student admission (Sapkota 2015). The medical education sector has become an increasingly suspect doctor factory, churning out wealthy and well-connected doctors.
 Figure 2. Dr. Govinda K. C. on a fast-unto-death in protest of Nepal’s medical education system Source: https://thewire.in/56418/nepal-doctor-govinda-kc/
Figure 2. Dr. Govinda K. C. on a fast-unto-death in protest of Nepal’s medical education system Source: https://thewire.in/56418/nepal-doctor-govinda-kc/The renowned Nepali orthopedic surgeon and activist Dr. Govinda K. C. has gone on thirteen hunger strikes since 2012, calling for major reforms to the medical (education) sector (Kathmandu Post 2017). Prime among his demands are that the government stop accrediting for-profit and private medical colleges with substandard facilities and curricula, that medical schools and opportunities for education are equally spread out among the country, and that politically and personally motivated appointments at these institutions are halted (Mallapaty 2014; Magar and Subba 2012). Throngs of (primarily young) doctors have taken to striking and closing medical facilities in support of these reforms over the years. Dr. K. C. and his supporters have achieved some significant victories, though the structural features of medical education remain pretty much intact, run by what they have called Nepal’s ‘medical mafia’ (Lamichhane 2016a; Sapkota 2015). As these issues continue to be brought to the fore of public discussions, one seemingly unavoidable consequence is the public’s continued erosion of faith in health care institutions and providers (cf. Marsh 2015), a topic to which we return below.
A PPP for strengthening public sector health care systems
Public-private partnerships, then, emerge as particularly salient amidst this trend, alongside concerns over the increasing privatization/commodification of health care that jar with the contemporary rhetoric around primary health care services free of cost from the state. The authors work for one PPP formed between the US-based nonprofit organization Possibleand Nepal’s Ministry of Health, which delivers care through an ‘accountable care systems’ framework (McClellan et al. 2014) in which the Nepali government plays the role of cofinancer, owner of facilities, and regulator of services and population health outcomes. The Possible PPPoperates tertiary-level hospitals staffed by both government health care workers and Possible-paid team members in two districts in Nepal, each with full-spectrum inpatient, outpatient, laboratory, radiology, and surgical care. Hospitals are also linked to a network of full-time, salaried community health care workers (CHWs) (cf. Maes et al. 2010) who deliver home-based care and collect data on health care services and outcomes via an integrated electronic health record (EHR) system (Bangura et al. 2015).
Possible’s ‘origin story’ (see Kenworthy this issue) involves the story of four medical students (three born in the United States, one born in Nepal) who set out in 2008 to start a health care NGO committed to social justice and health care equity (Bernardo 2008). In fact, Possible was originally called ‘Nyaya Health’, with ‘nyaya’ translating most simply as ‘justice’ in Nepali. Though there is much more to it, in part, the name of the organization was changed because it was considered hard to pronounce by non-Nepali speakers, and therefore hard to memorize, tell friends and colleagues about, and, ultimately, fund. The name ‘Possible’, however, is ‘byte sized’ and easy,[note 12] and somehow exemplary of the growing intermingling and influence of the social impact and entrepreneurial spheres of Silicon Valley that Kenworthy discusses in her essay in this issue (see also Lee 2014). Within our organization, there are some obvious examples of this, such as referring to the name changeas a ‘rebrand’, drawing inspiration from Netflix and Google to drive organizational culture, using an online project management tool (notably, started by one of the cofounders of Facebook[note 13]) as the primary form of communication throughout the organization, the fact that Possiblehas a CEO and not an executive director, as might be typical of a ‘global health organization’, and a board of directors constituted almost exclusively by US folks from the investment, pharmaceutical, IT, and social entrepreneurial sectors.
Yet, while Possiblefeels right at home in the private sector, the PPP has developed contractual principles and a revenue model that cohere around strengthening the public sector and enshrining the constitutional right to free health care. To achieve this, the PPP focuses on several core principles:
1. Existing infrastructure. Possible works only within existing government facilities, and links them with full-time CHW networks for longitudinal care, referral, and follow-up. To our knowledge, this is the first instance that a NGO has assumed, through a PPP mechanism, responsibility over the delivery of all health care services at a government hospital (Kalaunee et al. 2017);
2. National capacity. Building Nepali health care worker capacity is a core aim of the partnership, and Possible approaches this task with humility and understanding that ‘capacity building’ is not a one-way street (Wendland 2016a) nor a static process. The PPP does not employ (or allow) expatriate clinicians to provide direct medical care in Nepal;
3. Compensation. Possible pays salaries commensurate with government scales as signatories to the NGO Code of Conduct (Pfeiffer et al. 2008) that seeks, among other goals, to create compensation best practices to strengthen public-sector delivery systems;
4. Public financing. Possible works with the government of Nepal as the regulator of health care services through performance-based grant agreements (PBGAs), the goal of which is a population-based, capitated financing mechanism in which the government pays Possible a certain number of rupees per person in a designated catchment area if we achieve certain health outcomes that are set collaboratively with the Ministry of Health.[note 14] Performance-based financing mechanisms raise many important questions, including how ‘performance’ is defined and who gets to define it;
5. Access. The PPP provides all services completely free to patients at the point of care.
This last one is central to the PPP model, even as Possible hears quite regularly – from potential funders, other NGOs, and government officials alike – that providing free care is not sustainable. This often amounts to little more than the ‘skin in the game’ argument, suggesting, as we’ve heard time and time again, that Nepali people won’t value health care unless they pay for it. The fee-for-service model of health care championed, if not pioneered, in the United States is one of the country’s most dangerous exports. Medical bills remain the number one reason people file for bankruptcy in the United States, and 72 percent of those who file have health insurance (Himmelstein et al. 2005). In addition to a mound of evidence that suggests that user fees, no matter how small, tend to prevent the poor from accessing care (see for example Farmer et al. 2013, 89–90; Pearson 2004; Robert and Ridde 2013; Watson et al. 2016), this market logic is exactly the kind of thinking that contributed to the ‘under-resourcing’ of public-sector health care systems in low- and middle-income countries in the first place. It is easy to forget that the protracted work of strengthening healthcare systems at the center of many PPPs involves coming to terms with, and is often directly linked to, the legacy of neocolonial aid policies like structural adjustment programs. As Pfeiffer and Chapman (2010, 155) remind us, ‘the language of public-private partnerships entered the development discussion in part to justify passing on the costs of health care to communities’. Indeed, this is how communities in Nepal often feel.
A public-private death
These issues were highlighted for us last year in September when a young child suffering from diarrhea and dehydration was admitted to a rural hospital operated by Possible and tragically died later that day. The child belonged to a prominent family from the municipality, and by nightfall, the hospital was surrounded by angry protestors, several holding cans of petrol in one hand and lighters in the other. As tensions and shouting grew, one hospital health care worker was physically assaulted by the crowd, and at the height of the protest local police told several PPP team members that they should try to sneak out, as the police would be unable to protect them if the crowd got out of hand. Protestors broke into the doctors’ living quarters and staged tableaus of empty beer bottles alongside stethoscopes, which were then captured in images and videos with their smartphones and circulated on social media, inciting more anger in the community, and a fresh set of protests outside. The hospital was forced to shut and to discharge patients admitted to the inpatient ward, despite their conditions and the near certainty that any care they received from then on out would need to be covered out of their own pocket. When the public sector – or in this case, the public-private sector is closed – the private remains open for business.
The following day, protestors forcibly extracted a public apology and admission of guilt from the PPPteam on the front steps of the hospital, in an exchange that was overseen by the district police. This public opprobrium was also videotaped and circulated on Facebook and YouTube, and received more than one million views. One of our Nepali team members received harassing phone calls for weeks after the incident, with some threatening to parade him through the municipality after putting juttako malla (a necklace of shoes) around his neckor performing kalo moso on him, smearing his face with shoe polish or soot.
In part, these events also occurred because the Possible-run hospital initiated free care in a municipality with several established private hospitals. As the PPP team slowly learned, since reopening the facility in the district following the devastating 2015 earthquakes, we had angered investors and trade unions rumored to have stoked the flames of protest. Indeed, in conversation with several PPP members, the family of the child had indicated that they did not want to make a big deal of the matter (‘Thulo kura nabanaanuhola bhanera’),[note 15] and hoped to keep it more of a private matter. The agitating parties stood to make a good deal of money from poor people seeking care in the district. That the PPP-run hospitalwasn’t also making money – even in the case of a child death like this one – seemed unthinkable. During efforts to persuade still-angry community members that the PPP did not make any money from patients, and that the hospital was actually a NGO-managed government hospital with a service delivery mandate based on the constitutionally protected right to free care, one of the authors (HB) was told repeatedly that ‘NGOs don’t do such things’, meaning provide free care. She was pressed. ‘Ok, madam, don’t talk like that. Where have you hidden the money?’ (‘La, Madam tyasto nabhannus. Paisa kaha lukhaaunubhaechha?) Here, again, free health care raises the specter of a deal too good to be true, one that should be viewed with skepticism, given the many disappointments and promises unfulfilled by the NGOdom of global health in Nepal.
Several things collapse here. For the family, there is a wrenching bare life moment at work, as they struggle to come to terms with an unthinkable and unnecessary loss. There remains no clearer indicator of the breakdown of public health care systems than the death of a child. There is also a breakdown here of the partnership between Possible and the government of Nepal, where the boundaries between NGO and public sector are muddied, and the ambiguity, friction, and complexity of doing partnership re-emerge. The social contract, too, between Possibleand the communities it serves falls apart, as systems of care come to a grinding halt. We view the reaction of the community as both an expression of the unacceptability of this loss and a reassertion of that social contract – to first do no harm, to provide free, quality health care, to not ‘let’ children die. The story – however sensationalized by media, videos, and angry protestors – is archived in the broader Nepali public imagination, driving the narrative of suspect doctors and of profits somehow gained and hidden, furthering the loss of public trust in the health care system.
Concluding thoughts: Missing the bigger picture in public-private partnerships?
As the mission of global health is increasingly defined by ‘an emphasis on the mutuality of real partnership’ (Koplan et al. 2009, 1994–95), new forms of public-privatization from large-scale multinational initiatives to smaller models based on NGO-government collaborations require continued attention. Here, we end with a few key points for further consideration.
Firstly, PPPs in Nepal such as Possible drive the kind of ‘audit culture’ (Strathern 2000) that Gimbel and colleagues discuss (this issue), yet globally there still lacks comprehensive, mutually agreed-upon metrics for evaluating the fit, acceptability, and effectiveness of these forms of partnerships (Miley 2014). As noted, one component of Possible’scontractwith the Ministry of Health is a performance-based grant agreement, a financing model that raises important questions about dominant forms of metrical reasoning in global health and what ultimately gets counted as evidence (Adams et al. 2015; Adams 2016; Rottenberg et al. 2015). Performance-based frameworks are typically built around output-based indicators (such as counting the number of patients on antiretroviral therapy, or the number of such drugs dispensed), as opposed to summary or quality measures that might describe the workings of a system of longitudinal care or set of interventions (such as the percentage of people living with HIV enrolled in a community health follow-up program whose CD4 count has increased from baseline). Critical medical anthropologists have made important interventions here, unsettling the taken-for-granted assumptions about what it means ‘to do global health through metrics’ (Adams 2016; Erikson 2012; Rottenberg et al. 2015; Wendland 2016b).
In general, we need to imagine new ways to measure so-called performance by putting our ears to the ground to come up with more people-centric outcome measures, like care-to-wait time ratios, ‘patient satisfaction’ scores, facility-level complication and readmission rates, and even overall mortality, as just a few examples. We should think of ways to adapt patient navigator programs to unique settings of care, as the PossiblePPP has been working on over the past few years (Raut and Thapa et al. 2015). The core functions of navigators are to ensure patients are listened to, don’t get lost, have their questions answered, and are spoken to in a polite manner, the opposite of typical interactions at health care facilities in Nepal. These might be important ‘pressure valve’ systems to release some of the tension and discontent felt by Nepali people navigating unfamiliar medical landscapes, as we have found at Possible.
Opportunities for communities to themselves audit health care systems, which are completely absent in Nepal, are also greatly needed, as Adams (2013, 81) notes: ‘Questions about who evaluates the evaluators, and who audits the auditors, are seldom asked’. While litigation against health care providers is common in the United States, individuals and families in Nepal simply have no legal recourse in the case of suspected medical negligence.[note 16] Patient and community anger, and violent behaviors directed towards health care practitioners – a phenomenon seemingly on the rise in Nepal (IRIN 2014; Mahat et al. 2017; Rajbhandari et al. 2015; Sudhamshu 2011) – must be seen in this context: that of an exploding, largely unregulated private sector; the factory-like production of doctors in a growing number of for-profit teaching hospitals; reports of fake doctors and government programs to ‘crack down on quacks’; and insurance programs that need to extract money from the poor to survive. Taking a cue from accountable care organizations, one ‘net promoter’ question worth asking people who visit health care facilities is: would you recommend receiving care at our facility to a friend or loved one, and why or why not? If we can find ways to deliver these questions in a manner that enables the respondent to answer honestly – a task much harder than it sounds – we will likely learn a great deal. This information would surely help craft more ‘people-centered’ partnerships.
Another crucial take away, then, is that ‘partnership’ must be viewed not as a panacea but rather as a generative and dynamic concept (Nagar and Swarr 2010). In the context of PPPs, the idea is even more fraught, encumbered as it is by the tension of the hyphen that flattens – rather than reveals – the increasing friction and ambiguity between the public and private sectors. True partnership, however, is necessarily elusive, something realized as part of a continuously contested and negotiated process rather than an achieved state (Gerrets 2015, 184). Nepal’s State Non-State Partnership Policy for the Health Sector cites ‘equity’ as the first attribute of a desirable PPP in Nepal; in parenthesis it says, ‘e.g., not a master-servant type of relationship’ (MoHP 2012, 3). This is telling. It is a far cry from the cuddlier language of partnerships or consortiums. While the potential benefits of strengthening health systems through public-private partnerships are numerous, the costs of getting these partnerships wrong are far-reaching, including the potential to recast historically extractive North-South relationships (Fowler 1991, 2000), introduce new forms of inequalities, and, perhaps even unwittingly, further undermine faith in institutions of care.
As the landscape of global health is increasingly privatized, a major risk of PPPs like Possibleis that they continue to perpetuate the conflation of health care and health, as if the former necessarily leads to the latter. The United States has proven that this is not true, as it spends half of the total global expenditure on health care, at roughly US$9,000 per capita, with continuously declining life expectancies and some of the worst health outcomes of all rich nations (Kochanek et al. 2017; National Research Council and Institute of Medicine 2013); and even that care is delivered in a terribly unequal manner (Dickman et al. 2017). At the center of most PPP models is, typically, this very assumption about the benefits of health care, when more and more evidence points to various forms of inequality as one of the primary drivers of population health outcomes (Krieger 2004; Wilkinson 1996, 2005; Wilkinson and Pickett 2009). Some have made bold claims to this effect, such as Roos and colleagues (2006, 125), who assert that ‘investments in health care should never be confused with, or sold as, policies whose primary intent is to improve population health or to reduce inequalities in health. Claims to that effect are misleading at best, dangerous and highly wasteful at worst’ (see also Kruk et al. 2010; Macinko et al. 2009; Schoeni et al. 2008). Storeng and Béhague (2014a, 998) remind us to apply that claim to PPPs, noting that ‘the attribution of “lives saved” to specific PPPs is not only prone to overestimation, but might also negatively affect the overall governance of health systems’. We are charged, then, with seriously contending with the assertion that global health partnerships may undermine public sector systems while missing the bigger picture.
And so, we return to the tragic death of the child, which remains ever instructive. In the end, it is the only thing that really counts. The causes of a child’s death from diarrhea are related to infrastructure, sanitation, education, and nutrition, all ‘upstream’ factors that are typically not the focus of PPPs in the global health arena (McCoy et al. 2013). Might our continued focus on innovative delivery mechanisms, technical fixes, and scaling interventions further medicalize poverty, perpetuating a global climate in which health care is continuously championed at the cost of trying to make it less necessary? In our efforts to build new partnerships to enshrine the necessary right to affordable and accessible health care, we need to pay attention to these blind spots, ensuring we don’t risk further drawing resources and focus away from the social determinants of health, ignoring the very reasons people become sick in the first place.
Acknowledgements
This article is based on a talk given by one of the authors, David Citrin, at the Nepal and Himalayan Studies Conference at Cornell University, 28–29 April 2017. Thanks to all members of the partnerships in global health workshop at the University of Washington, and in particular to Mark Arnoldy, Stephen Bezruchka, Rachel Chapman, Sienna Craig, Johanna Crane, Sarah Gimbel, Scott Halliday, Duncan Maru, Nora Kenworthy, James Pfeiffer, Dan Schwarz, and Lynn Thomas for their insightful comments on earlier drafts. We are particularly grateful to Tom Widger and Rene Gerrets for their peer review and analytic nudges, from which this piece benefits a great deal.
About the author
David Citrin, PhD, MPH, is Affiliate Instructor in the departments of Anthropology and Global Health at the University of Washington, where he also codirects the South Asia Center’s Nepal Studies Initiative in the Jackson School of International Studies. He has been working and conducting research in Nepal since 2001, and currently is Director of Impact at Possible. dcitrin@uw.edu
Hima Bista, MBA, MPhil,is Director of People Operations at Possible. She has sixteen years of experience delivering integrated human resources, institutional development, and management services to those working for poor and vulnerable populations. Prior to joining Possible, Hima was Head of Human Resources at DFID Nepal (UKAID) and Senior Manager HR and OD at ActionAid International Nepal (AAIN), and she has worked closely with the Netherlands Development Organisation (SNV Nepal). Hima holds an MBA in Human Resource Management from Kathmandu University, School of Management (KUSOM), and an MPhil degree in English. hima@possiblehealth.org
Agya Mahat, BDS, MPH, is an independent global health consultant. She has worked in five countries with governmental, nongovernmental, and international agencies. She has been working in the health sector since 2006 and is a board member of Possible. mahat.agya@gmail.com
References
Adams, Vincanne. 2013. ‘Evidence-Based Global Public Health: Subjects, Profits, Erasures’. In When People Come First: Critical Studies in Global Health, edited by João Biehl and Adriana Petryna, 54-90. Princeton, NJ: Princeton University.
Adams, Vincanne. 2016. Metrics: What Counts in Global Health. Durham, NC: Duke University Press.
Adams, Vincanne, Sienna Craig, and Arlene Samen. 2015. ‘Alternative Accounting in Maternal and Infant Global Health’. Global Public Health 11 (3): 276–94. https://doi.org/10.1080/17441692.2015.1021364.
Akazili, James, John Ele-Ojo Ataguba, Edmund Wedam Kanmiki, John Gyapong, Osman Sankoh, Abraham Oduro, and Dr McIntyre. ‘Assessing the Impoverishment Effects of Out-of-Pocket Healthcare Payments Prior to the Uptake of the National Health Insurance Scheme in Ghana’. BMC International Health and Human Rights 17 (13): 1–8. https://doi.org/10.1186/s12914-017-0121-7.
Aryal, Bishnu Prasa. 2016. ‘Govt’s Health Insurance Plan for All Makes Feeble Start’. myRepública,27 October. http://www.myrepublica.com/news/8096/.
Awale, Sonia. 2017. ‘A National Health Insurance Scheme Is Not as Easy as It Looks’. Nepali Times, 10–16 November. http://archive.nepalitimes.com/article/nation/national-health-insurance-not-as-easy,4028.
Bangura, Alex Harsha, Al Ozonoff, David Citrin, Poshan Thapa, Isha Nirola, Sheela Maru, Ryan Schwarz, et al. 2015. ‘Practical Issues in the Measurement of Child Survival in Health Systems Trials: Experience Developing a Digital Community-based Mortality Surveillance Program in Rural Nepal’. BMJ Global Health 1 (4): e000050. https://doi.org/10.1136/bmjgh-2016-000050.
Bernardo, Mary Lou. 2008. ‘Nyaya Health: Improving Healthcare in Western Nepal’. Angels in Medicine, 26 May. http://www.medangel.org/nyaya/nyaya014.shtml.
Biehl, João, and Adriana Petryna. 2013. When People Come First: Critical Studies in Global Health. Princeton, NJ: Princeton University Press.
Birn, Anne-Emanuelle. 2014. ‘Philanthrocapitalism, Past and Present: The Rockefeller Foundation, the Gates Foundation, and the Setting(s) of the International/Global Health Agenda’. Hypothesis 12 (1): e8. https://doi:10.5779/hypothesis. v12i1.229.
Brada, Betsy. 2011. ‘“Not Here”: Making the Spaces and Subjects of “Global Health” in Botswana’. Culture, Medicine and Psychiatry 35 (2): 285–312. https://doi.org//10.1007/s11013-011-9209-z.
Broad, William J. 2014. ‘Billionaires with Big Ideas are Privatizing American Science’. New York Times, 15 March. https://www.nytimes.com/2014/03/16/science/billionaires-with-big-ideas-are-privatizing-american-science.html.
Brown, Hannah. 2015. ‘Global Health Partnerships, Governance, and Sovereign Responsibility in Western Kenya.’ American Ethnologist 42: 340–55. https://doi.org/10.1111/amet.12134.
Brown, Tim, Susan Craddock, and Alan Ingram. 2012. ‘Critical Interventions in Global Health: Governmentality, Risk, and Assemblage’. Annals of the Association of American Geographers 102 (5): 1182–89. https://doi.org/10.1080/00045608.2012.659960.
Buse, Kent, and Andrew M. Harmer. 2007. ‘Seven Habits of Highly Effective Global Public–Private Health Partnerships: Practice and Potential’. Social Science and Medicine 64 (2): 259–71. https://doi.org/10.1016.j.sociscimed.2006.09.001.
Buse, Kent and Gill Walt. 1997. ‘An Unruly Mélange? Coordinating External Resources to the Health Sector: A Review’. Social Science and Medicine 45 (3): 449–63. https://doi.org/10.1016/S0277-9536(96)00365-6.
Citrin, David. 2010. ‘The Anatomy of Ephemeral Healthcare: “Health Camps” and Medical Voluntourism in Remote Nepal’. Studies in Nepali History and Society 15 (1): 27–72.
Crane, Johanna T. 2010. ‘Unequal ‘Partners’: AIDS, Academia, and the Rise of Global Health’. Behemoth 3 (3): 78–97.
Cueto, Marcos. 2013. ‘A Return to the Magic Bullet? Malaria and Global Health in the Twenty-First Century’. In When People Come First: Critical Studies in Global Health, edited by Joãl Biehl and Adriana Petryana, 30–53. Princeton, NJ: Princeton University Press.
Dickman, Samuel, David U. Himmelstein, and Steffie Woolhandler. 2017. ‘Inequality and the Health-Care System in the USA’. Lancet 389 (10077): 1431–41. https://doi.org/10.1016/S0140-6736(17)30398-7.
Dixit, Hemang. 1995. Nepal’s Quest for Health: The Health Services of Nepal. Kathmandu: Educational Publishing House.
Edwards, Michael, and David Hulme. 1996a. Beyond the Magic Bullet: NGO Performance and Accountability in the Post-Cold War World. West Hartford, CT: Kumarian Press.
Edwards, Michael, and David Hulme. 1996b. ‘Too Close for Comfort? The Impact of Official Aid on Nongovernmental Organizations’. World Development 24 (6): 961–73. https://doi.org/10.1016/0305-750X(96)00019-8.
Eichler Rena, Koki Agarwal, Ian Askew, Emma Iriarte, Lindsay Morgan, Julia Watson. 2013. ‘Performance-Based Incentives to Improve Health Status of Mothers and Newborns: What Does the Evidence Show?’ Journal of Health, Population, and Nutrition 31 (4, Suppl. 2): S36–47. https://doi.org/10.1016/S0140-6736(17)30398-7.
Erikson, Susan L. 2012. ‘Global Health Business: The Production and Performativity of Statistics in Sierra Leone and Germany’. Medical Anthropology 3 (4): 367–84. https://doi.org/10.1080/01459740.2011.621908.
Erikson, Susan L. 2015a. ‘The Financialization of Ebola’. Somatosphere, 11 November. http://somatosphere.net/2015/11/the-financialization-of-ebola.html.
Erikson, Susan L. 2015b. ‘Secrets from Whom? Following the Money in Global Health Finance’. Current Anthropology 56 (S12): S306–16. https://doi.org/10.1086/683271.
Escobar, Arturo. 1995. Encountering Development: The Making and Unmaking of the Third World. Princeton, NJ: Princeton University Press.
Farmer, Paul, Arthur Kleinman, Jim Kim, and Matthew Basilico, eds. 2013. Reimagining Global Health: An Introduction. Berkeley: University of California Press.
Fassin, Didier. 2007. ‘Humanitarianism: A Nongovernmental Government’. In Nongovernmental Politics, edited by Michel Feher, 149–60. Cambridge, MA: The MIT Press.
Ferguson, James, and Akhil Gupta. 2002. ‘Spatializing States: Toward an Ethnography of Neoliberal Governmentality’. American Ethnologist 29 (4): 981–1002. https://doi.org/10.1525/ae.2002.29.4.981.
Fisher, William F. 1997. ‘Doing Good? The Politics and Antipolitics of NGO Practices’. Annual Review of Anthropology 26: 439–64. https://doi.org/10.1146/annurev.anthro.26.1.439.
Fowler, A. 1991. ‘Building Partnerships between Northern and Southern Development NGOs: Issues for the 1990s’. Development in Practice 1 (1): 5–18. https://doi.org/10.1080/096145249100076011.
Fowler, Alan F. 2000. ‘Beyond Partnership: Getting Real about NGO Relationships in the Aid System’. IDS Bulletin 31 (3): 1–13. https://doi.org/10.1111/j.1759-5436.2000.mp31003001.x.
Gautam, Manish. 2016. ‘36 Fake Docs in CIB Net’. Kathmandu Post, 20 June. http://kathmandupost.ekantipur.com/news/2016-06-20/36-fake-docs-in-cib-net.html.
Geissler, P. Wenzel. 2013. ‘The Archipelago of Public Health Comments on the Landscape of Medical Research in Twenty-First- Century Africa’. In Making and Unmaking Public Health in Africa: Ethnographic and Historical Perspectives, 231–56.Cambridge:Cambridge Centre of Africa Studies Series.
Geissler, P. Wenzel. 2015. ‘Introduction: A Life Science in Its African Para-State’. In Para-States and Medical Science: Making African Global Health, edited by P. Wenzel Geissler, 1–44. Durham, NC: Duke University Press.
Gerrets, Rene. 2015. ‘International Health and the Proliferation of ‘Partnerships’: (Un)Intended Boost for State Institutions in Tanzania?’ In Para-States and Medical Science: Making African Global Health, edited by P. Wenzel Geissler, 179–206. Durham, NC: Duke University Press.
Harper, Ian. 2014. Development and Public Health in the Himalayas: Reflections on Healing in Contemporary Nepal. London: Routledge.
Himmelstein, David U. Elizabeth Warren, Deborah Thorne, and Steffie Woolhandler. 2005. ‘Illness and Injury as Contributors to Bankruptcy’. SSRN, 8 February. https://doi.org/10.2139/ssrn.664565.
IRIN. 2014. ‘Rude Health: Fear and Violence in Nepal’s Medical System’. 21 March. http://www.irinnews.org/report/99818/rude-health-fear-and-violence-nepal’s-medical-system.
Kalaunee, S. P., and Ryan Schwarz. 2017. ‘Public-Private Partnerships: New Model for Healthcare’. The Himalayan Times, 1 February.
Kamat, Sangeeta. 2004. ‘The Privatization of Public Interest: Theorizing NGO Discourse in a Neoliberal Era’. Review of International Political Economy 11 (1): 155–76. https://doi.org/10.1080/0969229042000179794.
Kapilashrami, Anuj, and Oonagh O’Brien. 2012. ‘The Global Fund and the Re-Configuration and Re-Emergence of “Civil Society”: Widening or Closing the Democratic Deficit?’ Global Public Health 7 (5): 437–51. https://doi.org/10.1080/17441692.2011.649043.
Karkee, Rajendra, and Jude Comfort. 2016. ‘NGOs, Foreign Aid, and Development in Nepal’. Frontiers of Public Health 4, Article 177. https://doi.org/10.3389/fpubh.2016.00177.
Kathmandu Post. ‘Dr. Govinda K.C. Launches 13th Hunger Strike’. Kathmandu Post, 10 October. http://kathmandupost.ekantipur.com/news/2017-10-06/dr-govinda-kc-launches-13th-hunger-strike.html.
Kenworthy, Nora. 2016. ‘Governing through Production: A Public-Private Partnership’s Impacts and Dissolution in Lesotho’s Garment Industry’. In Case Studies on Corporations and Global Health Governance: Impacts, Influence and Accountability, edited by Nora Kenworthy, Ross MacKenzie, and Kelley Lee, 11–26. Rowman and Littlefield International.
Klees, Steven J. 2002. ‘NGOs: Progressive Force or Neo-Liberal Tool?’ Current Issues in Comparative Education 1 (1): 49–54.
Kochanek, Kenneth D., Sherry L. Murphy, Jiaquan Xu, and Elizabeth Arias. 2017. ‘Mortality in the United States, 2016’. NCHS Data Brief 2093, December.
Koplan, Jeffrey P., T. Christopher Bond, Michael H. Merson, K. Srinath Reddy, Mario Henry Rodriguez, Nelson K. Sewankambo, Judith N. Wasserheit. 2009. ‘Towards a Common Definition of Global Health’. Lancet 373 (9679: 1993–95. https://doi.org/10.1016/S0140-6736(09)60332-9.
Krieger, Nancy. 2004. Embodying Inequality: Epidemiologic Perspectives. Amityville, NY: Baywood Publications.
Kruk, Margaret E., Dennis Porignon, Peter C. Rockers, and Wim Van Lerberghe. 2010. ‘The Contribution of Primary Care to Health and Health Systems in Low- and Middle-Income Countries: A Critical Review of Major Primary Care Initiatives’. Social Science and Medicine 70 (6): 904–11. https://doi.org/10.1016/j.socscimed.2009.11.025.
Lamichhane, Subhas. 2016a. ‘Doctors under Threat’. Kathmandu Post, 1 July. http://kathmandupost.ekantipur.com/news/2016-07-01/doctors-under-threat.html.
Lamichhane, Subhas. 2016b. ‘Operation Quack’. Kathmandu Post, 17 July. http://kathmandupost.ekantipur.com/news/2016-07-17/operation-quack.html.
Latschan, Thomas. 2015. ‘Stateless in Nepal: How a Patriarchal System Denies Citizens to Millions?’ Deutsche Welle, 1 January. http://www.dw.com/en/stateless-in-nepal-how-a-patriarchal-system-denies-citizenship-to-millions/a-18223750.
Lee, Cynthia. 2014. ‘The Rise of Global Health Crowdfunding Platforms’. Global Health Governance, 14 July. https://blogs.shu.edu/ghg/2014/07/14/the-rise-of-global-health-crowdfunding-platforms/.
Macinko, J., B. Starfield, and T. Erinosho 2009. ‘The Impact of Primary Healthcare on Population Health in Low- and Middle-Income Countries’. Journal of Ambulatory Care Management 32 (2): 150–71. https://doi.org/10.1097/JAC.0b013e3181994221.
Maes, Kenneth, Brandon Kohrt, and Svea Closser. 2010. ‘Culture, Status and Context in Community Health Worker Pay: Pitfalls and Opportunities for Policy Research. A Commentary on Glenton et al’. Social Science and Medicine 71 (8): 1375–78. https://doi.org/10.1016/j.socscimed.2010.06.020.
Magar Angel, and Kamana Subba. 2012. ‘Strengthening District Health Care Systems Through Partnership with Academic Institutions: The Social Accountability of Medical Colleges in Nepal’. Journal of the Nepal Medical Association 52:142–47.
Mahat, Agya, Madhusudan Subedi, and David Citrin. 2017. ‘Assaulting the Caregivers: On the Rise of Workplace Violence in the Healthcare Sector’. Nepali Times, 22–28 September. http://archive.nepalitimes.com/article/Nation/Assaulting-the-caregivers,3957.
Makary, Martin A., and Daniel Michael. 2016. ‘Medical Error: The Third Leading Cause of Death in the US’. British Medical Journal (Online) 353: i2139. https://doi.org/10.1126/bmj.i2139.
Mallapaty, Smriti. 2014. ‘Lone Hunger Striker Spurs Nepal to Action’. Nature, 18 February. http://www.nature.com/news/lone-hunger-striker-spurs-nepal-to-action-1.14735.
Marsh, Henry. 2015. ‘The Biggest Victim of a Doctors’ Strike Would Be Trust in the Medical Profession’. The Guardian, 21 October. https://www.theguardian.com/commentisfree/2015/oct/21/doctors-strike-medical-profession-nhs.
Maru, Duncan, and Surendra Uprety. 2015. ‘The High Costs of Nepal’s Fee-For-Service Approach To Health Care’. Health Affairs Blog, 20 July. https://www.healthaffairs.org/do/10.1377/hblog20150720.049382/full/.
McClellan, Mark, James Kent, Stephen J. Beales, Samuel I. A. Cohen, Michael Macdonnell, Andrea Thoumi, Mariam Abdulmalik, et al. 2014. ‘Accountable Care around the World: A Framework to Guide Reform Strategies’. Health Affairs 33 (9): 1507–15. https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2014.0373.
McCoy, David, Nele Jensen, Katharina Kranzer, Rashida A. Ferrand, and Eline L. Korenromp. 2013. ‘Methodological and Policy Limitations of Quantifying the Saving of Lives: A Case Study of the Global Fund’s Approach’. PLoS Medicine 10 (10): e1001522. https://doi.org/10.1371/journal.pmed.1001522.
Miley, Marissa. 2014. ‘Public-Private Partnerships: A ‘Win-Win’ for Global Health?’ Public Radio International. 18 July. https://www.pri.org/stories/2014-07-08/public-private-partnerships-win-win-global-health.
MoHP (Ministry of Health and Population0. 2010. Nepal Health Sector Programme – Implementation Plan II (NHSP – IP2). 2010–2015. Kathmandu: Government of Nepal.
MoHP. 2012. State Non-State Partnership Policy for the Healthcare Sector in Nepal – Final Draft.Kathmandu: Government of Nepal, Ministry of Health and Population.
MoHP. 2013. Human Resources for Health, Country Profile: Strengthening Health Systems – Improving Services. Kathmandu: Government of Nepal, Ministry of Health and Population.
MoHP. 2015. Nepal Health Sector Strategy (2015–2020). Kathmandu: Government of Nepal, Ministry of Health and Population.
Mishra, Shiva Raj, and Pawan Acharya. 2013. ‘What Is Fueling Privatization in Health Care in Nepal?’ Health for All 1 (1): 7–11. http://www.nepjol.info/index.php/JHFA/article/view/8489.
Mishra, Shiva Raj, Pratik Khanal, Deepak Kumar Karki, Per Kallestrup, and Ulrika Enemark. 2015a. ‘National Health Insurance Policy in Nepal: Challenges for Implementation’. Global Health Action 8 (1): https://doi.org/10.1177/2333392814566508.
Mishra, Shiva Raj, Nirajan Kandel, Narayan Subedi, and Vishnu Khanal. 2015b. ‘Variation in Prices of Cardiovascular Drugs in Public and Private Pharmacies in Nepal’. Health Services Research and Managerial Epidemiology 2: 1–6. https://doi.org/10.1177/2333392814566508.
Mitchell, Mark. 2014. An Overview of Public-Private Partnerships in Health. Cambridge, MA: Harvard T. H. Chan School of Public Health.
Nagar, Richa and Amanda L. Swarr. 2010. ‘Introduction: Theorizing Transnational Feminist Praxis’. In Critical Transnational Feminist Practice, edited by Richa Nagar and Amanda L. Swarr, 1–23. Albany: State University of New York Press.
Ngcamphalala, Cebisile and John E. Ataguba. 2018. ‘An Assessment of Financial Catastrophe and Impoverishment from Out-of-Pocket Health Care Payments in Swaziland.’ Global Health Action 11 (1): 1–9. https://doi.org/10.1080/16549716.2018.1428473.
National Research Council and Institute of Medicine. 2013. ‘U.S. Health in International Perspective: Shorter Lives, Poorer Health’. In Panel on Understanding Cross-National Health Differences among High Income Countries, edited by Steven H. Woolf and Aron Laudan, Committee on Population, Division of Behavioral and Social Sciences and Education, and Board on Population Health and Public Health Practice, Institute of Medicine. Washington, DC: The National Academies Press.
Nichter, Mark. 2008. Global Health: Why Cultural Perceptions, Social Representations, and Biopolitics Matter. Tucson: University of Arizona Press.
Ong, Aihwa, and Stephen J. Collier, eds. 2005. Global Assemblages: Technology, Politics, and Ethics as Anthropological Problems. Malden, MA: Blackwell.
Pearson, M. 2004. Issues Paper: The Case for Abolition of User Fees for Primary Health Services. London: DFIR Health Systems Resource Centre.
Packard, Randall. 2016. A History of Global Health: Interventions into the Lives of Other Peoples. Baltimore, MD: Johns Hopkins University Press.
Peters, David H., and Traci Phillips. 2004. ‘Mectizan Donation Program: Evaluation of a Public-Private Partnership’. Tropical Medicine and International Health 9 (4): A4–15. https://doi.org/10.1111/j.1365-3156.2004.01209.x.
Pfeiffer, James. 2003. ‘International NGOs and Primary Health Care in Mozambique: The Need for a New Model of Collaboration’. Social Science and Medicine 56 (4): 725–38. https://doi.org/10.1016/S0277-9536(02)00068-0.
Pfeiffer, James. 2013. ‘The Struggle for a Public Sector: PEPFAR in Mozambique’. In When People Come First: Critical Studies in Global Health, edited by João Biehl and Adriana Petryna, 166–81. Princeton, NJ: Princeton University.
Pfeiffer, James and Rachel Chapman. ‘Anthropological Perspectives on Structural Adjustment and Public Health’. Annual Review of Anthropology 39 (1): 149–65. https://doi.org/10.1146/annurev.anthro.012809.105101.
Pfeiffer, James, Wendy Johnson, Meredith Fort, Aaron Shakow, Amy Hagopian, Steve Gloyd, Kenneth Gimbel-Sherr. 2008. ‘Strengthening Health Systems in Poor Countries: A Code of Conduct for Nongovernmental Organizations’. Health Policy and Ethics 98 (12): 2134–40. https://doi.org/10.2105%2FAJPH.2007.125989.
Plumer, Bradford. 2005. ‘Privatizing Global Health’. Mother Jones, 31 May. http://www.motherjones.com/politics/2005/05/privatizing-global-health/.
Rai, Bhrikuti. 2013. ‘Doctor Who?’ Nepali Times, 10 May.
Rajak, Dinah. 2011. In Good Company: An Anatomy of Corporate Social Responsibility. Stanford, CA: Stanford University Press.
Ramiah, Ilavenil, and Michael Reich. 2005. ‘Public-Private Partnerships and Antiretroviral Drugs for HIV/AIDS: Lessons from Botswana’. Health Affairs 24 (2): 545–51. https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.24.2.545.
Rankin, Katharine Neilson. 2004. The Cultural Politics of Markets: Economic Liberalization and Social Change in Nepal. London: Pluto Press.
Raut, Anant, Poshan Thapa, David Citrin, Ryan Schwarz, Bikash Gauchan, Deepak Bista, Bibhu Tamrakar, et al. 2015 ‘Design and Implementation of a Patient Navigation System in a Rural District Hospital in Nepal: Improving the Patient Experience in Resource-constrained Settings’. Healthcare: The Journal of Delivery Science and Innovation 3 (4): 251–57. https://doi/org/10.1016/j.hjdsi.2015.09.009.
Ravishankar, Nirmala, Paul Gibbons, Rebecca J. Cooley, Katherine Leach-Kemon, Catherine M. Michaud, Dean T. Jamison, and Christopher J. L. Murray. 2009. ‘Financing of Global Health: Tracking Development Assistance for Health from 1990 to 2007’. Lancet 373 (9681): 2113–24. https://doi.org/10.1016/S0140-6736(09)60881-3.
Renmans, Dimitri, Nathalie Holvoet, Christopher Garimoi Orach, and Bart Criel. 2016. ‘Opening the ‘Black Box’ of Performance-based Financing in Low- and Lower Middle-Income Countries: A Review of the Literature’. Health Policy and Planning 31 (9): 1297-1309. https://doi.org/10.1093/heapol/czw045.
Richter, Judith. 2004. Public-private Partnerships and International Health Policy Making: How Can Public Interests Be Safeguarded? Helsinki: Ministry of Foreign Affairs of Finland, Development Policy Information Unit.
Robert, Emilie, and Valéry Ridde. 2013. ‘Global Health Actors No Longer in Favor of User Fees: A Documentary Study’. Globalization and Health 9: 29. https://doi.org/10.1186/1744-8603-9-29.
Robertson, Adam, and Shisham Mishra. 1997. Forced to Plough: Bonded Labour in Nepal’s Agricultural Economy. London: Anti-Slavery International.
Roehrich, Jens K., Michael A. Lewis, and Gerard George. 2014. ‘Are Public-Private Partnerships a Healthy Option? A Systematic Literature Review’. Social Science and Medicine 113: 110–19. https://doi.org/10.1016.j.socscomed.2014.03.037.
Roos, Noralou P., Marni Brownell, and Verena Menec. 2006. ‘Universal Medical Care and Health Inequalities: Right Objectives, Insufficient Tools’. InHealthier Societies: From Analysis to Action, edited by J. Heymann, C. Hertzman, M. L. Barer, and R. G. Evans, 107–31. New York: Oxford University Press.
Rottenberg, Richard, Sally E. Murray, Sung-Joon Park, and Johanna Mugler. 2015. The World of Indicators: The Making of Government of Knowledge through Quantification. Cambridge: Cambridge University Press.
RTI International. 2010. Overview of Public-Private Mix in Health Care Service Delivery in Nepal. Research Triangle Park, NC: RTI International.
Ruckert, Arne, and Ronald Labonté. 2014. ‘Public-Private Partnerships (PPPs) in Global Health: The Good, the Bad and the Ugly’. Third World Quarterly 35 (9): 1598–1614. https://doi.org/10.1080/01436597.2014.970870.
Saito Eiko, Stuart Gilmour, Md Mizanur Rahman, Ghan Shyam Gautam, Pradeep Krishna Shrestha, and Kenji Shibuya. 2014. ‘Catastrophic Household Expenditure on Health in Nepal: A Cross-Sectional Survey’. Bulletin of the World Health Organization 92: 760–67. https://doi.org/10.2471/blt.13.126615.
Sanders, Catherine, and Kimber H. McKay. 2013. ‘The Search for “Strong Medicine”: Pathways to Healthcare Development in Remote Nepal Using GIS’. Technology and Innovation 15 (2): 109–24. https://doi.org/10.3727/194982413X13650843068799.
Sapkota, Ramu. 2015. ‘Manufacturing Fake Doctors’. Nepali Times, 11–17 September.
Schoeni, R. F., J. S. House, G. A. Kaplan and H. Pollack, eds. 2008. Making Americans Healthier: Social and Economic Policy as Health Policy. New York: Russell Sage Foundation.
Shah, Saubhagya. 2002. ‘From Evil State to Civil Society’. In State of Nepal, edited by Kanak Mani Dixit and Shastri Ramachandaran, 137–60. Kathmandu: Himal Books.
Sparke, Matthew. 2011. ‘Global Geographies’. In Seattle Geographies, edited by Michael Brown and Richard Morrill, 48–70. Seattle: University of Washington Press.
Storeng, Katarini T. 2014. ‘The GAVI Alliance and the “Gates approach” to Health Systems Strengthening’. Global Public Health 9 (8): 865–79. https://doi.org/10.1080/17441692.2014.940362.
Storeng, Katarini T., and Dominique P. Béhague. 2014a. ‘“Lives in the Balance”: The Politics of Integration in the Partnership for Maternal, Newborn and Child Health’. Health Policy and Planning 31 (8): 992–1000. https://doi.org/10.1093/heapol/czw023.
Storeng, Katarini T., and Dominique P. Béhague. 2014b. ‘“Playing the Numbers Game”: Evidence-based Advocacy and the Technocratic Narrowing of the Safe Motherhood Initiative’. Medical Anthropology Quarterly 28 (2): 260–79. https://doi.org/10.1111/maq.12072.
Strathern, Marilyn. 2000. Audit Cultures: Anthropological Studies in Accountability, Ethics and the Academy. London: Routledge.
Subedi, Madhusudan Sharma. 2001. Medical Anthropology in Nepal. Kathmandu: Udaya Books.
Sudhamshu, K. C. 2011. ‘Violence in the Health Sectors in Nepal’. Journal of Nepal Medical Association 51 (183): 1–2.
Taylor, Michelle E., and Ian Harper. 2014. ‘The Politics and Anti-Politics of the Global Fund Experiment: Understanding Partnership and Bureaucratic Expansion in Uganda’. Medical Anthropology 33 (3): 206–22. https://doi.org/10.1080/01459740.2013.796941.
Taylor, Wendy, and Amy Lin. 2016. ‘Leveraging Markets for Global Health.’ USAID Impact Blog. https://blog.usaid.gov/2016/05/leveraging-markets-for-global-health/.
Watson, Sam I., Emily B. Wroe, Elizabeth L. Dunbar, Joia Mukherjee, Bertie Squire, Lawrence Nazimera, Luckson Dullie, et al. 2016. ‘The Impact of User Fees on Health Services Utilization and Infectious Disease Diagnoses in Neno District, Malawi: A Longitudinal, Quasi-Experimental Study’. BMC Health Services Research 16 (1): 595. https://doi.org/10.1186/s12913-016-1856-x.
Wendland, Claire L. 2016a. ‘Opening Up the Black Box: Looking for a More Capacious Version of Capacity in Global Health Partnerships’. Canadian Journal of African Studies/Revue Canadienne des Etudes Africaines 50 (3): 415–35. https://doi.org/10.1080/00083968.2016.1266675.
Wendland, Claire L. 2016b. ‘Estimating Death: A Close Reading of Maternal Mortality Metrics in Malawi. In Metrics: What Counts in Global Health, edited by Vincanne Adams, 57–81.Durham, NC: Duke University Press.
World Health Organization. 2008. Maximizing Positive Synergies between Health Systems. Geneva: WHO. http://www.who.int/healthsystems/MaximizingPositiveSynergies.pdf.
Wilkinson, Richard. 1996. Unhealthy Societies: The Afflictions of Inequality. London: Routledge.
Wilkinson, Richard. 2005. The Impact of Inequality: How to Make Sick Societies Healthier. New York: The New Press.
Wilkinson, Richard, and Kate Pickett. 2009. The Spirit Level: Why Greater Equality Makes Societies Stronger. New York: Bloomsbury Press.
Endnotes
1 Back
In 1990, there were only 192 NGOs registered with the council. The number of health-related NGOs registered in 1995 was 110, but grew to more than two thousand in 2008 (RTI International 2010). After the earthquakes in 2015, these numbers also shot up. To be sure, a closer look at which among these are active organizations that regularly mobilize resources to deliver services, or coordinate with government systems in other required ways, would reveal a much smaller number.
2 Back
The twist here on ‘kingdom’ resonates especially in the Nepali context because of the sweeping power the 240-year-old monarchy held in the country until its abolition by a then Maoist-led coalition government in 2008. This was one of the primary demands of the Maoists, who led a decade-long armed uprising against the Nepali state from 1996–2006. Arguably, Shah’s NGOdom has emerged as an even stronger force in Nepal, as the world’s once only Hindu kingdom became the world’s newest federal republic, ruled more and more by NGOs beyond the purview and regulation of a putatively absent state.
3 Back
In the 1990s, Nepal fell in line with the neoliberal drive towards free-market policies and privatization, and NGOs were promoted to fill the gaps in public services that resulted from reduced public spending (cf. Pfeiffer 2003, 726). Their international growth has been widely noted (Edwards and Hulme 1996a, 1996b; Fisher 1997; Klees 2002; Nichter 2008), but perhaps nowhere has this phenomenon been more visible than in Nepal.
4 Back
See Adams et al. (2015) for an excellent discussion of the concept of scaling up vs. vertically in global health projects.
5 Back
We are thankful to Nora Kenworthy for helping to articulate this point.
6 Back
The language of consortiums is also dominant in the field of global health. Funded by e.g. the US National Institutes of Health (NIH) and USAID), consortiums invoke the notion of novel partnerships, often between ‘odd bedfellows’ in the public and private sectors to create ‘impact’ and to ‘translate a business ethos into the health sector’ (cf. Gimbel et al., this issue). For example, a piece entitled ‘Leveraging Markets for Global Health’ on a USAID blog notes how the OPTIMIZE project – led by the Wits Reproductive Health and HIV Institute, and supported by PEPFAR and USAID’s Office of HIV and AIDS and their Center for Accelerating Innovation and Impact – is an ‘innovative consortium [that] brings together an unusually diverse set of partners to draw on expertise in clinical research, market access, and advocate engagement’ with the goals of ‘reducing manufacturing costs, accelerating product registrations in developing countries, and facilitating production planning with more demand visibility’ (Taylor and Lin 2016).
7 Back
In one country-wide effort to deter unlicensed doctors from practicing in Nepal, authorities arrested thirty-six fake doctors (Gautam 2016).
8 Back
Possible is currently conducting research on out-of-pocket expenditures and medical debt in two rural districts where we work. A recent census in part of our catchment area conducted among 3,424 households over three months from June to September 2016 found that 52 percent of all households reported medical debt, with the median debt reported as 214 percent of household monthly expenditures. These results are consistent with a growing body of literature demonstrating that out-of-pocket health expenditures are an important cause of household impoverishment in low-income countries (see, for example Akazili et al. 2017; Ngcamphalala and Ataguba 2018)
9 Back
‘Catastrophic health expenditure’ was defined as spending more than 10 percent of a household’s total budget on health care in the past thirty days.
10 Back
In 2018, this division was renamed the Health Insurance Board.
11 Back
In October 2017, Nepal’s Parliament passed a national insurance act that will make insurance mandatory for all, however, there remains a good deal of confusion about what this will look like in practice, and whether this will, for example, drive patients further towards the private sector and fee-for-service hospitals in the cities, at the cost of strengthening rural facilities (see Awale 2017). People who live near the Possible PPP-run hospitals, for example, which provide all services free of care, often question the value of enrolling in an insurance scheme at all.
12 Back
Even still, one of the authors (DC) is routinely asked how things are going, working at Probable or Promise. So, what’s in a name, really?
13 Back
Dustin Moskovotz left Facebook to cofound Asana in 2008, a web-based, workflow management software that allows teams to collaborate on projects remotely with the goal of increasing transparency, accountability, efficiency.
14 Back
While committed to the capitated approach to financing, in actuality, a true capitated financing model was never achieved. Rather, we received grants directly from the Government of Nepal that varied by year.
15 Back
Reported speech, personal communication with member of PPP (DC).
16 Back
A recent study found that medical errors account for 10 percent of all deaths in the United States, so people there might be more justified in their legal pursuits than one might think (Makary and Michael 2016).