Blaming the rat?
Accounting for plague in colonial Indian medicine
—
Abstract
On 18 December 1908, during a debate at the newly formed Royal Society of Tropical Medicine and Hygiene in London, James Cantlie, a physician known for his work on bubonic plague, made a flippant yet revealing remark.[note 1] At issue was a discussion of the rat-flea theory of bubonic plague: the idea that the disease was transmitted to humans from infected rodents via the bite of a flea. Commenting upon this, Cantlie jokingly suggested that ‘we are blaming the rat whereas perhaps the rat would blame man’ (Petrie 1908, 111). This statement’s unusual nature points toward a problematic area for colonial medicine: the interlinking of animal and human agencies and responsibilities at a time of epidemic disease.
Bubonic plague, caused by the bacterium Yersinia pestis, is the disease most commonly thought to have been responsible for the Black Death in the fourteenth century. Modern-day iconography of the Black Death is replete with images of rats as plague carriers, but this idea was unheard of before the turn of the twentieth century. This article examines the process through which plague came to be recognised as a disease that crosses a species barrier from rodents to humans. For all bubonic plague’s association with European history, it was not in Europe that the rodent link was discovered, but rather in the colonial world, during a global event that has come to be described as the Third Plague Pandemic. In India, between 1896 and 1910, the proof of this rodent ‘link’ was laboriously made through the processing of hundreds of thousands of rat bodies in an almost industrial, factory-like setting. These investigations forced plague out of its shadowy historical identity as the ‘Black Death’ and recast it as a disease that could be known at the intersection of humans and animals.
This article stands alone in this special issue in considering what we might think of as the prehistory of zoonosis. While the term ‘zoonosis’ first occurred in the nineteenth century, it appears not to have been applied to the Indian plague in the first decades of the twentieth century, even after the discovery that plague passed from rats to humans. This is not just a point of vocabulary; it points us toward the fact that for colonial doctors, the object of study was never a system of relations, and certainly nothing approaching an ecology. Rather, colonial doctors sought to elucidate the particular agencies of animals and insects, in studies that always sat in uneasy tension with another quite different mode of accounting for plague as a total social phenomenon.
The Indian plague thus confounds many of the features of zoonotic diseases that have made them a topic of pressing concern for contemporary anthropology. That zoonosis has become of interest to anthropologists at precisely this moment in the discipline’s history is not surprising, for zoonosis fits well with our contemporary political and theoretical concerns. Zoonotic diseases emerge from multispecies relations, they blur distinctions between the wild and the domestic, and their study can demand a reassessment of our understanding of scientific knowledge production (Fearnley 2015b). They also throw a spotlight onto the securitisation of life in contemporary biopolitics (Hinchliffe et al. 2013; Keck 2014) that is often linked to questions of pandemic preparedness in relation to emergent disease (Lakoff 2008; Fearnley 2015a; Nguyen 2015). Additionally, zoonotic diseases provide easy application for posthumanist theories that seek to debunk the distinctiveness of the human species, for they lurch sideways upon a virtual plane of possibility with little regard to species barriers. Zoonosis thus beckons to anthropologists in a uniquely enticing way, for it promises a destruction of clean lines and an emergence of the new out of impure mixing.
What, then, can a prehistory of zoonosis in India tell us? For a start, this is not a case that can be understood through contemporary theoretical paradigms such ‘entanglement’ (Nading 2014) or through encompassing ontologies of a ‘multispecies cloud’ (Lowe 2010, 645). In the absence of a broad ecological understanding of plague as a zoonosis, colonial doctors in India were forced to limit their concerns to specific moments of infection, contagion, and transmission. As a result, individual and often disconnected accounts of animal and human agency led to very different levels of explanation in which the question of what happened, how it happened, and why it happened were frequently disconnected. Fundamentally, this led to a situation in which the question of what rats were doing was curiously disentangled from the broader ontological question of what plague was. The scientific production of rodent agency in colonial India must be seen against the background of a broader set of changes occurring in tropical medicine at the time. The introduction of bacteriology, while not leading to the dramatic ‘revolution’ in colonial medicine that is sometimes assumed, did contribute to an important rearrangement in moral understandings of disease. This was a slow shift from understanding tropical climates as spaces that imperilled white health to seeing colonised bodies as the problematic and dangerous carriers of germs (Anderson 1992, 2006). Such developments paralleled those in metropolitan centres, where new germ theories shifted moral discourses around disease so that they focused upon questions of individual responsibility and transgressive bodily habits (Tomes 1997). In India, bacteriology emerged as a moral enterprise for both colonial doctors and for Indian reformers. It introduced new ways of thinking about responsibility and causality, but it also did so in a manner that sometimes reinforced existing ideas about the links between race, germs, climates, and cultures (Chakrabarti 2012, 6). When plague first struck Bombay, Indians were held responsible in a multitude of nonspecific ways. Germ theories suggested that the native body was a site of potential danger, but older ideas about geography and the environment meant that the urban environment, housing, and climate were also all seen as causes of the malady (Kidambi 2004).
I argue that during the Indian plague epidemic, the discovery of animal agency was an important part of this gradual shift in how individual moral responsibilities were understood. This was a situation in which the cross-species potentialities of a zoonotic disease paradoxically led to a strengthening of human categories that were premised on ideas of racial and social purity. It was through intensive work upon the corpse of the rat that colonial authorities came to refashion human moral responsibility. This raises the question of how to talk about zoonotic disease when the subjects of our study employ a hierarchical language that goes against a vocabulary of emergence and becoming. As such, this article can be read as a cautionary note against a trend within the social sciences to see zoonotic disease as something that automatically destabilises anthropocentric human hierarchies.
The Indian plague epidemic
The Indian plague epidemic was part of the so-called Third Plague Pandemic, which emerged in mid-nineteenth-century China, but first gained the attention of outside powers in 1894 when it struck Hong Kong. Over the next few decades, outbreaks of plague occurred in many major cities, including San Francisco, Honolulu, Sydney, Cape Town, and Porto. The label of ‘Third Plague Pandemic’ was applied only later, once retrospective diagnosis had been used to argue that this pandemic was the newest in a series of global events following the Justinian Plague of the sixth century and the Black Death of the middle ages. Although isolated outbreaks of plague had occurred throughout the nineteenth century, the Hong Kong epidemic was the first time in history that the disease came to the attention of scientists trained in bacteriology. There, bacteriologists belonging to the competing schools of Pasteur and Koch, Alexandre Yersin and Kitasato Shibasaburo, simultaneously claimed to have shown that this most famous and feared of historical diseases was indeed caused by a bacteriological agent. In spite of this discovery, however, almost everything else about the aetiology of plague was subject to speculation. This continued to be the case when the disease surfaced for the first time in Bombay in 1896. While the true nature of plague remained subject to debate, Indian authorities were nonetheless confident that through quick and uniquely severe sanitary intervention they might stamp out the disease before it spread beyond the city. Hopes that plague could be quickly squashed through sanitary intervention were nonetheless soon proven false as the disease spread from Bombay, established itself throughout India, and fell into a pattern of yearly recrudescence that lasted for decades. The total number of Indians to die from plague during the Third Plague Pandemic was greater than all other nationalities put together. By 1930, perhaps as many as twelve million people from the subcontinent had perished, mainly from just three provinces: Punjab, the United Provinces, and Bombay (Arnold 1993, 202). Whereas in much of the world the pandemic took the form of isolated flare-ups and outbreaks, in India it became endemic.
Historians have tended to see the initial outbreak of plague in Bombay as precipitating a government response that resulted in a social and political crisis. Colonial officials were thrown into a state of frenzy as the Bombay Plague ‘became the focus of the most terrible anxieties which India evoked in the British imagination’ (Chandavarkar 1992, 111). Plague threatened trade relations with other nations, damaged productivity in India, and for a time it also appeared to be a danger to European life. In 1897, the Indian government passed the Epidemic Diseases Act, which effectively created a state of emergency around plague, and enacted a series of measures in Bombay and the nearby city of Poona that caused widespread popular disturbance. Medical science was in this moment afforded an administrative authority that was unprecedented in India (Arnold 1993, 209–10), and a huge array of measures including forced searches of houses and the removal of infected persons to hospitals were enacted. In the words of the historian Raj Chandavarkar (1992, 208), ‘The city was literally drenched in disinfectant solution’.
An influential account of the Bombay Plague by David Arnold (1993) emphasises how these sanitary measures constituted an ‘assault’ upon the bodies of the colonised, and more recent work by Prashant Kidambi (2004) elucidates how plague policy could also be read as an assault upon the urban environment. The harsh and all-encompassing sanitary measures targeted the environment, people, and urban space in a somewhat indiscriminate fashion. In these early days, colonial policy worked upon an assumption of what Kidambi (2004, 251) calls ‘contingent contagionism’, a multifactorial explanation for plague in which local conditions of poverty and filth were seen to generate contagious disease. Sanitary policies, in other words, appeared to echo the lack of scientific consensus about how to assign responsibility for the epidemic.
By contrast, Indian sources paint a less ambiguous picture of responsibility. The extraordinary sanitary measures produced significant disquiet among the population and in vernacular newspapers. Such concerns never quite amounted to a single unified response, and ‘resistance’ may be too simplistic a term for a longer reaction that involved complex translations and ‘vernacularisations’ of colonial responses to plague (Mukharji 2011). In the short term, however, the government’s plague measures, particularly in the Bombay Presidency, led to disgust, upset, and open dissent in the form of rioting and, in the case of Poona, the assassination of the British officer in charge of plague measures. This crisis – although lasting only for the first few plague seasons – had long-term effects upon both the industrial landscape of Indian cities (Sarkar 2014) and the development of public health in India (Arnold 1993). In the face of this popular unrest and discontent, the most draconian of the plague measures were relaxed and the government eventually accepted that force was counterproductive (Arnold 1993, 236).
This relaxation paved the way for a remarkably laissez-faire attitude to plague over the next two decades, even as it ravaged the Indian countryside killing hundreds of thousands a year. While inoculation was encouraged en masse, few other sanitary policies were pursued with any conviction. For administrators and doctors, however, the epistemological challenge of the disease did not abate with the relaxation of government plague regulations. Indeed, plague continued to disrupt categories and was in some ways unknowable for at least a decade after the initial outbreak in Bombay.[note 2] A simple reading would be to see such confusion abating with the gradual ascendency of the rat-flea theory during this same period of time; this article suggests that things were rather more complicated.
Between 1896 and 1910 the way that colonial doctors and bureaucrats in India talked about plague changed dramatically. New types of agency came to be highlighted, and the role of animals came to be seen as central. The rat’s clichéd symbolic association with plague in wider culture was firmly established. By 1910, rats had become serious actors in plague, and plague was no longer the same disease it had been in 1896. The more new networks emerged at the boundaries of human, insect, and animal life, the more closely the colonial state seemed to associate the disease with the bodies, habits, and customs of Indian people. Any methods to prevent plague by blocking the agency of rats could thus be written off as an ‘impracticable fad’, insofar as they did not address what was seen as the real reason for plague: Indian custom and habit.[note 3] Rats and fleas increasingly came to be seen as causative agents in plague, and yet for the colonial authorities, they never quite got ‘blamed’ in the way that Cantlie imagined.
At one level, this is a story of racial prejudice. Colonial accounts of plague must be viewed in the context of a broader racial discourse in which Indian cultural practices had, since the 1830s, increasingly been seen as pathogenic (Harrison 1999, 154). But there were complexities and disjunctures within this discourse. The initial outbreak of plague in Bombay severely unsettled the colonial state’s sanitary and racial knowledge of its subjects. The state may never have waivered in its assumption that Indians were somehow to blame for plague, but for a short while after 1896, sanitarians were distinctly unclear about how Indians were to blame. The tracing of animal agency led to a restabilisation in the state’s sense that it could know its subjects. Key to this destabilisation was the coexistence of two quite different modes of inquiring into plague that overlapped and informed one another in colonial discourse. Between 1898 and 1905, the Indian government ordered two commissions to investigate plague. Each exemplified a particular mode of asking questions about plague in the first fifteen years of the Indian epidemic. It is only by placing these modes of inquiry side by side that we can begin to understand the disjuncture between colonial accounts of agency and responsibility.
Two modes of inquiry
The plague commissions differed both in their operation and how they asked questions of plague. As massive projects involving multiple actors over long spans of time, they were necessarily driven by multiple rationalities and expectations, but in each of these commissions a distinct mode of inquiry can be ascertained. These two modes of inquiry continued to drive the questions being asked by colonial sanitarians right into the second decade of the twentieth century.
The Fraser Commission
By late 1898, plague was showing little sign of abating in India, and, despite the fact that many in the administration were still self-congratulatory about the government’s antiplague policies, it was becoming increasingly clear that the disease was nonetheless continuing to spread. A resolution was thus passed for the creation of the Indian Plague Commission.
The Indian Plague Commission was one instance of a huge proliferation of commissions in late nineteenth- and early twentieth-century India. The first major commission into a disease had been the Cholera Commission of 1861–1862 (Strachey 1864). In some respects, this was a very similar institution to the Indian Plague Commission: both were expeditionary in character, touring the subcontinent and reconstructing narratives of the disease under investigation. Yet an important difference remained: the earlier cholera commission was tasked only with investigating the sanitary conditions of European soldiers in the army; it was explicitly instructed not to investigate either the pathology or the treatment of cholera. The remit of the plague commission, on the other hand, encompassed aetiology, pathology, and treatment.
The plague commissioners assembled in Bombay on 26 November 1898 under the direction of the physician Thomas R. Fraser. From there they toured the subcontinent until March 1899, holding a total of seventy sittings and taking evidence from 260 witnesses. Some bacteriological work was also conducted, but the questioning of witnesses was the major technique through which the commission sought to produce truth (Fraser 1900c, 5). The commission published transcripts of this entire process in three thick volumes that accompanied their report of 1900. These were, however, very particular kinds of transcripts that allowed only for questions asked by the commission and the enunciations they elicited from witnesses. The evidence preserved in the minutes is therefore never a conversation but rather a particular mode of producing truth from speech. Every piece of evidence that was brought before the committee was recorded as a response to a question, and each question was numbered: in total, 27,415 questions were asked over seventy-two days (Fraser 1900b, 380, 396). When each new witness was brought before the commission, their name was listed, along with the words, ‘called and examined’. If a translator was used, it was noted as ‘(Evidence translated)’ but the original language was never stated.
What remained was therefore a record of interactions that were entirely directed by the commission. There was no sense that anything was guided by the witnesses, even those who were presented as experts. Instead, the commission extracted evidence, one numbered question at a time, and in the process they transformed plague into a thing that could be known through a particular form of speech. Many of the witnesses had submitted a written précis prior to appearing on the stand, but few questions elicited anything not contained in these prior submissions: only through voiced articulation did the evidence under consideration thus come to be established as such. In practice this led to interesting lines of questioning as the commissioners sought to transmute speech into truth, and to extract from narratives of experience knowledge about plague that could not be known from text.
Take, for example, the examination of the Health Officer at Baroda, Mr A. D. Cooper. Having been asked to state his qualifications (Member of the Royal College of Surgeons and Diplomate of Public Health), he was asked in the third question of his interview (question no. 15,320), ‘Have you any evidence to show how plague got into India?’ (Fraser 1900a, 286). This was not an obvious question to ask a witness from Baroda, which was hundreds of miles north of Bombay, plague’s point of entry in India. Unsurprisingly, Cooper had no answer. But the questions continued in such a way as to elicit Cooper’s personalopinion on plague, the next question being, ‘What do you consider are the predisposing causes of plague?’ (Fraser 1900a, 286). Later in the same interview, Cooper was asked for his opinion on quarantine. He started to give an answer that generalised about how quarantine was tried at Surat, Broach, and Baroda, but the commission stopped him in his tracks: ‘I only want facts observed by yourself. You were not at Surat and Broach, and I want your evidence about things you have seen at Baroda’ (Fraser 1900a, 287).
The truth that the commissioners sought thus emerged through a particular form of speech, and could not be gleaned from prior studies, pre-submitted précis, or published papers. But it also sought to capture as broad-as-possible an observation about what plague might be. Advertisements were published in both English-language and vernacular papers encouraging anybody to step forward as a witness to the commission.[note 4] The idea was evidently that the commissioners, as men of judgement, would be able to synthesise understanding out of the vast array of information that generated itself before them. Within the commission’s minutes of evidence, as speech produced truth, there was a levelling of testimony. Hakims – local, traditional medical practitioners – were called to give testimony side by side with European-trained doctors. Quacks and eccentrics – for example those who believed in electrochemical baths as a method of treating plague – likewise took the same witness stand as physicians (Fraser 1900b, 42–45). The commission thus sought to know plague as an expansive arena of social experience.
The end product of this mode of investigation was a report that was a narrative of plague in its totality. It gave detailed histories of plague in each locality investigated; it summarised the ‘character’ of the disease. The report was a layered folding-together of the multiple witness statements and voices, a summation of the anecdotes and experiences grounded in judgements that had been placed before the commissioners (Fraser 1900c). In its own words the commission had aimed to be ‘an investigation of a scientific character’ into the origin of plague, the manner of its communication, and the effectiveness of various curative serums and preventative inoculations (Fraser 1900c, 3). The final report, following pressure from the government of India, attempted to separate out scientific questions from reports of administrative measures, yet it is quite clear that the commissioners felt that such a separation was wholly artificial, for the facts of plague’s origin were, they found, ‘inseparably interwoven’ with the facts of its administration (Fraser 1900c, 3). What thus characterised the mode of investigation pursued by this commission was that the question of plague could not be delineated and purified. The question of knowing plague could not be detached from the experiences of those who witnessed it. Knowing plague was thus an activity enfolded within the moral judgements of these witnesses.
This method, of course, did not necessarily endear the commission to contemporary observers. In a ‘Memorandum on Plague’, sent directly to the Indian viceroy in 1905, W. J. Simpson, a prominent plague scientist who routinely disagreed with everything his colleagues said, dismissed the commission as merely collecting and sifting the ‘undigested opinions’ of just about anybody who had anything to do with plague.[note 5] Yet for all Simpson’s desires that it be more rigorous, the commission represented a form of reasoning about plague that continued to be employed even when a second, more ‘scientific’ commission was established.
The second commission
The Fraser Commission, for all its enormity, made little impact on either administration or science. While it had concluded that rats played a role in human plague, its conclusions as to how this occurred were somewhat vague. The rat-flea theory of plague propagation had in fact been proposed early in the Bombay epidemic by the French Pasteurian, Paul-Louis Simond (1898), and in the following years increasing numbers of physicians in India and abroad began to endorse the primary roles of the rat and the flea in transmitting bubonic plague to humans. Indeed, the suggestion that rat destruction might help prevent human plague had surfaced periodically from the beginning of the epidemic, and some unusual measures, for example the destruction of rats by ‘bacillic infection’, had been experimented with.[note 6] Moreover, international sanitary opinion had moved toward similar notions, with the International Sanitary Conference of 1903 in Paris advocating rat destruction on ships.[note 7]
When a new plague commission was instituted in 1905, it was thus tasked with finally clearing up the precise link between rat plague and human plague in the Indian context. It asked questions of very specific relations between species, and between epidemics and epizootics (widespread diseases among animals). It was furthermore decided from the very beginning that this commission would report in a very different way from its predecessor. There was to be no single, synthesised conclusion. Rather, periodic reports would be forwarded to the government of India, with the scientific results being published mostly under the authors’ own names in The Journal of Hygiene. In a series of special issues, a total of eighty-three papers were eventually published between 1906 and 1917. Initial investigations consisted of epidemiological studies in four villages on the Island of Bombay, and in two ‘isolated’ villages in the Amritsar District of Punjab. Additionally, experimental work was carried out at the Plague Research Laboratory in Parel, Bombay (Lamb 1908). The second commission quickly confirmed the hypothesis that rats were the paramount factor in the spread of plague, and, perhaps more crucially, the commission’s members argued that insanitary conditions had no bearing upon plague, except in so far as such circumstances favoured rat infestations (Lamb 1908, 93). For the remainder of its existence, the commission produced ever more detailed accounts of the various linkages through which plague came to be spread across species boundaries.
For the first commission, plague had been a vast area of inquiry, an ever-expanding problem within the domain of what it meant to be a person living in society. The second commission, by contrast, attempted to account for plague by focusing upon connections. As we shall see, this primarily occurred through laborious work conducted upon the bodies of hundreds of thousands of animals. Through this enormous labour, the second commission reduced the entire phenomenon of plague to a few knowable relationships between and within human and animal worlds.
In the reports of the second commission, we can observe an attempt, through material and discursive labour, to centre accounts of plague on the agency of rats and fleas. And yet such accounts never quite explained plague in the terms of their own experimental work. Other questions that pushed into the margins of these texts offered explanations that lay just beyond the work of the experiments, just beyond the laboratory. The tremendous experimental labour that went into constructing the rat as an agent of plague was never quite enough to make the rat an explanation for plague. To actually explain plague, the commission returned to an idea of the disease as an impure phenomenon, enfolded in the experiences of witnesses: a total social fact that could only be understood as a fault in the customs and habits of the people of India.
Problematic bodies
Human bodily transgressions
It may seem unsurprising that for the British, racial stereotypes about entrenched Indian custom came to explain plague when animal agency could not. While it has been shown that such racial discourses were fairly glacial in their development and change (Harrison 1999), the initial plague outbreak in Bombay nonetheless confused the racial narratives through which colonial science felt it knew Indian society. It was only with the elaboration of rat agency that moral culpability for plague could once again be easily known.
The plague crisis in Bombay led administrators to increasingly panic as they saw the social fabric of the city disintegrating and irrationalities came to echo and reinforce one another (Chandavarkar 1992). As one historian has recently explained, ‘the contagion of plague appeared to travel the streets hand in hand with the contagion of urban breakdown’ (Sarkar 2014, 183). In response to heavy-handed government intervention, unpredictable alliances emerged between Hindus and Muslims, between untouchable sanitary workers and caste-Hindu millworkers, which nonetheless never added up to overall solidarity among the poor. As much as the contagion of disease, the municipal authorities of Bombay began to fear contagious social disorder (Sarkar 2014, 185–87).
If colonial rule operated through the hierarchical arrangement of its subjects – through the knowing of them via their caste and class designations – then plague appeared to shatter these certainties at a corporeal level. Plague was immediately understood by most medical men in India to be a social disease – a disease of filth – and yet early in the epidemic it became worryingly apparent that categories of dirtiness in people did not map onto the disease. Sweepers in Bombay appeared oddly immune to the disease, as did those who removed night soil and were, according to the president of the Plague Research Committee, ‘probably the dirtiest portion of the population’, a fact that could seemingly be explained only by a Darwinian assumption that they were a product of survival of the fittest.[note 8] When plague did spread among the poor in a more straightforward fashion, it was assumed to do so through an improper mixing of bodily fluids arising from the habit of the poor ‘receiving the sputa of the sick in their hands’.[note 9] Neither ‘localist’ nor ‘contagionist’ theories seemed to explain the Indian plague (Hankin 1905), and perhaps more crucially, assumptions about what counted as an insanitary or filthy category of people seemed to align neither with how contemporary accounts of disease predicted plague should spread nor with observations of how plague was spreading.
As such, certain questions continued to worry the British administration. Why was it that prisons – spaces of dirt and moral filth, but also discipline and regulation – had remained immune to plague? How was it possible that 16,500 pilgrims – the quintessential spreaders of disease – could pass through a pilgrim segregation camp in Bombay in one year, and yet none got plague?[note 10] Plague led to a situation in which the British could no longer maintain the fiction that their imperfect understanding of Indian social relations in any way corresponded to the reality on the ground.
Of all the marginal bodies out of place that caused concern to the colonial authorities, those of beggars were most important. At the beginning of 1901, the Bombay government utilised the Epidemic Diseases Act (created at the height of plague panic in 1897) to clear the city of vagrants.[note 11] In Poona, the ‘mendicant class’ likewise continued to arouse a great deal of concern. And yet this concern was not simply a result of homeless people being associated with plague. The real problem was that nobody was quite sure precisely how to make this association.[note 12] Should beggars be inoculated or not? How did they carry the disease? The epistemological uncertainty of plague meant that in the first few years of the twentieth century, even the colonial state’s most rigid categories for what counted as a body-out-of-place could be thrown into doubt. The authorities were certain in their judgement that plague was a disease of filthy people and filthy places, but they could not quite say howthis was so.
In order to regulate and control infectious bodies, the state turned in many places to mass programmes of railway inspection and control of movement through the issuing of a whole series of identification documents, policies that it viewed as more transparent and enlightened than traditional forms of quarantine. In the Madras Presidency in particular, plague passports were issued for those travelling from infected areas. As recent analysis has shown, such documents must be read as attempts to mediate the state’s dual desire to encourage the proliferation of connections that made the empire economically profitable whilst also minimising the dangerous potential of such links (Sriraman 2014, 208).
Categories of understanding were further confused by precisely those state policies that attempted to fix and control the bodies of Indians, particularly in relation to the unprecedented intrusion of the state into private houses early in the epidemic. In both Bombay and Poona, where such policies were pursued under the Epidemic Diseases Act of 1897, the goal was to separate the sick from the diseased and the clean from the filthy. Soldiers forcibly entered private residences and searched for the sick and the dead in order to move problematic bodies into spaces of disciplinary regulation. Disinfecting gangs attended to the spaces of houses as sites of dangerous infection. In short, they sought to remake clear boundaries around people and sanitary spaces.
This intrusion into the private sphere was, however, a transgression that threatened the state’s own image of itself as a power that ruled through detachment. Soldiers who entered houses in this exceptional way reported in their regimental newspaper their discovery of the city as a ‘rabbit-warren’, which was ‘built in the most extraordinary and unmethodical manner’.[note 13] The intimacy of plague created uncomfortable proximities that threatened the fragile epistemological grip that the British felt they had upon the Indian city: from afar they believed that they could comprehend it, but up close its complexities could be dealt with only through revulsion. House-to-house searches also resulted in more immediate confusions of corporeal boundaries. Echoing events of the earlier plague outbreak in Hong Kong, bodies began to be dumped in unexpected spaces in the city as people sought to avoid military intrusion into their homes (Lynteris 2018).
In summary, during the first few plague seasons in India, the government thus found much to be confused and concerned about regarding bodies out of place. Contemporary disease theories seemed ill equipped to explain the spread of plague, which cut across those categories of person – race, class, and caste – upon which the effectiveness of colonial rule was premised. Simultaneously, panicked sanitary policy imperilled these categories further.
The body of the rat
Throughout the early years of the Indian plague, anecdotal evidence regarding the role of rats began pouring in from collectors in rural areas. This led to some concern that a possible shift in policy to focus on the rodents would distract the government from the regulation of transgressive human bodies. In 1900, the sanitary commissioner for Madras wrote that while he accepted the important role of rats in plague transmission, he could not countenance the notion of rats themselves spreading infection in advance of humans, for ‘the acceptance of such an opinion would give much colour to the hopelessness with which some persons are wont to regard the putting forth of sanitary effort to stay the progress of plague by watching the movements of the possibly infected human being’.[note 14] If the rat hypothesis was to coexist at a theoretical level with an idea of human-to-human transmission, it could threaten the disciplinary control of bodies out of place. Such ideas did not last for long, however, and as the rat hypothesis was strengthened – as ever more forms of agency were attributed to the rat and its parasites – it began to act as an ameliorative for a colonial government whose neat categorisations of persons had been so threatened by plague.
Given the long history of discourses about the rat as vermin, there was from the very start of the epidemic a concern about the transgressing rat body: it was a creature that took no notice of social or political distinction as it moved across the indeterminate spaces of the city. The rat’s tendency to hide in crevices and spaces in-between (walls, floors, the decks of ships) made its body a problematic object of extermination. Poisoning rats produced noxious smells as their bodies rotted in these in-between spaces, and it is thus not surprising that a Canadian company, hoping to win contracts with the Indian government by selling them a dream of total rodent eradication, advertised their product, the Common Sense Compound, as ‘curing’ rat carcasses so as to produce corpses without smell.[note 15] The ability of the rat to cross boundaries made it a problematic object of extermination by mechanical means, whilst rat burrows between houses made gas an ineffective and dangerous method of rat destruction.[note 16]
This discourse about rats is, of course, unsurprising. What makes the development of ideas about the rat so interesting during the Indian plague epidemic is that so much work went into stabilising these rodents as known agents in plague rather than as things that were generally transgressive. This led to something of a divergence between the rat as it was understood by the colonial administration and the rat as portrayed in the global circulation of images produced during the Third Plague Pandemic. Very early in the pandemic, and well before the rat-flea theory was in any way generally accepted, we can see in the pandemic’s global visual economy a trend toward the personification of the rat as plague (figure 1). This form of visual identification persists to this day in popular depictions of the disease. The grotesque horror of the plague-carrying rat also occasionally appears in Indian accounts well into the middle of the first decade of the twentieth century, for example in reports by medical officers of rats eating the faces of the corpses of people who died from plague (Bannerman 1906, 183).
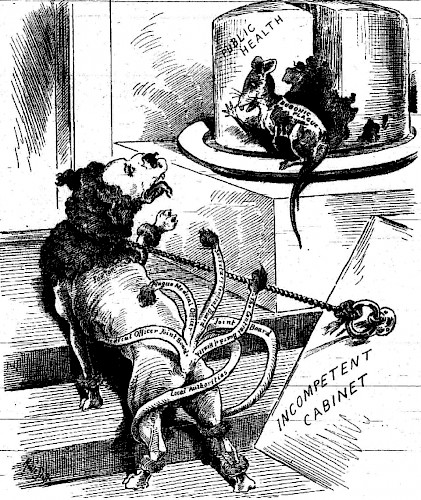 Figure 1. An early example of a personification of the rat as plague, from the Australian paper Worker, 12 May 1900, in an article entitled ‘The Government and the Plague’ (p. 4)
Figure 1. An early example of a personification of the rat as plague, from the Australian paper Worker, 12 May 1900, in an article entitled ‘The Government and the Plague’ (p. 4)Despite this, after 1905 the second plague commission began a sustained effort that led to the transformation of the body of the rat into an unproblematic carrier of plague. Through a laborious process conducted on the bodies of dead rats, their living counterparts were constructed as having a singular kind of agency within plague that was morally unthreatening.
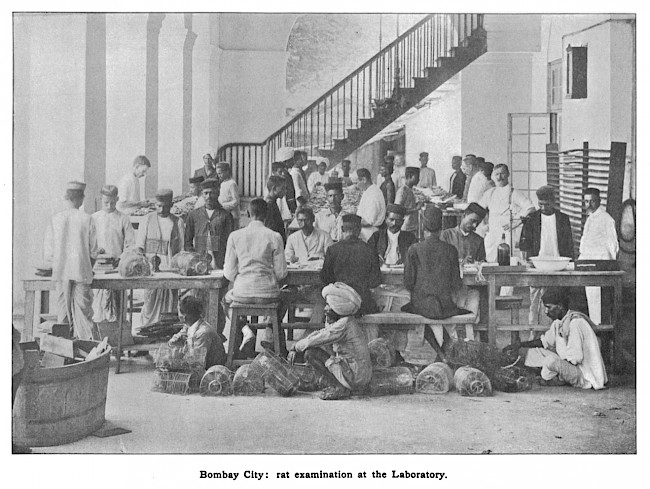
In order to statistically correlate the epizootic to the epidemic, the second plague commission began a programme of mass rat collection and dissection in 1905. Facilities were provided to enable the examination of hundreds of rats from all over the city of Bombay every day, and by 1907, at least 117,000 animals had been caught, killed, and dissected (Plague Commission 1907b, 756). Every single one of these animals was processed in exactly the same fashion in a practice reminiscent of industrialised production, only what was here being ‘made’ was animal agency.
The city’s sweepers were charged with collecting both dead and live rats. The place in which these samples were collected was carefully recorded, before they were sent to the laboratory. Once the rats reached the laboratory they were moved through a long chain of procedures, at each stage of which an ‘unskilled Native assistant’, assumed to be ‘entirely ignorant of the object of his operation’ performed a specific task in which he had been trained.[note 17] Live rats were first killed with chloroform, and a flea count was made. The subsequent process was the same for animals that were brought in dead and alive. Firstly, an ‘Izal-wallah’ would dip the rat in solution of Izal (disinfectant) and wash it. Then a ‘card-wallah’ would attach a card to the fore leg of each rat with the following fields: date, number, catcher, locality, where and how caught, weight, number of fleas, species, sex, pregnant, infected, initials. This was then filled out by a clerk with all details of the rat’s discovery. A ‘weight-wallah’ would subsequently take the weight of the rat, which the clerk would enter onto the card. An attendant would then take the rat to a ‘board-wallah’, who would pin the rat onto a board ready for dissection (see figure 2). The rats would be laid out in rows on long tables. At each table was a ‘cutter up’, although it appears that unlike the other functionaries, the ‘cutter up’ was a European soldier. He would open up the rat and then determine its sex, whether it was pregnant, its species, and the presence of any buboes. All these details would be entered on the card by the clerk. A smear was then taken from any buboes, the slides were collected by an attendant, and a ‘stain-wallah’ applied carbol-thionin blue stain to them.
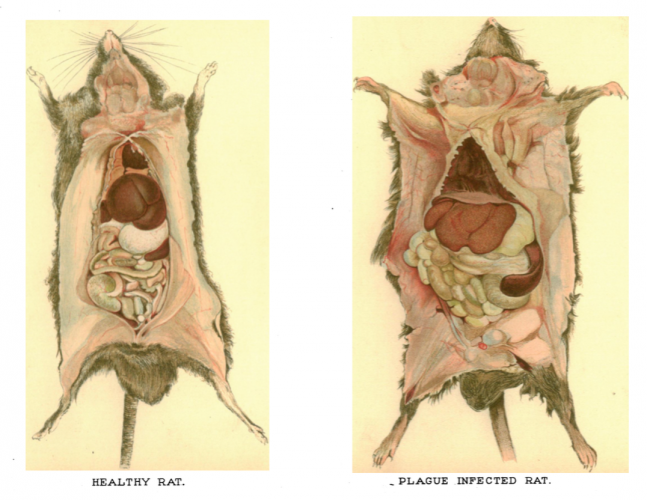 Figure 2. Drawings of healthy and infected rats pinned to the board and dissected Source: Edwin Wilson (illustrator) in Plague Commission (1907a), Plate VII
Figure 2. Drawings of healthy and infected rats pinned to the board and dissected Source: Edwin Wilson (illustrator) in Plague Commission (1907a), Plate VIIThe rat bodies were then placed on numbered shelves in case further examination was deemed necessary, and if there was confusion about the diagnosis, then microscopic examination could be undertaken. This was handled by three or four unskilled microscopists who had been trained to use an immersion lens to examine the slides to identify anything resembling plague. Further diagnosis was provided by a member of the commission, and if any doubt still remained, the committee would test for plague by inoculating a guinea pig with a sample from the spleen of the rat. While this proved a successful initial strategy it was soon discontinued, for the commission ran out of guinea pigs.
This entire process was, as one member of the commission acknowledged, tedious work that confirmed what many had already anticipated (Lamb 1908, 2), yet it is precisely this tedium that I wish to attend to here, for it was through this tedious labour – through a quasi-industrialised process – that Indian clerks and peons and colonial doctors made explicit the rat as a single, known link in the transmission of plague. This is a process that was meticulously recorded, with each stage being photographed in a didactic fashion. In one particularly striking image (figure 3), we see the entire process of the laboratory arrayed in a single scheme, rat traps at the forefront leading to tables for processing rat corpses, and then at the back, three long dissection tables on which the rows of neatly pinned animals can just be discerned. This transformational labour left no room in the state’s interactions with rats for the kind of symbolism that we see circulating in global images of the pandemic. Its effect was to make rats an integral part of plague while at the same time making it impossible for the rat to be personified as plague in figurative and symbolic ways.
As Rohan Deb Roy (2013, 77) notes regarding malaria in the same period in India, contra to the kind of technopolitics described by Timothy Mitchell (2002), the empire in India ‘appears to have thrived on scientific accounts which upheld and advertised straightforward, uncontaminated non-human agency’. Two points need be made here. Firstly, this process of producing agency ultimately did little to alter how colonial authorities asked questions about who and what was responsible for plague. Secondly, we have to deprivilege ‘agency’ as an analytical term and instead begin to account for how situated kinds of agency are produced out of material practices and discursive labour. We have, in other words, to begin to think of ‘agencies’ as things with histories that might have their own vernacular articulations (for an example, see Marrow 2013).
Rat agency and the reinscription of human hierarchies
Once a new kind of agency began to be attributed to rats, the idea that plague would be solvable if only the public took more interest in rat destruction became far more commonplace.[note 18] Such thinking dominated discussion in the wake of the second plague commission. In September 1907, the commission communicated to the government with complete confidence their findings that plague was definitely spread via rats and fleas. The author of the report acknowledged that this did little to make the situation more hopeful, apart from finally enabling the government to dispense with ineffective and expensive measures of disinfection. In terms of what might actually be achieved, however, he was less sanguine: ‘So far as we know at present the only completely effective measure against plague now and for all time would be to re-build the greater number of the towns and villages of India, and even this would not be successful unless the people could be educated to prevent rats coming into the houses’.[note 19] What is more, he advised against any kind of casual trapping of rats, for while total rat destruction could end the Plague, anything less would only discredit antiplague measures, for the population of rats, he argued in a Malthusian idiom, was regulated only by the food supply. Uncovered animal agency had revealed human culpability. Rats were imagined as a self-regulating entity, a population that continually self-stabilised in response to food supply and that was thus subject to regular laws. Humans were the unpredictable factor where blame could lie. To account for plague at a total level thus meant turning back to implicit forms of knowledge about native society.
Nowhere is this demonstrated more clearly than in a paper published by the second commission, ‘Epidemiological Observations in Bombay City’ (Plague Commission 1907b), which described in detail the processing and testing of rat carcasses. Using data obtained from this work, the paper set out to demonstrate a robust statistical link between rat plague and human plague. Interestingly, once the rat had been shown to be a potent if uncomplicated agent of plague, it no longer explained plague. What was needed was thus a return to the kind of reasoning that had characterised the first plague commission. At this point, statistical data became secondary and the report began to build upon the experiences of the commissioners and their common sense judgements drawn from long observation of Bombay. They dismissed the idea that plague was a result of a generalised problem with sanitation, and instead focused upon a very particular kind of problem with the people of Bombay: their relationship to rats. Plague was thus shifted from being a general problem of filth to being a very specific kind of problem in native custom.
As a result of this conceptual shift, many of the elements of plague that had previously been challenging for colonial typologies of natives could be stabilised. One of the confusing aspects of the Indian plague had previously been the fact that modern purpose-built dwellings seemed no more immune to the disease than older insanitary living quarters. The new focus on the improper relationship between Indians and rats now seemed to explain the fact that modern, well-built chawls (tenement blocks) did not seem to prevent plague. The laborious uncovering of rat agency had thus made native bodies and habits knowable and, crucially, judicable, in ways that had never quite seemed possible at the beginning of the epidemic. All those previous questions about why sweepers, prisoners, and pilgrims seemed to get plague in unpredictable ways made sense now that plague was understood as a very specific problem of habit.
There is a question in historical accounts of the Indian plague as to why the government so abruptly ended their intrusive plague policies after the first few seasons of the disease, especially given that neither the spiralling costs nor popular resistance initially dampened their enthusiasm. Chandavarkar (1992, 209) suggests that the policy change occurred once the disease came to be understood as one that afflicted the poor and was unlikely to affect Europeans, becoming something toward which the British felt they could afford to be indifferent. In light of this, it is worth thinking about how the entwining of species in scientific work enabled such judgements to be easily made. Scientific work on plague in India revealed a disease that cared little for boundaries between humans and animals; it revealed a bacterium that crossed the barriers of animal, human, and insect spheres with ease. And yet it was precisely this knowledge that enabled the human sphere to once more become the space under trial.
Accounts of rat agency came to explain failures in state power; they came to explain how categories of knowledge had been so dramatically blurred in Bombay in 1896. We tend to think of zoonosis as a moment of species entanglement, a moment of broken purities and shattered wholes. It is true that in anthropological accounts of contemporary bioscience we find moments that challenge the narratives we tell ourselves about our species. Zoonoses, however, are not stable historical categories. In this particular moment of imperial science, disease shared between species ultimately reinforced the rigidity of existing racial and social hierarchies.
Science and bureaucracy
I have argued thus far that investigations into the Indian plague in the first fifteen years of the epidemic were driven simultaneously by two very different modes of accounting for the disease. It is tempting to associate these forms of accounting for plague as two opposing bureaucratic and scientific rationalities. Discourse, however, shifted between these domains, and it was often administrators who were often most keenly invested in inquiring into the native body and promoting medical theories that supported their claims about it (Sriraman 2014, 286).
At times, distinctions between scientific and administrative rationalities were made clear and apparent. The bacteriologist Waldemar Haffkine, famous for having created an antiplague inoculation of some limited efficacy, was occasionally dismissed not because his work was considered bad, but because it was ‘unsuitable and inconsistent’ with government policy on quarantine.[note 20] The Egyptian Plague Commission, one of a number of foreign delegations that studied the disease, expressed reservations that Haffkine’s confined experience within the laboratory was a danger, for it meant that he might ‘oppose the application of practical sanitary measures’,[note 21] the implicit idea being that laboratory rationality was in conflict with managerial acumen in disease control.
Such concerns, however, attached themselves primarily to Haffkine, who despite being an invaluable asset to the British, was also a somewhat scorned outsider: a Russian, Jewish Pasteurian, who in the eyes of the British administration was inclined to tantrums and excessive pride (see also Kumar 1999).[note 22] We cannot simply associate these two modalities of reasoning with science and policy. The first plague commission – which ultimately came to see plague as a total social phenomenon – was nonetheless instructed by the viceroy not to investigate segregation and quarantine, that is, matters of government policy. The members of this commission were professional men, ‘ignorant’ of administration, and it was feared that they might condemn such policies in precisely that document which the government hoped could authoritatively speak to the other nations of Europe (Kumar 1999, 252–53). Modalities of questioning crossed lines of demarcation between the professional, the administrative, the scientific, and the medical.
Conclusion
In anthropological and historical studies of zoonoses, we often assume that animal agencies destabilise boundaries and divisions, even in historical settings where scientific practice was radically different from contemporary approaches (see, for example, Jones 2004). We have been less attentive to how scientific inquiry into moments of cross-species transgression might actually serve to re-establish borders and hierarchies. There has been a tendency to think of zoonoses as automatically interesting because they unsettle the distinction between human and animal, and because they can cause the boundaries that separate the natural and the domestic to become blurred.
Rats could be seen to cross certain kinds of boundaries: their burrows were found to link houses in villages and their movements to draw disparate groups together as victims of plague. Yet the discovery of precisely this transgression served, for the colonial government, to re-establish the fixed racial and caste categories through which it ruled. In its first few years, plague troubled the categories upon which colonial ideologies rested. The notion that it was rats that caused the transgression, however, neutralised this threat by exposing the ‘social’ causes of plague to colonial judgement. Most importantly, at no point in the epidemic did rat agency ever threaten the moral explanation for plague given by colonial authorities. To return to the quote by James Cantlie that opened this article, the rat was never actually blamed.
In studies of the Indian plague, it has not always been easy to trace the complex interplay between colonial science and colonial policy. It is, moreover, perhaps too easy to see plague policy as something emerging directly out of theories of disease, albeit ones that were inflected with racial and class prejudice. To understand this situation fully, I argue, we have to attend to how two quite different yet interlinked modalities of reasoning about and accounting for plague guided colonial questioning of the disease. Charting the ways that science and policy interacted in early twentieth-century India means being attentive to how various actors differently framed the question: ‘What is plague?’ It means understanding how a laborious account of rat agency could be quite separate from and yet supportive of another kind of reasoning in which human agency continually re-emerged as the main preoccupation of colonial sanitary policy.
The developments described here must be seen as part of a broader and gradual shift during which multifactorial explanations for disease gave way to singular explanations based upon germ theory. Michael Worboys (2000, 120) has explored how this led to a shift from ‘inclusive’ sanitary measures that left no stone unturned to ‘exclusive’ measures that focused upon a single cause. This can be seen in the fact that inoculation became the only widespread antiplague measure pursued by Indian authorities during the first decade of the nineteenth century. As Pratik Chakrabarti (2012, 55) has shown, this is not surprising, for inoculations and vaccinations were welcomed by many Indians in a way that other intrusive sanitary practices were not. The supposed antipathy of Indians toward vaccination was often an invention of colonial physicians who themselves opposed the new science of bacteriology. The complexity I have tried to capture lies in the fact that the production of animal agency in the laboratory did not produce a sanitary policy that worked upon rats, but rather refocused attention on human behaviour as the moral site of disease.
If before, moral fault for the disease had existed somewhere between a filthy urban environment, a corrupting climate, and the colonised individual, it was now located firmly within the last. The industrial work enacted upon rat bodies rendered them into mechanical links: connections with no morality, such that the whole moral burden of the disease could be shifted to the human realm. The more that the government knew about the rats’ role in plague transmission, the more hopeless it seemed to try and encourage any programme of rat destruction, and the more they gave up on efforts to try and encourage Indians to rat-proof their homes. One must wonder what was being produced in the Parel Laboratory where rats were methodically dissected in the thousands: was it a zoonotic link in the disease, or was it the radicalised image of the stubborn native, impervious to change?
Writing in 1904, the lieutenant-governor of Punjab, Charles Rivaz, encapsulated much of why accounts of animal agency could, for the colonial state, provide no explanation for plague. No amount of scientific investigation could address the problem that was plague, and it did not really matter if any links to rats were discovered. Until people changed their habits, he argued, no prevention could occur. Illustrating this, Rivaz drew an analogy in which he compared Indian custom to the fixed properties of a circle: ‘Mathematical science may discover properties of the circle as yet unknown, but there will be no change in the relation of the circumference to the diameter’.[note 23] What the conceit of this quote misses is that, throughout this epidemic, the supposed ‘inflexibility’ of the native was constantly being created anew at the intersection of two very different modes of reasoning.
Acknowledgements
This research was funded by a European Research Council Starting Grant (under the European Union’s Seventh Framework Programme/ERC grant agreement no. 336564). I would like to thank Lukas Engelmann, Christos Lynteris, and Branwyn Poleykett for their comments and support in the writing of this article. I am thankful to MAT’s anonymous reviewers for their helpful suggestions.
About the author
Nicholas H. A. Evans is a fellow in the Department of Anthropology at the London School of Economics. Between 2014 and 2017 he was a postdoctoral research associate on the ERC-funded project Visual Representations of the Third Plague Pandemic. Nicholas has conducted ethnographic and archival research in India, on topics including religion, uncertainty, and the history of epidemics. With Christos Lynteris, he is coeditor of Histories of Postmortem Contagion: Infectious Corpses and Contested Burials (Palgrave, 2018), and his monograph Far from the Caliph’s Gaze: Being Ahmadi Muslim in the Holy City of Qadian is forthcoming from Cornell University Press.
References
Anderson, Warwick. 1992. “‘Where Every Prospect Pleases and Only Man Is Vile”: Laboratory Medicine as Colonial Discourse’. Critical Inquiry 18 (3): 506–29. https://doi.org/10.1086/448643.
Anderson, Warwick. 2006. Colonial Pathologies: American Tropical Medicine, Race, and Hygiene in the Philippines. Durham, NC: Duke University Press.
Arnold, David. 1993. Colonizing the Body: State Medicine and Epidemic Disease in Nineteenth-Century India. Berkeley: University of California Press.
Bannerman, W.B. 1906. ‘The Spread of Plague in India’. Epidemiology & Infection 6 (2): 179–211. https://doi.org/10.1017/S0022172400002813.
Cantlie, James. 1900. Plague: How to Recognise, Prevent, and Treat Plague. London: Cassel & Company.
Chakrabarti, Pratik. 2012. Bacteriology in British India: Laboratory Medicine and the Tropics. Rochester, NY: University of Rochester Press.
Chandavarkar, Rajnarayan. 1992. ‘Plague Panic and Epidemic Politics in India, 1896–1914’. In Epidemics and Ideas: Essays on the Historical Perception of Pestilence, edited by T. O. Ranger and Paul Slack, 203–40. Cambridge: Cambridge University Press.
Fearnley, Lyle. 2015a. ‘The Disease That Emerged’. Limn 5. http://limn.it/the-disease-that-emerged/.
Fearnley, Lyle. 2015b. ‘Wild Goose Chase: The Displacement of Influenza Research in the Fields of Poyang Lake, China’. Cultural Anthropology 30 (1): 12–35. https://doi.org/10.14506/ca30.1.03.
Fraser, T. R., ed. 1900a. Indian Plague Commission, 1898–99. Minutes of Evidence Taken by the Indian Plague Commission with Appendices. Vol. II. Evidence Taken from 11th January 1899 to 8th February 1899. London: Her Majesty’s Stationary Office.
Fraser, T. R., ed. 1900b. Indian Plague Commission, 1898–99. Minutes of Evidence Taken by the Indian Plague Commission with Appendices. Vol. III. Evidence Taken from 11th February 1899 to 20th May 1899. London: Her Majesty’s Stationary Office.
Fraser, T. R., ed. 1900c. Indian Plague Commission, 1898–99. Report of the Indian Plague Commission with Appendices and Summary. Vol. V.London: Her Majesty’s Stationary Office.
Hankin, E. H. 1905. ‘On the Epidemiology of Plague’. The Journal of Hygiene 5 (1): 48–83. https://doi.org/10.1017/S0022172400002357.
Harrison, Mark. 1999. Climates and Constitutions: Health, Race, Environment and British Imperialism in India 1600–1850. Delhi: Oxford University Press.
Hinchliffe, Steve, John Allen, Stephanie Lavau, Nick Bingham, and Simon Carter. 2013. ‘Biosecurity and the Topologies of Infected Life: From Borderlines to Borderlands’. Transactions of the Institute of British Geographers 38 (4): 531–43. https://doi.org/10.1111/j.1475-5661.2012.00538.x.
Jones, Susan D. 2004. ‘Mapping a Zoonotic Disease: Anglo-American Efforts to Control Bovine Tuberculosis before World War I’. Osiris (2nd series) 19: 133–48. https://doi.org/10.1086/649398.
Keck, Frédéric. 2014. ‘From Purgatory to Sentinel: “Forms/Events” in the Field of Zoonoses’. Cambridge Anthropology 32 (1): 47–61. https://doi.org/10.3167/ca.2014.320105.
Kidambi, Prashant. 2004. ‘“An Infection of Locality”: Plague, Pythogenesis and the Poor in Bombay, c. 1896–1905’. Urban History 31 (2): 249–67. https://doi.org/10.1017/S0963926804002135.
Kumar, Deepak. 1999. ‘“Colony” under a Microscope: The Medical Works of W. M. Haffkine’. Science Technology & Society 4 (2): 239–71. https://doi.org/10.1177/097172189900400205.
Lakoff, Andrew. 2008. ‘The Generic Biothreat, Or, How We Became Unprepared’. Cultural Anthropology 23 (3): 399–428. https://doi.org/10.1111/j.1548-1360.2008.00013.x.
Lamb, George. 1908. The Etiology and Epidemiology of Plague: A Summary of the Work of the Plague Commission. Calcutta: Calcutta Superintendent of Government Printing.
Lowe, Celia. 2010. ‘Viral Clouds: Becoming H5N1 in Indonesia’. Cultural Anthropology 25 (4): 625–49. https://doi.org/10.1111/j.1548-1360.2010.01072.x.
Lynteris, Christos. 2018. ‘Suspicious Corpses: Body Dumping and Plague in Colonial Hong Kong’. In Histories of Post-Mortem Contagion: Infectious Corpses and Contested Burials, edited by Christos Lynteris and Nicholas H. A. Evans, 109–33. New York, NY: Palgrave Macmillan.
Marrow, Jocelyn. 2013. ‘Feminine Power or Feminine Weakness? North Indian Girls’ Struggles with Aspirations, Agency, and Psychosomatic Illness’. American Ethnologist 40 (2): 347–61. https://doi.org/10.1111/amet.12026.
Mitchell, Timothy. 2002. Rule of Experts: Egypt, Techno-Politics, Modernity. Berkeley: University of California Press.
Mukharji, Projit Bihari. 2011. Nationalizing the Body: The Medical Market, Print and Daktari Medicine. Anthem South Asian Studies. London: Anthem.
Nading, Alexander M. 2014. Mosquito Trails: Ecology, Health, and the Politics of Entanglement. Oakland: University of California Press.
Nguyen, Vinh-Kim. 2014. ‘Ebola: How We Became Unprepared, and What Might Come Next’. Hot Spots, Cultural Anthropology website, 7 October. https://culanth.org/fieldsights/605-ebola-how-we-became-unprepared-and-what-might-come-next.
Petrie, G. F. 1908. ‘A Short Abstract of the Plague Commission’s Work in Bombay with Regard to the Rat-Flea Theory’. Transactions of the Royal Society of Tropical Medicine and Hygiene 2 (2): 97–112. https://doi.org/10.1016/S0035-9203(08)90018-3.
Plague Commission. 1907a. ‘XI. The Diagnosis of Natural Rat Plague’. Journal of Hygiene 7 (3): 324–58. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2236248/.
Plague Commission. 1907b. ‘XXII. Epidemiological Observations in Bombay City’. Journal of Hygiene 7 (6): 724–98. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2236259/.
Roy, Rohan Deb. 2013. ‘Quinine, Mosquitoes and Empire: Reassembling Malaria in British India, 1890–1910’. South Asian History and Culture 4 (1): 65–86. https://doi.org/10.1080/19472498.2012.750457.
Sarkar, Aditya. 2014. ‘The Tie That Snapped: Bubonic Plague and Mill Labour in Bombay, 1896–1898’. International Review of Social History 59 (2): 181–214. https://doi.org/10.1017/S0020859014000157.
Simond, P. L. 1898. ‘La Propagation de La Peste’. Annales de l'Institut Pasteur 12: 625–87.
Sriraman, Tarangini. 2014. ‘Assault and Assuage: Identification Documents, Colonial Rationalities and Epidemic Control in British India’. In Critical Studies in Politics: Exploring Sites, Selves, Power, edited by Nivedita Menon, Aditya Nigam, and Sanjay Palshikar, 271–318. New Delhi: Oriental Blackswan.
Strachey, John. 1864. The Second and Third Sections of the Report of the Commissioners Appointed to Inquire into the Cholera Epidemic of 1861 in Northern India: With an Account of the Epidemic by the President of the Commission. Calcutta: O.T. Cutter, Military Orphan Press.
Tomes, Nancy. 1997. ‘Moralizing the Microbe: The Germ Theory and the Moral Construction of Behaviour in the Late-Nineteenth-Century Antituberculosis Movement’. In Morality and Health, edited by Allan M. Brandt and Paul Rozin, 271–94. New York: Routledge.
Worboys, Michael. 2000. Spreading Germs: Disease Theories and Medical Practice in Britain, 1865–1900. Cambridge History of Medicine. Cambridge: Cambridge University Press.
[1] For Cantlie’s own work on plague, see Cantlie (1900).
[2] For the challenges of knowing plague, see Hankin (1905).
[3] Education: Sanitary: A: July 1913, no. 88–102, National Archives of India (NAI).
[4] Summoning of Witnesses of Indian Plague Commission, 1898, General Department, Volume 89, no. 159, Maharashtra State Archives (MSA).
[5] W. J. Simpson, Memorandum on Plague, Sanitary Plague, A, January 1905, no. 71–74, NAI.
[6] Home: Sanitary Plague: A: December 1901, no. 304–305, NAI.
[7] Home: Sanitary Plague: A: August 1909, no. 139, NAI.
[8] Report by Surgeon Major R. W. S. Lyons, I. M. S., President of the Plague Research Committee, Home: Sanitary Plague: B: August 1898, no. 96–98, NAI.
[9] Ibid.
[10] Proposed inquiries into the etiology of plague, Home: Sanitary Plague: A: September 1904, no. 85–87, NAI.
[11] Resolution of Government No. 962–P., 1901, General Department, vol. 93, no. 769, MSA.
[12] 1902, General Department, vol. 83, no. 781, MSA.
[13]The Bugle, 18 March 1897 (p. 1599), Durham County Record Office.
[14] Sanitary Commissioner for Madras, to the Secretary to the Government, Local and Municipal Department, 9 June 1900, Home: Sanitary Plague: A: August 1900, no. 80, NAI.
[15] Home: Sanitary Plague: B: February 1904, no. 127–128, NAI.
[16] Home: Sanitary Plague: A: May 1909, no. 96–97, NAI.
[17] The following description is mostly based upon ‘Organisation and Agency for the Collection and Examination of Bombay Rats for Plague’, appendix to First Progress Report to the Committee, by Martin (7 July 1905), Home: Sanitary Plague: A: April 1906, no. 129–131, NAI. Some details have also been taken from Plague Commission (1907b).
[18] Home: Sanitary Plague: A: April 1903, no. 268–274, NAI.
[19] ‘Measures to Be Taken for Dealing with Plague’, Leslie, 26 July 1907, Home: Sanitary Plague: A: September 1907, no. 190–196, NAI.
[20] Hewett to Government of North-Western Provinces, Home: Sanitary Plague: A: December 1897, no. 563-565, NAI.
[21] Home: Sanitary Plague: A: March 1898, no. 422–443, NAI.
[22] Home: Sanitary Plague: A: May 1904, no. 187–198, NAI.
[23] Demi-official from Rivaz to Ibbestson, Home: Sanitary Plague: A: September 1904, no. 85–87, NAI.
Endnotes
1 Back
For Cantlie’s own work on plague, see Cantlie (1900).
2 Back
For the challenges of knowing plague, see Hankin (1905).
3 Back
Education: Sanitary: A: July 1913, no. 88–102, National Archives of India (NAI).
4 Back
Summoning of Witnesses of Indian Plague Commission, 1898, General Department, Volume 89, no. 159, Maharashtra State Archives (MSA).
5 Back
W. J. Simpson, Memorandum on Plague, Sanitary Plague, A, January 1905, no. 71–74, NAI.
6 Back
Home: Sanitary Plague: A: December 1901, no. 304–305, NAI.
7 Back
Home: Sanitary Plague: A: August 1909, no. 139, NAI.
8 Back
Report by Surgeon Major R. W. S. Lyons, I. M. S., President of the Plague Research Committee, Home: Sanitary Plague: B: August 1898, no. 96–98, NAI.
9 Back
Ibid.
10 Back
Proposed inquiries into the etiology of plague, Home: Sanitary Plague: A: September 1904, no. 85–87, NAI.
11 Back
Resolution of Government No. 962–P., 1901, General Department, vol. 93, no. 769, MSA.
12 Back
1902, General Department, vol. 83, no. 781, MSA.
13 Back
The Bugle, 18 March 1897 (p. 1599), Durham County Record Office.
14 Back
Sanitary Commissioner for Madras, to the Secretary to the Government, Local and Municipal Department, 9 June 1900, Home: Sanitary Plague: A: August 1900, no. 80, NAI.
15 Back
Home: Sanitary Plague: B: February 1904, no. 127–128, NAI.
16 Back
Home: Sanitary Plague: A: May 1909, no. 96–97, NAI.
17 Back
The following description is mostly based upon ‘Organisation and Agency for the Collection and Examination of Bombay Rats for Plague’, appendix to First Progress Report to the Committee, by Martin (7 July 1905), Home: Sanitary Plague: A: April 1906, no. 129–131, NAI. Some details have also been taken from Plague Commission (1907b).
18 Back
Home: Sanitary Plague: A: April 1903, no. 268–274, NAI.
19 Back
‘Measures to Be Taken for Dealing with Plague’, Leslie, 26 July 1907, Home: Sanitary Plague: A: September 1907, no. 190–196, NAI.
20 Back
Hewett to Government of North-Western Provinces, Home: Sanitary Plague: A: December 1897, no. 563-565, NAI.
21 Back
Home: Sanitary Plague: A: March 1898, no. 422–443, NAI.
22 Back
Home: Sanitary Plague: A: May 1904, no. 187–198, NAI.
23 Back
Demi-official from Rivaz to Ibbestson, Home: Sanitary Plague: A: September 1904, no. 85–87, NAI.