Drone philanthropy?
Global health crowdfunding and the anxious futures of partnership
—
Abstract
 Figure 1. Screenshot of video of Chase Adam’s Y Combinator talk about Watsi’s origins. Source: https://www.youtube.com/watch?v=WlT3UhC7NwQ
Figure 1. Screenshot of video of Chase Adam’s Y Combinator talk about Watsi’s origins. Source: https://www.youtube.com/watch?v=WlT3UhC7NwQWhen Chase Adam strode onto the stage at Y Combinator’s Start-up School in 2013, he looked like any other Silicon Valley techie or ‘thought leader’ (Sessions 2017), dressed in a dark T-shirt and sneakers. Adam’s organization, Watsi, was the first nonprofit entity to ever be supported by Y Combinator, which is widely recognized as Silicon Valley’s most prestigious start-up incubator. Adam had been invited to this forum because he runs what is described as the world’s most successful global health start-up, a crowdfunding platform that promotes and funds the medical needs of patients in other countries.[note 1] With the help of ‘medical partners’ – nonprofit organizations, often founded or based in the global North, who provide medical services in countries in the global South – Watsi identifies patients in need of medical interventions, helps write patient narratives that will appeal to donors, and posts them to its online funding platform. Using its well-curated website, as well as ample social media outlets and partnerships with for-profit companies, Watsi solicits donations from media-savvy donors across the world to support the costs of treatment for featured patients. Most campaigns focus on technical, biomedical interventions for patients in need of critical care, such as reconstructive surgeries, advanced orthopedic care, or even acute malnutrition treatment. As a result, quick, biomedical fixes are prioritized for fundraising, and communication focuses on the ‘success’ of each campaign.
Branding itself as the ‘kickstarter for medical treatments’ (Here and Now 2013), Watsi has taken a relatively clichéd model for global charity – similar to World Vision’s strategy of child sponsorship (Bornstein 2001) – and remade it as something new, evocative of the path-breaking technical power of Silicon Valley. In its organizational culture, the ethics that guide its work, and the ways it tackles global health challenges, Watsi occupies a tenuous and ambivalent space in the ever-growing center of a Venn diagram, situated between Silicon Valley and global health, and between nonprofit organizations and tech start-ups. As Silicon Valley has seized space in the global health and development fields, it has sought to normalize new forms of partnership and ways of knowing – such as the power of big data and the inherent good of public–private partnerships (Adams 2016; Citrin this issue; Gimbel et al. this issue; Mitchell and Sparke 2016; Storeng and Béhague 2017) – while encouraging the ‘disruption’ of institutional forms and modes of practice through the embrace of things like hackathons, ‘failing forward’, and eHealth or m-health technologies (Ahlin 2016; Buckee 2017; Duclos 2015).[note 2] Promising ‘radically transparent’ giving that is ‘powered by technology’ and novel data-gathering practices, Watsi both represents and accelerates these changing norms.
In addition to characterizing global health challenges as problems of technological insufficiency, distribution barriers, and inadequate innovation – problems they appear uniquely situated to help solve – Silicon Valley leaders have increasingly sought to transform and move global health into their own domain of work and purpose. These more fundamental incursions seek to disrupt the very institutions and processes at the core of the global health field. Watsi emerges in response to critiques of traditional global health partnerships (and the institutions that make them up) as inflexible, bureaucratically cumbersome, and prone to corruption (Crane this issue). As anthropologists have documented, traditional modes of global health foster relations among donors, governments, nongovernmental organizations (NGOs), and recipient communities that can be disappointing at best, and politically and socially toxic at worst (Kalofonos 2010; Kenworthy 2017; McKay 2012). Rather than taking direct aim at these practices and attempting to improve them, Watsi, like many start-ups, aims to disrupt and dismantle the broader system of which they are part: the global architecture through which funding is disbursed and health care is delivered.[note 3]
These efforts are reflective of Silicon Valley’s fascination with disruption of all kinds, an economic idea hatched in the 1997 book The Innovator’s Dilemma (Christensen 1997) that has become a cornerstone of Silicon Valley economies and cultures. The central idea of disruptive innovation is that markets, products, and ideas must be fundamentally broken in order for advancement to be made; as Jill Lepore (2014) observes, it is a ‘competitive strategy for an age seized by terror’. Disruption also seems to reflect the social and economic crises brought about by late liberalism: if disruption creates wildly profitable technologies, it does so not only by breaking old economic molds but also by bringing havoc and disruption into the lives of people caught up in its financial machinations, such as the cadres of workers bankrupted or pushed into precarity by the gig economy (Irani 2015). Yet as Lepore (2014) reminds us, disruption is difficult to discern as it unfolds; it becomes apparent only in retrospect, and even those things that appear disruptive may be less fundamentally innovative than many claim them to be: ‘Unless you already believe in disruption, many of the successes that have been labelled disruptive innovation look like something else, and many of the failures that are often seen to have resulted from failing to embrace disruptive innovation look like bad management’. Rather than aim to unpack and analyze the level of actual disruption at work through Watsi, I wish to examine how Watsi’s origins, aims, and values reflect ideals about global health, Silicon Valley, and the role of partnership, and how Watsi imagines and portrays the disruptive innovation of its practices.
Watsi’s values and practices do reflect a relatively new global health ethos that embraces entrepreneurship, individualism, flexibility, and private investment in lieu of more lasting partnerships. Consequently, I examine here the relationships and connections that are enabled in this future space; the subjectivities, anxieties, and values Watsi brings to the fore; and the forms of intimacy and estrangement that are enabled by such connections and relations. Watsi represents, I argue, a new kind of ‘drone philanthropy’[note 4] that contrasts with older forms of partnership, affiliation, and connection among donors, organizations, and individual recipients of aid. Drone philanthropy, as its name implies, enables acute surveillance of recipients and ‘partners’ while introducing new forms of distance and proximity that complicate these relationships. It is a philanthropic connection that bridges the space between donor and recipient not through actual geographic, social, or economic proximity, but through short-term, highly surveilled transactions.
The drone is a powerful icon, as well, because of its actual use in of global health practice, and the growing interdigitation of military and global health institutions as (literal) ‘forces’ combatting disease and promoting security, particularly in Africa (Duffield 2016; Hoffman 2017; Rosen 2017; Sachan 2016). The figure of the drone evokes the kinds of anxiety that recipients of global health aid can feel: the sense of at once being objects to be surveilled, treated, counted, and written about while so much of their lives and concerns remain invisible and unheard (Kenworthy 2017). In what follows, I wish to let the figure of the drone hover and hum above my exploration of Watsi, to both recognize Watsi’s work as a form of drone philanthropy, and to recognize Watsi itself as an organization whose work is suffused with the kinds of anxiety, watchfulness, and contradiction that are used to justify the use of drones as well as to characterize life under the drone. Watsi is a nonprofit whose vision relies upon and feeds deep discomfort with the nonprofit enterprise; it is an organization whose construction of radical transparency is built on strategic opacity and occlusion; it is a disruptive start-up whose core innovation draws on storytelling as a charitable appeal, a strategy that seems quaint and timeworn. Finally, Watsi’s philanthropy invokes the spectre of the drone through its identity, practices, and partnerships, but also through the broader economies of surveillance, disruption, and humanitarianism of which it is a part. As concerns with return on investment, actuarial surveillance, and debt management become ever more rooted in global health practice – including, tellingly, in the World Bank’s promotion of ‘Ebola bonds’ and other humanitarian disaster investment opportunities (see Erikson 2015) – the philanthropic drone becomes less of a novelty item and more of a practical norm in global health partnerships.
Care through self-marketing: The emergence of crowdfunding
Watsi’s start-up success parallels the broader emergence and popularity of crowdfunding platforms for charitable causes. Companies like GoFundMe help individuals, families, and groups to develop their own fundraising campaigns to cover medical costs, alleviate the financial burdens of misfortune and disaster, and bring attention to personal causes. One of the most popular uses of crowdfunding in the United States is to raise money for individual medical procedures and health care-related bills, a phenomenon that underscores the gaps in coverage and shortcomings of the health care system (Berliner and Kenworthy 2017).
The rise of crowdfunding in the global North is paralleled by the growing use of crowdfunding as a financial and organizational modality in the global South, with the emergence of organizations such as Watsi, CaringCrowd, Samahope (now operated by Caring Crowd), and Kangu.[note 5] In addition, more traditional global health institutions are turning to crowdfunding as a fundraising modality, including well-known NGOs like Partners in Health and academic institutions such as the University of California San Francisco. Whereas crowdfunding platforms like GoFundMe enable individuals to create their own campaigns to solicit donations for care from social networks, global health crowdfunding platforms like Watsi tend to hand-pick potential recipients of aid and act as intermediaries by promoting the stories of distant others. Thus, global health ‘crowdfunding’ confounds one of the basic tenents of the crowdfunding industry: the direct connection between fundraisers and their network of donors. Instead, Watsi’s primary role is to act as an intermediary, working exclusively with a limited number of ‘medical partners’ in the global South who can help them find patients in need of treatment, carefully ‘curating’ patients to feature on its website, and translating and writing up patient narratives for a largely anonymous donor audience.
Watsi’s institutional role reflects shifts in the terrain of partnerships towards more private and procapitalist arrangements. As public financing for global health faces increasing threats, corporations, industry leaders, and their private philanthropies are playing an ever more important role as partners and leaders in the global health field (Kenworthy and MacKenzie 2016; McGoey 2015; Mitchell and Sparke 2016; Rajak 2011). ‘As befits an approach that emerged from the Silicon Valley’, writes Edwards (2009, 36), philanthrocapitalists utilize a ‘strategy’ for promoting global health initiatives that ‘is dominated by aggressive revenue generation efforts to promote financial sustainability … and an emphasis on rapid “scaling-up” to meet potential demand’. As Edwards (2009, 36) notes, philanthrocapitalists emphasize a wide array of partnership modalities to achieve these ends: ‘for-profit corporations, public/private partnerships of various kinds, social enterprises, and even profit-making subsidiaries of the new foundations themselves’. These priorities are abundantly evident in Watsi’s work. While early literature on philanthrocapitalism has examined the role of large philanthropic donors like the Bill & Melinda Gates Foundation, smaller, more flexible entities like Watsi – which acts simultaneously as donor, nonprofit organization, and technological platform – represent another important domain of partnership in the changing field of global health.
As studies of philanthrocapitalism largely focus on powerful entities, individuals, and partnerships, its impacts on those who are its intended recipients or beneficiaries can often remain underarticulated. Yet forms of abandonment and what Sparke (2017) calls ‘biological sub-citizenship’ that are enabled by new global health arrangements are acute and pervasive. In most domains where it operates, charitable crowdfunding reflects what Duffield (2016, 147), in a stunning appraisal of information technology, calls the ‘resilience of the ruins’. Writing of new technosciences in humanitarian response, Duffield holds up the forms of abandonment and surveillance enabled by new data informatics against the common claims that technology can build connection, diminish distance, enable remote sensing, and reduce friction. Contesting the ‘affirmatory promise of technoscience to positively empower and create new forms of self-realisation’, Duffield (2016, 147) argues that new technology, borne of a pervasively neoliberal period, ‘locks-in the negativities of actually existing capitalism’. As those in need turn to crowdfunding as an economy of hope and salvation, crowdfunding similarly ‘locks-in’ an economic system where self-marketing is necessary for survival and where donors possess the power to choose deserving individuals for salvation (Berliner and Kenworthy 2017).
Origin stories
Start-ups and nonprofits share a common faith in the power of origin stories. Watsi’s story, as narrated by Adam in his Y Combinator talk, portrays the organization as emerging from the disappointing, untrustworthy world of nonprofits and moving into the competitive, promising landscape of Silicon Valley. Adam tells the audience that he initially came up with the idea for Watsi while serving in the Peace Corps, traveling on a public bus in Costa Rica. But he explains that the impetus for the idea came not from Costa Rica, but from an earlier break in his Peace Corps service, when he returned to the United States and visited San Francisco:
Before I [returned and] saw my friends, I thought they were all going to be miserable. I was the guy that had spent the last five to seven years with nonprofits traveling around the entire world; I figured they were living the Office Space life, working dead-end jobs in cubicles in San Francisco, day in and day out. But that wasn’t the case. My friends were all happy. Every single one of my … friends had an awesome apartment, they actually had girlfriends and boyfriends, they went out, they got to date, they were having fun. … But beyond that, they were working for companies and building products and solving problems that they cared about. They were happy; they had found a way to do good and do well. And in contrast, the six years I had spent traveling around the world working for nonprofits, it seemed slow, it seemed bureaucratic, it seemed underfunded – it didn’t come with the same energy and optimism and innovation that San Francisco had.
Adam’s narrative reflects many of the prominent suspicions and anxieties with which NGOs and governments involved in global health are regarded, and these mingle with the more personal anxieties and feelings of inadequacy that Silicon Valley’s success has projected for millennials who find themselves outside its gilded orbit. Adam tells his audience that before he left San Francisco, he told ‘every single person I knew’ that he was ‘done with’ working for out-of-date NGOs and that he was no longer ‘going to sell my soul’. At this point in his talk he is interrupted by enthusiastic applause. He smiles, and then laughs. He explains that he vowed to ‘come back to San Francisco and … find a way to do well and do good’.
Adam’s idea for how to ‘do good and do well’[note 6] came to him on that bus ride in Costa Rica, as a woman boarded the bus and asked for money to fund her son’s medical treatment. Adam ‘immediately’ ignored her requests, noting that such appeals were commonplace on public buses. But then he realized that others on the bus were actually giving this woman money. He said he could not figure out, ‘why all of these local people trusted this woman when they had never trusted all of the women who had come before’? He realized that she ‘had her son’s medical records with her. She was passing it around the bus … they were grilling her with questions about the doctor or the hospital or the condition’. Adam tells his audience that this moment sparked his idea for crowdfunding that would support medical care in developing countries. Yet it is also a moment that reveals one of the core values at the heart of Watsi’s work: a commitment to accountability, proof, and transparency that will lift the veil of pessimism and doubt with which beleaguered Westerners regard appeals for charity and the work of nonprofit entities in the global South.
The tension between intimacy and distrust, between optimism and skepticism, lies at the root of crowdfunding initiatives in both the global North and South. As my colleague Lauren Berliner and I have explored (2017), on crowdfunding sites like GoFundMe, a politics of suspicion and hierarchies of deservingness make campaigners feel that they must work to document and prove their deservingness, much like the woman on that bus in Costa Rica did. Sites like gofraudme.com reflect the popular fear that acts of intimate generosity can be easily capitalized upon by dishonest campaigners. Some crowdfunders then respond by sharing ever more personal details, including medical bills and health records, efforts at documentation that sacrifice privacy (and sometimes even dignity) in order to foster connections with well-meaning but distant donors. Watsi promotes and rewards this moral and material economy, presenting an apparent suspicion of medical partners to potential donors and combining this with an intimate, individualized form of funding that connects donors directly to patients. This is the core disruptive innovation of its model, and it is worth exploring in more depth what this means for current and future global health models and partnerships.
Radical transparency and nonprofit partnerships
Ultimately, the idea at the heart of Watsi’s work – identify people in need, write compelling stories about their suffering, and advertise those stories to sympathetic donors in the global North who are seeking a personal connection with the recipients of their charity – is hardly novel. It echoes earlier practices of child sponsorship at World Vision and other (largely Christian) organizations, which have repeatedly faced suspicion and public scorn because donations do not go directly to children, or are even solicited on behalf of families without their knowledge (Bornstein 2001; Hadid 2016). But the use of personalized stories and narratives of poor people has been used much more widely by NGOs and celebrity philanthropists, both within and beyond the global health and development fields. This strategy is evoked in equal measure by abolitionist and missionary iconography from the early nineteenth century onwards, by telethons of the 1980s, and in the year-end reports and social media posts of contemporary NGOs.[note 7]
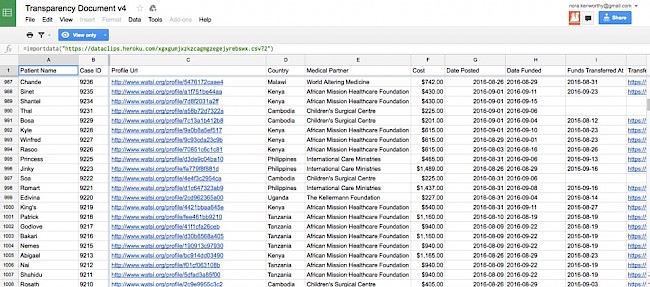
What differentiates Watsi, then, is not the primary aim of its work (enabling charitable donations to and from individuals) nor the sympathetic subjects of its campaigns, but the view it promotes of the global health terrain, the types of partnerships it leverages, and the techniques of surveillance it uses to maintain them. Watsi perceives the global health terrain as one in which inefficient nonprofits run projects that are inscrutable, top heavy, and slow moving. By contrast, Watsi builds an infrastructure for its work that enables seamless, rapid transfers of funds and data. The aspirational ideals of this work are best reflected in a Google spreadsheet Watsi maintains, which is accessed by clicking on the word ‘transparency’ highlighted throughout its website. This spreadsheet is a frequently updated record of every single person funded by the organization; it is a catalogue of individual case data that records how and when medical partners were reimbursed for the costs of treatment, when funds were transferred, and how proof of the medical procedure was documented (Watsi 2017c). Through a commitment to what it calls ‘radical transparency’, Watsi unmasks key operational details that other organizations rarely disclose to the public. Along the way, it encourages its medical partners in various countries to do the same (see African Mission Healthcare Foundation 2017). Similarly, Watsi reassures donors that their money goes directly to patients by publicly releasing records of each patient it has funded, posting how and when money has been transferred to medical partners, and disclosing investigations into the misuse of funds on its blog.
 Figure 3. A tweet from Chase Adam speaks to the organization’s embrace of Silicon Valley values and skepticism about nonprofits.
Figure 3. A tweet from Chase Adam speaks to the organization’s embrace of Silicon Valley values and skepticism about nonprofits.Such efforts to create transparency produce strange new forms of visibility and invisibility: a journalist who covered Watsi’s work in Haiti noted that he was told that a list of ‘patients who died before surgery’, most of them children, could be found in ‘tab 6’ of an organizational spreadsheet (Hankinson 2017). In speaking with Watsi’s in-country partners, it becomes clear that this commitment to radical transparency also occludes willful misunderstandings and flexible financial accounting practices that lubricate work on both sides of the partnership. As other scholars note (Crane this issue; Gimbel et al. this issue; Taylor this issue), these sorts of workarounds can be essential for making global health partnerships functional in the first place. One of Watsi’s partners explained to me that Watsi had instructed them to add as much financial ‘padding’ to their budgeted costs for medical procedures as possible, padding that covers not only items like patient transportation, family support, and food but also the hospital’s infrastructure costs and even the personnel who work full time to manage crowdfunding campaigns. He also noted that, as a partner of Watsi, he viewed the transparency document with significant distrust since the costs of care among different partners varied widely. Commenting on the high price of malaria treatment at one site, he said, ‘I would like to see the break-down of the cost… . If Watsi really wanted to be transparent, I think they need to make public how much money they are asking for what aspect of care’. Such flexible accounting dressed in the garb of transparency has benefits, however. Watsi’s support is more sustainable than it might seem on the surface because it can support these infrastructure costs and direct funds to longer-term health-system building. Yet these costs must also remain hidden from donors (and other partners), as Watsi promises that ‘100% of every donation … directly funds medical treatment’ (Watsi 2017c).
This sort of ‘open-source’ philanthropy leaves other aspects of Watsi’s day-to-day work inscrutable as well. How are patients chosen for campaigns? What happens to those who are not chosen? What half-truths, misunderstandings, or exaggerations enter into the patient narratives featured on the site, which are edited by US-based interns? How are permissions for Watsi’s work negotiated with nonprofit medical partners around the world, and with the individual patients that Watsi reassures us have signed consent documents allowing their stories to be shared? What, if any, in-country ethics review is Watsi’s work subject to, particularly given that it is selecting patients for treatment in contexts where it might not otherwise be available?[note 8] Watsi’s guarantee of ‘100% transparency’ applies only to a specific set of partners and their vantage points. How transparent, for example, are Watsi’s partnerships with hospitals or the transactional decisions made by patients featured on its site? These are questions that are difficult to assess without further access to data, documents, and information on these topics, information that Watsi does not publicly share, despite its transparency policies.[note 9]
Watsi’s practices also occlude other causes that do not – cannot – benefit from workarounds, no matter how creative partner organizations are in their campaigning. Watsi (2017b) stipulates that campaigns cannot ask for funds in excess of US$1,500, and makes clear that partner organizations should put forward patients with treatable conditions that ‘have a high probability of success’. As Watsi (2017b) notes, its ‘mission is to fund low-cost, high-impact healthcare. While we would like to eventually work in the United States, we currently focus our efforts in low income countries because it’s more frequently the case that a relatively small amount of money stands in the way of someone receiving life-changing care’. Watsi repeatedly emphasizes the need for care to be ‘life changing’ in order to be worthy of crowdfunding.[note 10] But what is considered life-changing care? Is blood pressure medicine life changing? Is cancer treatment? What about palliative care? It’s important to note that these parameters, as currently interpreted by Watsi and its partners, not only exclude patients with chronic, ongoing medical needs and unsolvable health problems, but also the kinds of preventative, population-level interventions that might reduce the need for expensive surgeries and treatments in the first place.
Despite the suspicion Watsi cultivates about nonprofits, it not only holds 501(c)(3) nonprofit status itself but demands that all of its partners also hold 501(c)(3) status in the United States. Watsi claims that its partners are ‘some of the most well-respected medical organizations in the world’. Yet its requirements ensure that no funds will go to government-run medical facilities, ministries of health, or even in-country organizations that cannot obtain 501(c)(3) status. Watsi’s rhetoric and public commentary about ‘transparency’ thus reinforces a clear hierarchy of trustworthiness in global health: through its very discursive efforts to discredit ‘traditional’ nonprofits, Watsi reinforces its own status as an arbiter of credibility among other nonprofits. And ironically, Watsi’s partners confirm that it is the very trust they are able to cultivate with Watsi over time that enables them to pad budgets with the kinds of costs that support their broader infrastructure. These sorts of creative workarounds actually enable Watsi donations to support infrastructure among medical partners. But Watsi’s public avowals of scrutiny and suspicion contrast with the implied trust between partners that enables a form of mutually beneficial nontransparency. It is also worth noting that this trust works to build infrastructure for nonlocal NGOs that is made at the expense of local organizations and public sector health institutions, potentially also undermining them through internal brain drain (Sherr et al. 2012).
As with other kinds of partnership, the broader health systems in which Watsi operates affect not only how its services are perceived but also the ethical ramifications of those services. Watsi largely partners with medical nonprofits that provide medical care to patients without charge. Much of this care would otherwise be inaccessible in the health systems of recipient countries, either because the medical procedures are so resource-intensive and advanced, or because public health systems are so depleted that the cost of services is rarely, if ever, covered by the government. In providing these services, Watsi may cultivate a distrust among public-sector health institutions, as patients find (some) specialized care to be possible – and free – in NGO-run partners’ facilities, but not in the public sector. As David Citrin notes in this issue, one of Watsi’s former partners in Nepal, Possible, is a public–private partnership whose role in an increasingly privatized and commodified health system creates friction with its commitment to provide free services and strengthen the public health system.
For Possible and other Watsi partners, existing commitments to providing free services complicate an already contentious ethical terrain. Watsi maintains that patients’ ability to consent to their profiles being written up and posted on its website is essential, but its partners on the ground have explained to me that it would be easier and more transparent to obtain consent from patients if they were seeking care in a fee-for-service environment. This is because Watsi’s support in this environment would directly help patients pay for their medical costs, while also signaling more explicitly to them what it might ‘cost’ to get their care paid for by Watsi, rather than covering the costs of care that would otherwise be shouldered by the NGO. From the perspective of patients and their advocates, why would Watsi cover the costs of care at a facility where treatment is already free, rather than at a government clinic fifteen kilometers away where many kinds of treatment must still be paid for? The current financial arrangement creates a situation whereby patients are not sure what they are consenting to, and partner organizations have a perverse incentive to push patients for consent in order to raise funds for operational and care costs. The desire for a more strictly transactional relationship – one in which what a patient gives for what they get is much more stark, and thus more clear – reflects broader tensions in the ethics of partnership that emerge in the essays in this issue (Boum this issue; Fourie this issue; Okeke this issue). As the essays by Boum and Okeke underscore, perhaps what we can best hope for in partnerships is mutual benefit, in which the terms of the transaction are clear and all parties enter willingly. This stands in contrast to aspirations of partnership based in ideals of power equity or even mutual affection (see Fourie this issue; Taylor this issue).
Drone philanthropy and charity at a distance
As a new financial modality and media form, crowdfunding stitches markets, health care, and data surveillance ever closer together. Writing about the centrality of data and metrics to a financialized, philanthrocapitalist global health enterprise, Vincanne Adams (2016, 45) argues:
These metric practices ultimately invite us to come to terms with a new kind of ‘global sovereign’. This sovereign is a flexible assemblage of data production, number crunching, and scale-up profit sourcing that … orchestrates biopolitical health interventions so that they work within capitalism’s terms and limits and so that they serve the global architecture of neoliberal debt and profit economies.
These norms are reflected in the donor ‘data vacuuming’ described by Gimbel and colleagues in this issue. Watsi’s faith in (selective) data surveillance and its insistence on radical transparency is also consistent with these ‘metric practices’. And yet, simultaneously, patient narratives, photos, and appeals are the central currency of its work. As Adams (2016, 47) recognizes, ‘the compelling case study, the moving story, and the anecdote’ play an equally important role in the contemporary global health field. They hold ‘affective power’ (Adams (2016, 48) that reinforces the legitimacy of metrics: ‘It is perhaps for this reason that having great stories to back them up seems to give them a kind of credibility that, left to their own devices, the raw numbers never really seem to offer’ (Adams (2016, 49).
This is true, but I would argue that what stories also offer is an alchemist’s gift: they help turn metrics into money, by attracting, and making meaning of, the (private) funds that global health relentlessly seeks to acquire in order to keep functioning. Perhaps more than anything else, Watsi has mastered this global health alchemy, turning numbers and technology into money through the selling of easily digestible stories.
In his Y Combinator talk, Adam describes his early fundraising efforts for the site as a ‘complete disaster because I didn’t know what we were selling… . Books [about nonprofit fundraising] told me that I should sell emotion. They said you should go out and tell stories about your patients that make people happy and make them cry’ (Watsi 2017a). He bluntly says that when he did this he ‘felt like a complete fraud’ (Watsi 2017a). Ultimately, he honed in on an ‘incredibly simple’ perspective on Watsi’s work that was highly marketable: ‘if we make the world smaller, we’re gonna make the world better’ (Watsi 2017a). Watsi ‘makes the world smaller’ by carefully curating individualized appeals on its site, and targeting them directly to consumer-donors. But Watsi’s objective is not simply to close the gap between donors and recipients; rather, its objective is to close the gap between donors and their investments, ensuring that everyday donors can trace their money, see its impact, and understand the contexts in which it is used.
Thus, while an early fundraising narrative for a three-year-old girl from Haiti with a congenital heart condition begins ‘Meet Rebecca’ and features compelling photographs, it does not provide the more in-depth narrative of suffering or urgent need that we might expect. ‘Rebecca’s story’ largely features concise descriptions of the treatment process, risks and side effects, alternatives, the heart condition’s impact on her life, and a discussion of cultural and social contexts (Watsi 2015). These texts aim to guarantee that donors’ money will not be misspent; in doing so, narratives on the site transform unique conditions, treatments, and social contexts into ideal types, making patients themselves seem interchangeable. In the section on ‘cultural or regional significance’ on Rebecca’s page, for example, potential donors are told that ‘families in Haiti often have complex cultural mechanisms for understanding cardiac illnesses and their causes… . Nevertheless … parents are willing and cooperative participants in their child’s treatment’. As Watsi has transitioned to having staff at partner organizations write up patient narratives, medical partner staff tell me that they have improved their efficiency in writing these by developing formulaic scripts for common conditions and patient types. Thus, what Watsi builds is a particularly thin sort of affective and narrative relation between donor and patient, one with a patina of personalization but no lasting bonds of obligation.
As with much crowdfunding (whether for new products or life-saving medical procedures), what Watsi sells to consumers is the idea of a solvable problem, so that they can become investors in the kinds of innovative, one-off solutions that drive the Silicon Valley economy (Berliner and Kenworthy 2017). These are aspirational investments as much as they are charitable engagements; one of the more significant groups of donors on Watsi are Chinese WeChat users, who Adam explains are increasingly ‘interested in global philanthropy’ (O’Brien 2015). As Malkki (2015) has reminded us in her ethnography of Finnish humanitarian workers, volunteers, and domestic crafters, such investments have affective value for the donors themselves, allowing them to take on new identities and subjectivities. Donations to Watsi become, then, not just charitable acts of generosity, but discrete investments in human capital. Watsi repeatedly advertises that donors’ money goes further, for example, because it is simply so much cheaper to save a life with a medical procedure in developing country contexts. The underlying message on Watsi’s site is that saving a life elsewhere is not only easy, but inexpensive. Watsi adds value to these investments by carefully selecting patients, aggressively surveilling medical partners for fraud and mismanagement, and transforming singular, needy individuals into interchangeable charitable investments.
This work then produces a unique set of relationships that operate at various registers of proximity and distance. These relationships must simultaneously deploy affective bonds, gift economies, and forms of surveillance in order to facilitate Watsi’s work and uphold its credibility. Watsi’s data-collection efforts and its rhetoric of transparency cultivate a sense among donors that they can surveil their donations from a distance, participating in a kind of drone philanthropy enabled by social media, open-source software, and a faith in big data metrics. The metaphor of drone philanthropy also helps us to understand – indeed, to viscerally feel – the limitations of ideals such as ‘consent’ and ‘privacy’ in crowdfunding platforms. It underscores how patients on Watsi can be at once present – in our inboxes, our social media accounts, our consciousness – and yet be held at great moral, physical, and affective distance.
In their powerful assessment of corporate social responsibility (CSR) efforts, Dolan and Rajak 2011) describe how corporate ethics rely on a strange mix of close affective bonds and social distancing. They note the ‘productive work that distance, dissociation, and detachment perform for CSR, as corporate virtue operates through estrangement as much as intimacy’ (Dolan and Rajak 2011, 6). This proximate distance has been a norm in transnational corporate ethicizing for some time now (see also Kenworthy 2014), but it has become embedded in Watsi’s funding model in new ways. Watsi has borrowed from corporate ‘modalities of ethical governance’ and placed them online, in the hands of consumer-donors. While traditional global health partnerships aspire to close the distance between discrete institutions (universities, nonprofits, donors) in the global North and South, Watsi’s objective is to create a different form of proximity and intimacy across distance. Rather than place human narratives at the center of its work, Watsi privileges marketing strategies that bridge distance without creating lasting bonds or relations of dependence with patients. Watsi (2016) also maintains that it can ‘freeze’ or ‘retire’ its medical partners at any time if they do not comply with its transparency and data-gathering practices.
The drone philanthropy enabled and promoted by crowdfunding platforms like Watsi signals an uncertain (and, at times, anxious) future for global health partnerships. It is a future in which the relationships, institutions, and practices of the past are regarded with suspicion, but recycled into something new; in which faith is invested in those who appear to be held with distrust; in which the subjects of global health charity are both close and distant; and in which radical transparency occludes important ethical and social questions. As a Silicon Valley ethos drives organizations like Watsi to relentlessly pursue the new, the innovative, the data driven, and the technological, it is incumbent on us to draw the cultural and political work they perform nearer, pulling distant forms of the drone into view and critically examining them.
Acknowledgements
I am grateful to all of the participants of the global health partnerships workshop series for their supportive and insightful comments, and especially to Rachel Chapman, David Citrin, Sarah Gimbel, Jenna Grant, James Pfeiffer, and Adam Warren. Thanks as well to Matt Sparke, Thomas Widger, Adia Benton, Pierre Minn, and the participants of the After Global Health panel at the 2017 American Anthropological Association conference for their feedback on this work at various stages. My deepest thanks to Johanna Crane and Lynn Thomas for their collaboration on this project, which was supported in part through grants from the Simpson Center for the Humanities and the Population Health Initiative at the University of Washington.
About the author
Nora Kenworthy is Assistant Professor of Nursing and Health Studies at the University of Washington, Bothell, and Adjunct Assistant Professor of Anthropology at the University of Washington, Seattle. Her recent book, Mistreated: The Political Consequences of the Fight Against AIDS in Lesotho (Vanderbilt University Press, 2017)is an examination of the unexpected political costs and missed opportunities for deepening democracy during the global HIV response. Her more recent research examines the industry and emerging cultures of medical crowdfunding.
References
Adams, Vincanne, ed. 2016. Metrics: What Counts in Global Health. Durham, NC: Duke University Press.
African Mission Healthcare Foundation. 2017. ‘AMHF Transparency Document’. https://app.smartsheet.com/b/publish?EQBCT=7897e1c80bc54f00a0844da05ce571d7.
Ahlin, Tanja. 2016. ‘Time to Pay Attention: E/M-Health and Telemedicine’. Anthropology News June.
Berliner, Lauren S., and Nora J. Kenworthy. 2017. ‘Producing a Worthy Illness: Personal Crowdfunding amidst Financial Crisis’. Social Science & Medicine 187 (August): 233–42. https://doi.org/10.1016/j.socscimed.2017.02.008.
Bornstein, Erica. 2001. ‘Child Sponsorship, Evangelism, and Belonging in the Work of World Vision Zimbabwe’. American Ethnologist 28 (3): 595–622. https://doi.org/10.1525/ae.2001.28.3.595.
Buckee, Caroline. 2017. ‘Sorry, Silicon Valley, But ‘Disruption’ Isn’t a Cure-All’. Boston Globe, January 22. https://www.bostonglobe.com/ideas/2017/01/22/sorry-silicon-valley-but-disruption-isn-cure-all/M9LenqPQnMrbZDlkp0w92O/story.html.
Christensen, C. 1997. The Innovator’s Dilemma: When New Technologies Cause Great Firms to Fail. Boston, MA: Harvard Business School Press.
Donohue, John. 2015. ‘Fail Fast, Fail Often, Fail Everywhere’. The New Yorker, 31 May. https://www.newyorker.com/business/currency/fail-fast-fail-often-fail-everywhere.
Duclos, Vincent. 2015. ‘Global eHealth: Designing Spaces of Care in the Era of Global Connectivity’. Medicine Anthropology Theory 2 (1): 154. https://doi.org/10.17157/mat.2.1.166.
Duffield, Mark. 2016. ‘The Resilience of the Ruins: Towards a Critique of Digital Humanitarianism’. Resilience 4 (3): 147–65. https://doi.org/10.1080/21693293.2016.1153772.
Edwards, Michael. 2009. ‘Gates, Google, and the Ending of Global Poverty: Philanthrocapitalism and International Development’. The Brown Journal of World Affairs 15 (2): 35–42. http://www.jstor.org/stable/24590840.
Erikson, Susan. 2015. ‘The Financialization of Ebola’. Somatosphere, 11 November. http://somatosphere.net/2015/11/the-financialization-of-ebola.html.
Hadid, Diaa. 2016. ‘A World Vision Donor Sponsored a Boy. The Outcome Was a Mystery to Both’. The New York Times, 2 August. https://www.nytimes.com/2016/08/03/world/middleeast/worldvision-palestinians-sponsor-a-child.html.
Hankinson, Andrew. 2017. ‘Swipe Right to Save a Life’. Digg, 11 April. http://digg.com/2017/watsi-crowdfunding.
Here and Now. 2013. ‘Medical Crowdfunding Attracts Top Silicon Valley Investors,’ 8 August. http://hereandnow.legacy.wbur.org/2013/08/08/medical-crowd-funding.
Hoffman, Danny. 2017. ‘African Military Partnerships in the Age of the “Enemy Disease”’. Africa Is a Country, July. http://africasacountry.com/2017/07/african-military-partnerships-in-the-age-of-the-enemy-disease/.
Irani, Lilly. 2015. ‘Difference and Dependence among Digital Workers: The Case of Amazon Mechanical Turk’. South Atlantic Quarterly 114 (1): 225–34. https://doi.org/10.1215/00382876-2831665.
Kalofonos, Ippolytos Andreas. 2010. ‘“All I Eat Is ARVs”: The Paradox of AIDS Treatment Interventions in Central Mozambique’. Medical Anthropology Quarterly 24 (3): 363–80. https://doi.org/10.1111/j.1548-1387.2010.01109.x.
Kenworthy, Nora J. 2014. ‘A Manufactu(RED) Ethics: Labor, HIV, and the Body in Lesotho’s “Sweat-Free” Garment Industry’. Medical Anthropology Quarterly 28 (4): 459–79. https://doi.org/10.1111/maq.12114.
Kenworthy, Nora. 2017. Mistreated: The Political Consequences of the Fight Against AIDS in Lesotho. Nashville, TN: Vanderbilt University Press.
Kenworthy, Nora J., and Ross MacKenzie, eds. 2016. Case Studies in Corporations and Global Health Governance: Impacts, Influence, and Accountability. London: Rowman & Littlefield.
Lepore, Jill. 2014. ‘The Disruption Machine: What the Gospel of Innovation Gets Wrong’. The New Yorker, 23 June. https://www.newyorker.com/magazine/2014/06/23/the-disruption-machine.
Malkki, Liisa. 2015. The Need to Help: The Domestic Arts of International Humanitarianism. Durham, NC: Duke University Press.
McGoey, Linsey. 2015. No Such Thing as a Free Gift: The Gates Foundation and the Price of Philanthropy. New York: Verso Books.
McKay, Ramah. 2012. ‘Afterlives: Humanitarian Histories and Critical Subjects in Mozambique’. Cultural Anthropology 27 (2): 286–309. https://doi.org/10.1111/j.1548-1360.2012.01144.x.
Mitchell, Katharyne, and Matthew Sparke. 2016. ‘The New Washington Consensus: Millennial Philanthropy and the Making of Global Market Subjects’. Antipode 48 (3): 724–49. https://doi.org/10.1111/anti.12203.
O’Brien, Sara Ashley. 2015. ‘The Unlikely Donor to This Silicon Valley Nonprofit? China’. CNN Tech, 24 November. http://money.cnn.com/2015/11/24/technology/watsi-tencent-wechat/.
Rajak, Dinah. 2011. In Good Company: An Anatomy of Corporate Social Responsibility. Redwood City, CA: Stanford University Press.
Rosen, Jonathan W. 2017. ‘Zipline’s Ambitious Medical Drone Delivery in Africa’. MIT Technology Review, 8 June. https://www.technologyreview.com/s/608034/blood-from-the-sky-ziplines-ambitious-medical-drone-delivery-in-africa/.
Sachan, Dinsa. 2016. ‘The Age of Drones: What Might It Mean for Health?’ Lancet 387 (10030): 1803–4. https://doi.org/10.1016/S0140-6736(16)30361-0.
Sessions, David. 2017. ‘The Rise of the Thought Leader: How the Superrich Have Funded a New Class of Intellectual’. New Republic, 28 June. https://newrepublic.com/article/143004/rise-thought-leader-how-superrich-funded-new-class-intellectual.
Sherr, Kenneth, Antonio Mussa, Baltazar Chilundo, Sarah Gimbel, James Pfeiffer, Amy Hagopian, and Stephen Gloyd. 2012. ‘Brain Drain and Health Workforce Distortions in Mozambique’. Edited by J. Jaime Miranda. PLoS ONE 7 (4): e35840. https://doi.org/10.1371/journal.pone.0035840.
Sparke, Matthew. 2017. ‘Austerity and the Embodiment of Neoliberalism as Ill-Health: Towards a Theory of Biological Sub-Citizenship’. Social Science & Medicine 187 (August): 287–95. https://doi.org/10.1016/j.socscimed.2016.12.027.
Storeng, Katerini T., and Dominique P. Béhague. 2017. ‘“Guilty until Proven Innocent”: The Contested Use of Maternal Mortality Indicators in Global Health’. Critical Public Health 27 (2): 163–76. https://doi.org/10.1080/09581596.2016.1259459.
Watsi. 2015. ‘Success! Rebecca from Haiti Raised $1,500 to Treat a Congenital Heart Disease’. https://watsi.org/profile/dce6b8877376.
Watsi. 2016. ‘Medical Partner Manual’. https://docs.google.com/document/d/1j2rq7IYxY_mbTJPRjEYphORmQ-TbQ6kUaKZTvRVTnW8/pub.
Watsi. 2017a. ‘About Us’. https://watsi.org/about.
Watsi. 2017b. ‘FAQ’. https://watsi.org/faq.
Watsi. 2017c. ‘Transparency Document v4’. https://docs.google.com/spreadsheets/d/1tZq47h6jg7NX4ddhTS_H8JFVfLZiDbxwwdQD47_ow64/edit#gid=842368430.
Endnotes
1 Back
While nonprofit ‘success’ is always difficult and problematic to measure, success here is based on Watsi’s recognition in the field of crowdfunding and the amounts of capital and individual donations it has been able to raise. I spoke with staff at multiple medical partners of Watsi (the nonprofit medical providers who put forward patients for crowdfunding, many of whom have worked with a variety of crowdfunding platforms to fund patient treatment), and all agreed that Watsi had emerged as the most successful entity in this domain.
2 Back
Hackathons are short-term events designed to bring many people together to address specific problems or issues using primarily computer programming skills. Failing forward, or the mantra of ‘fail fast, fail often’ is a common invocation in Silicon Valley, where failure is increasingly celebrated as a means of making progress, so much so that there are now failure conferences (FailCons) held around the world (see Donohue 2015).
3 Back
To this end, Watsi announced in 2017 that it was expanding its services to include ‘Watsi coverage’, a novel attempt to provide cheap, technologically enabled health care coverage in Uganda. Because this program has only recently been announced and information about its modality or impact is scanty, I do not discuss it here, though its launch is indicative that Watsi’s disruptive intents reach beyond crowdfunding to health system financing.
4 Back
I am deeply indebted to Rachel Chapman for the suggestion of this term to describe crowdfunding.
5 Back
While each of these global health crowdfunding platforms is different, all focus on crowdfunding primarily for patients in less developed countries. This is typically managed by working with ‘partners’ in these countries who provide direct care to patients. All of the platforms listed require partners to be registered as 501c3 organizations in the United States.
6 Back
This is a common turn of phrase in the philanthrocapitalist and social responsibility realms, but one that is more frequently expressed as ‘doing good by doing well’.
7 Back
I’m thankful to Lynn Thomas for helping make this connection.
8 Back
This is in essence a form of triage with few guiding principles for how patients are selected. Those guiding principles that do exist are stipulated by Watsi, rather than by in-country medical partners, governments, or independent ethical boards.
9 Back
My own attempts to secure interviews with Watsi founders and staff have so far been unsuccessful.
10 Back
I’m thankful to David Citrin for reminding me of this essential point.