A journey through chronic illness
An autoethnographic photo essay
—
Introduction
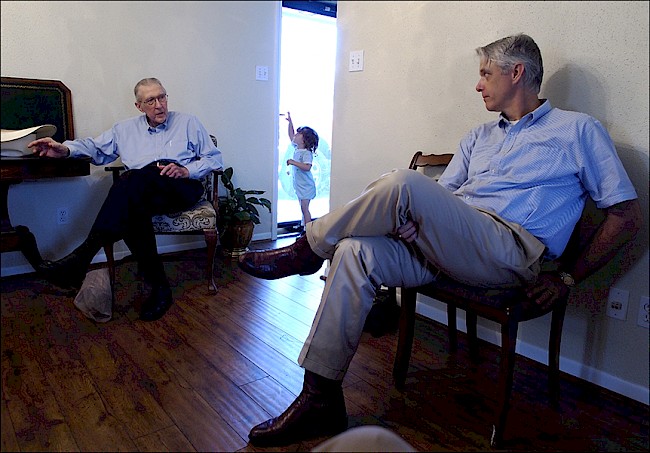
While studying anthropology in graduate school I never thought about how the skills I learned as an ethnographer would prepare me for understanding and processing my father Winston’s multiple chronic illnesses, advocating for him, and facilitating his eventual passing. The decades of living, observing, and working intimately with families in Bolivia and Perú helped me recognize those significant moments in life that we witness and then relive in our memories. As a professor teaching ethics and humanities courses to medical students in the United States, I became acutely aware of the acculturation of biomedicine and the priorities it places on saving lives. At seventy, when Dad’s congestive heart failure manifested to a level that he needed intervention and received his implantable cardioverter defibrillator (ICD),[note 1] I began to consider my own family’s health care as a subject to observe and document.
There, in his hospital room, while my wife and I were visiting, I snapped a few images on my cell phone of him talking with us. Immediately my spouse expressed how inappropriate it was for me to make an image of him (or anyone) convalescing in the hospital. Dad did not flinch, responding, ‘oh, that’s ok, he can take as many as he wants’. A photographer himself, Dad taught me the wonders of working with a camera, thinking about subjects, and mastering the fundamentals of exposure. In that moment we realized his new journey of navigating chronic illness could be a project for us to share, and even though neither of us had any idea where that trip would take us, we trusted each other enough to go together. Dad was not selfish about sharing his journey, indeed, he invited his family to join him and knew he needed our support throughout. In that one moment, we implicitly agreed upon our roles: he would be patient/subject and I would be ethnographer/advocate, and together we would embrace the impending chaos by documenting our steps and sharing his/our story. For this reason I list him as my coauthor on this publication.
In the end, accompanied or not, it was he who took every step, he who persevered, he who trusted his caregivers and the medical system, and he who believed in an eventual positive outcome. As an observer, I witnessed procedures succeed and fail, professionals make mistakes and have amazing insights, and his persistence amidst his suffering. It was the ultimate parallax: as one living through treatment(s), Dad saw his reality quite differently from those around him. Like so many other documentary projects, this photo essay captures how our visions of the same story diverged and aligned. My struggle was to accurately depict the phases of his journey, keeping in mind the multiple audiences, but ultimately knowing we were the only two who would really care about the photos.
Ultimately this photo essay is as much about one patient and his family’s experience with chronic illnesses as it is about visualizing the social and medical structures within which we live. When teaching medical students humanities, ethics, and professionalism, we urge them to try to understand the patient’s context and expectations as much as they do the medical indications. Harder to convey is the culture of medicine and the inherent values within which they will operate as students and future physicians. As ethnographers, we focus on that context, recognizing the patient’s values upon which medical decisions are made. In this case, we consider how a white, well-educated veteran with health insurance and a supportive family navigated a system filled with well-meaning caregivers, top-notch technology, and shelves of pharmaceuticals and still suffered acutely, in ways that medicine strives to avoid. And we are prompted to ask: What happens, then, to people without such resources and access? How much do they suffer, and what happens to them and their families in our system? Where do they die and what is that death like?
Editor’s note: click on images to enlarge or watch as slideshow.
I recall telling a physician-colleague of mine in 2006 about my father’s new ICD. He responded, while shaking his head, ‘congestive heart failure is a terrible death’. Dad’s eventual passing had not occurred to me up until that point; he was stabilized and his prognosis was good. It was only arrhythmia, or atrial fibrillation (AFib). ‘Men like your dad probably only have ten years, max’, he continued. I recognized that ICD devices like his would prolong his life as long as the rest of him remained disease free. In my mind, he was too young to have someone give him ten years; certainly he would beat those odds. Dad’s physicians had treated his AFib with medications for nearly two years before his condition required the ICD. After the initial procedure, it seems Dad did not heed the advice of his electrocardiologist and lifted a heavy object (a car battery), unduly stressing his heart before the device’s cathode was securely anchored in the chamber by scar tissue. The loose wire required a second procedure (image 1).
In January of 2011 Dad reported feeling a hard, cyst-like bump the size of a BB (birdshot pellet) under his right mandible and pointed it out to his physician, as well as a number of his family members. He and his physician adopted a ‘wait-and-see’ approach and monitored its growth. By November of that year the cyst had increased significantly in size, almost to that of a pea or small marble and was painful to the touch. He complained about it affecting his sleep. It was now visible, disfiguring his jawline; he wanted it removed. Dad waited to do anything about it until after the holidays so he could enjoy time with his family and not spend that time recovering.
In January 2012 a surgeon performed a skinny-needle biopsy of the lump (covered by his military health plan) and found that no cancer cells were present. He requested a computerized tomography (CT) scan to know exactly where the cyst was located and scheduled a surgery for 1 February. When the surgeon got in, he found the 3cm x 2cm lump to be on Dad’s salivary gland and indications that the nearby lymph node was completely compromised. As it was scheduled as a cyst removal and not a cancer excision, the surgeon cut to the edge of the affected area as best as he could, removing the entire structure without removing all of the tissue, in other words, leaving ‘positive’ margins or tissue that potentially still contained cancerous cells. The pathology report returned the following week indicated the salivary gland had squamous cell carcinoma in it and metastatic carcinoma was present in a single lymph node.
At a family gathering to celebrate one of his nephew’s birthdays, Dad’s niece gifted him with a pair of Hulk Smash Hands as a way of supporting his fight against cancer. The oncologist subsequently recommended simultaneous radiation and chemotherapy. There would be seven weeks of radiation, five days per week, for five to seven minutes each day. The eventual build-up of radiation would continue to kill cancer cells for up to two weeks following completion of the therapy. After the first two weeks he would experience a ‘sun burn’ on his tongue and throat, making it hard to swallow and eat. Most patients regain 80 to 100 percent of their sense of taste. Even though the physicians expected a full recovery, if there were problems with swallowing he could seek care from a speech pathologist to teach him how to swallow (again); in a worst-case scenario, a feeding tube (percutaneous endoscopic gastrostomy tube) would be administered. We learned from the physicians that many people undergo this treatment and ‘get past it and enjoy their lives’.
 4. Preparing for radiation therapy, 30 April 2012. The mask immobilizes the head and allows the oncologist to pinpoint where the therapy is directed.
4. Preparing for radiation therapy, 30 April 2012. The mask immobilizes the head and allows the oncologist to pinpoint where the therapy is directed.After a full-body positron emission tomography (PET) scan[note 2] revealed cancer only in the region of his neck where his salivary gland had been, the doctors decreased his radiation therapy to six weeks and limited the stronger doses on the affected side of his neck and prescribed lower doses on the opposite side, for seven minutes each day. Dad decided to forgo any surgery and begin radiation and chemotherapy (Erbitux). He returned to the radiation oncologist’s office to have the head/neck mask made and began both treatments on 9 April.
When Dad began his radiation therapy, he enthusiastically drove himself to the hospital; by the middle of the second week, we were taking turns driving because he felt so weak. By the third week Dad’s throat had swollen so much he could not eat solid foods and he said his sense of taste had disappeared (temporarily, he hoped). By the fourth week, pain from the burns on his back and neck were unbearable and his throat was so swollen he could not swallow. He had reached the worst-case scenario: he would have to receive artificial hydration and nutrition through a PEG tube.
Signs of the chemotherapy include an acne-like rash on the arms and upper body; we were told developing the rash indicated that the body was responding to the therapy.
We chatted about the impending PEG procedure while waiting for the gastroenterologist’s arrival in the hospital room. Radiation damaged Dad’s mouth and tongue, so he was not saying too much that morning. Several nights before, I had helped him bathe. Now he required help because the warm water was painful on his skin, and he had trouble standing in the shower and raising his arms to wash. As I dried him off he yelled with each touch of the towel anywhere near his back, shoulders or neck. His screams scared me, as he was not one to express pain much, if ever.
The gastrointestinal doctor entered the room and approached Dad’s bed, introducing himself as the physician who would perform the PEG procedure that day. He said, ‘Tell me Mr. Crowder, on a scale from one to ten, how is your pain today?’ Dad struggled, ‘Good morning, Doctor, nice to see you. I’d say it’s about a seven’. The doctor nodded with acceptance; I looked at Dad incredulously. As the doctor continued with his explanation of where the tube would be placed and what his diet would consist of, my mind returned to the shower/toweling-off incident. After the doctor left us I asked him in disbelief, ‘Seven? Really, seven? If your pain is a seven, what are we doing here? After drying you off the other night, I’d say your pain is an eleven!’ Dad was quiet for a moment, his normal reaction when being cross-examined. ‘Well’, he said, as he summoned some strength to speak, ‘I didn’t want the doctor to be upset with me’.
Dad recovered well following his cancer incident, and now considered himself a ‘survivor’. He continued his regular check-ups with his oncologist, who decided to leave the chemo port in him. Once the swelling in his throat and neck from the radiation abated, his physicians decided to remove the PEG tube as he needed to return to solid foods, which would give him more strength and accelerate his recovery. Dad’s senses of taste and smell never fully returned, but he continued to cook outstanding meals as food was one of his deepest passions.
 7. Three days post-op; diptych of Dad engaging with his technology while in cardiac intensive care, 28 March 2015
7. Three days post-op; diptych of Dad engaging with his technology while in cardiac intensive care, 28 March 2015In order to relieve some chest pain and shortness of breath, in late March 2015 Dad’s cardiologist decided to place a stent (angioplasty) in one of his major arteries. But during the preoperative visit, they said that Dad’s condition warranted a triple bypass, instead. He was immediately checked into the hospital and his surgery was scheduled for the following morning. Just months before, he and my mom had rewritten their wills and completed their advance directives. Dad’s confidence in his doctors and the procedure were steadfast; however, the fact that he was undergoing such a major operation nine years after receiving his ICD underscored how much his condition had worsened.
The cardiac team advised our family that even though heart surgeries are painful, patients often feel better because their blood flow improves significantly. Once awake in recovery, Dad was alert and talkative, saying he felt really good despite the new scar running down his chest. Dad remained in the cardiac intensive care unit (CICU) for a couple of days to monitor his progress. By the third day he was reading, eating, and wanting to go home. Dad used his cell phone to call friends and video called his daughter and her family on the East Coast.
Unlike most heart patients who return home within the week, Dad developed an infection and continued to have AFib issues, requiring him to stay in the hospital for nearly a month following his surgery. These setbacks weakened him considerably. Regular visits from his family and friends could only keep him in good spirits for so long. Frustration set in by the middle of April, as it became apparent that he required more involved care than he could receive at home. Walking, bathing, eating, taking medicine, etc.: all these were difficult for him. He needed a safe environment where he could get the attention necessary to expedite his recovery. Although his insurance covered his excellent surgeons and hospital support, the options available for skilled care were very limited, so much so it took a week to find a suitable facility with an open bed.
Dad moved to a skilled nursing facility a few miles away from his house. It was the best one his health insurance covered; it included physical therapy, occupational therapy, and open space for him to move around in. He could wear regular clothes and engage with other patients.
After the first few days he was already frustrated with the food, the care, and the situation in general. He wanted to do things on his own, like use the restroom or take a shower, get dressed, etc., but his weakness kept him from accomplishing those tasks without aid, which required waiting for someone to come to his room. Even though we all tried to regularly visit him, he felt lonely. Mom went by to see him every night after work, but still he wanted to go home. On phone calls he often complained about the terrible food and irregular help. He began referring to the facility as ‘the jail’. We tried to balance what he told us about the care with what the nurses and staff reported about his behavior and prognosis. More than once he wheeled himself back to the kitchen to instruct the cook about how to properly prepare a dish; this would then be followed by a phone call, requesting that we bring him something to eat.
Dad lived at the facility until the end of May when his insurance would no longer pay for it, and he was strong ‘enough’ to return home.
By January 2016 my father’s lower right jaw, the same area where the cancer had been, had begun to swell. The bump was sensitive to the touch and we encouraged him to have it looked at by his doctor; he thought it was an abscess. Dad visited an oral surgeon/dentist who took X-rays and determined the bump was not related to his teeth but to a growth on his jawbone. Dad refused to go through the radiation and chemotherapy again, but also was clear that he did not want cancer in his body. The surgeon suggested that they preserve the jaw by scraping the cancer off of it and a date was set for late July.
In early February my parents moved out of the house where they had lived since 1976 and into a cottage for independent living in a retirement community across town. The move was very disruptive, but necessary, as they could no longer maintain their home and live there safely. In early July my mother celebrated the holiday with the family in the Texas hill country. Near the river, she slipped and broke her left femur just above the prosthesis she had received in 2010. Her doctor instructed her to remain immobile for two weeks before he would check it again. We hired someone to spend the day at the house, and to cook, clean, and support them. Insurance did not cover those expenses.
I was teaching the morning of Dad’s operation and could not make it to the hospital until 1 pm. We had been discussing the procedure for weeks and we were confident that it would go as planned. However, as I understood it, on the morning of the surgery, the doctors decided to remove his jaw instead of scraping the cancer off the bone. I did not learn about this change in plans until I arrived at the hospital and spoke with my aunt (Dad’s sister) who had taken him to the hospital, as my mother was bedridden.
After more than six hours of surgery, during which they removed his lower right jaw, rebuilt it with his pectoral muscles, and inserted another PEG tube for him to ‘eat’ through, my father opened his eyes in the recovery room. He had a tracheostomy, so he could only sign to me how he felt with a thumbs-up on his left hand. He then flattened his palm and raised it above his head. We played charades for a while until I understood that he was asking me to take a photo of him and send it to my mother via text. It was his way of telling her he had survived the surgery and he missed her. This is the photo I sent her.
We wondered why the doctors decided to remove his jaw that morning. Had they discussed that change with him in pre-op? My aunt said he had consented to it. But there were so many questions: When? Did anyone explain how long he may have to have the PEG tube? What would the extra burden of eating through the PEG be for him and his family? What would his quality of life be without a jaw? Why didn’t they consider an implant? Most of all, were there alternatives to surgery for an eighty-one-year-old man in his condition? What kind of care would he need in the future and would my mother be able to provide it to him? My angst stemmed from not having adequate answers to these questions; my guilt consumed me for allowing him to navigate those questions alone. But how were we to know?
Four days after his surgery Mom was able to visit Dad in the hospital. I wheeled her up to his room because she was not supposed to be walking yet. Still breathing through the tracheotomy tube, all of his communications were either signed or written on a small white board. He was quite engaged and expressive despite the tube in his throat. He wanted to listen to us: he wrote on his board, ‘I’m fine, tell me about you’. And then he would remember something that needed to be done at home and write it down on the board for us to tend to.
 13. Diptych: After the family meeting with care team, 23 August 2016 (left); Dad waits to be discharged from the hospital, 27 August 2016 (right)
13. Diptych: After the family meeting with care team, 23 August 2016 (left); Dad waits to be discharged from the hospital, 27 August 2016 (right)August was filled with small victories, Dad was taking short steps, buttoning his shirt, combing his hair, and cleaning his mouth out by himself. The occupational and physical therapy teams pushed him and he responded positively, as he really wanted to go home. After listening to all of the teams report on his progress, the idea of his returning home was overwhelming. How on earth would he be able to receive the same level of care? Who would provide it? Who would pay for it? I encouraged my mother and brother to attend the weekly meetings, too, as they needed to participate in the conversation and know what Dad would need. We were the transition team, especially since mom was still in a wheelchair. The continuity of care would require us to maintain a level of engagement we were not expecting, and we worried about how we were going to adequately provide what he needed.
The fall was not easy. Mom and Dad kept the 24/7 care through October, then decreasing the amount of support because of the expense and their desire for privacy. Setting up home health care visits squandered an exceptional amount of time and the turnover of providers was quite frequent (and annoying). Dad’s medications, exercises, and nutrition required a spreadsheet to keep them organized and administered correctly. We got a refresher course on how to ‘feed’ Dad through the PEG and learned how to ‘spot’ him when using the walker. Life had become quite intense for the family, including Dad, as the simplest things were now struggles. New boundaries had been placed on their lives, some of which would become new ‘normals’. One of the most difficult aspects of Dad’s recovery was learning how to swallow again. The speech pathologists worked with him a few times a week, but he had to do his exercises on his own; these were quite painful for him to do, and his enthusiasm waned. He did not improve, prompting one of the therapists to casually remark to him that some patients never learn to swallow again. That incidental comment shook Dad’s confidence in his own recovery, and despite his eventual physical recovery he never did surmount the swallow test.
The first week of June Dad complained of chest pains and thought he had suffered a heart attack. A trip to his primary care physician revealed he had not suffered a myocardial infarction. However, the following week his electrocardiologist’s office called to say his ICD device had been ‘firing’ – a flutter of activity – and they wanted to see him as soon as possible. Mom took Dad in to see the specialist, who decided to immediately admit him to the CICU for observation. They wanted to monitor him closely to figure out what was happening.
In the waiting room, family members discuss Dad’s situation. CICU rules state that only two people can visit a patient in the unit at a time, so we often took turns sitting and waiting while others visited with him. Sometimes after everyone had their visit, we would stay a while longer and discuss next steps, immediate and long term, educating each other on what we had learned, and sharing our support for one another. Other patients’ families were not from the city and often spent their nights in the waiting room as they had no place else to go.
We celebrated Dad’s eighty-fourth birthday in the CICU; his nurses and caregivers brought him balloons, a card, and the neck pillow; his grandchildren, children, and other family visited, testing the limits of how many people could visit a patient at once.
By the middle of the week Dad was transferred to the medium care unit, where they ran tests and made images in preparation for the valve replacement procedure; a surgery date was set for the following week. Friday night the whole family visited Dad in his room. All of his grandchildren and children were there; we talked, laughed, and told him we loved him.
That night Dad’s AFib acted up and his defibrillator went off. He was intubated and returned to the CICU.
Back in the CICU, Dad was placed in an isolation room because he had contracted methicillin-resistant Staphylococcus aureus (MRSA) and had to be separated from other patients. Before entering his room we were asked to put on blue plastic disposable gowns and gloves, and were encouraged to wear a face mask. Teams of physicians rounded more frequently in the CICU but rarely shared their observations with the family; my sister and I engaged each one who saw Dad, inquiring about their strategies for him and his prognosis.
By his third week in the hospital Dad’s family members and the nursing staff had developed strong relationships. This is inevitable when you’re caring so intimately for someone so important to others. We learned a couple of nurses requested to care for Dad, and others would drop by his bed after their shift to check on him. Dad was conscious and alert. Our goal was to have a family member present in the CICU as long as visiting hours allowed (sometimes longer). My sister-in-law arrived each morning at 4 am, my mom took over after she left, and then once we could leave work my brother and I would appear. My sister stayed in town while her husband and boys returned to their home state. Dad’s condition was not improving; he began retaining fluids because of his weak heart, so they used diuretics, but those changed his electrolytes, sending his heart into AFib.
After another defibrillation witnessed by my mother and sister, we realized Dad’s situation had to change. While he wanted to live, his body was not cooperating. A resident electrocardiologist stopped by, and I asked him hypothetically, ‘What is your threshold for knowing when to turn-off an ICD device?’ I mimed placing a magnet just below his left clavicle.
‘I’m confident we can get your father stabilized with these medicines. He’ll be better in a few days more’, he said encouragingly.
‘I’m not asking for him, I’m asking you. When do you know a patient must move from curative to palliative care?’ The resident did not answer me.
I continued, ‘I’ve requested an order for a palliative care evaluation, so we’ll know about his other options’. He looked at me sternly.
Three weeks earlier, when arriving at the hospital, we gave the medical team Dad’s medical power-of-attorney (MPOA)[note 3] and Directive to Physicians documents. Now we were asking about a Do Not Resuscitate (DNR) order from the doctor so if Dad went into another bout of AFib, his ICD would not fire. The clinical ethicist pulled up the documents on his phone and approached Dad’s bed.
‘Mr. Crowder, I want to discuss your advance directives’, he said. Dad looked at him, then he looked at me and the rest of the family standing around, draped in blue, wearing masks. I thought about how unnatural this all had become. We motioned for the resident to join us at the bedside, and I made room for him to stand by me.
The resident clasped his hands to his face and pulled the mask off. ‘I don’t do death’, he stated, as he walked through the curtain and out of the room. I was now at the foot of the hospital bed and found myself explaining to my father his situation. ‘Certainly, he knew all of this already?’, I thought to myself. I had explained it to his sister earlier that day, along with my mother, cousins, and siblings. The questions in my mind continued: ‘How lucid was he? Doesn’t he remember everything that has transpired? Why am I the one doing this?’ We locked eyes and I repeated myself, but now the words meant something completely different. Instead of discussing the medical indications about someone else, I was sharing those observations with the patient himself, who listened like he had never heard those words or considered the alternative to not getting better, because he always had.
At noon that day we met with the hospice nurse and completed the paperwork. The health care team continued to supply Dad with forced air via mask and administered his medications. More family appeared and the room was soon full of cousins and friends; the phone would ring and the voice of someone far away shared with Dad what he meant to her. The afternoon was full of stories and memories, tears and togetherness.
Around 6 pm a team came and removed the colored wristbands from his swollen arms and replaced them with white ones, effectively transferring him from being an CICU patient to one in hospice care. A magnet was placed on his ICD to turn it off; a nurse reached up and turned off the alarms on the bedside monitors. He would no longer receive the heart meds or forced air, but instead morphine and a nasal cannula. Nurses getting off shift dropped by, too, and even the resident returned to see how he was doing. Dad’s oxygen levels remained steady throughout the evening and there was talk about moving him home the next day. Visitors continued to arrive, but by 10:30 pm only the hospice nurse and immediate family remained.
Everyone was exhausted. Before leaving with my sister, my mother wished my father good night and kissed his forehead.
I turned off the bright fluorescent lights and turned up the classical music on the iPod speaker next to the bed. I removed my blue plastic gown and gloves and got comfortable in a chair next to his bed, keeping my head in a position where I could see the monitor on the wall. I continued talking with him to let him know I was there; he responded by nodding his head or vocalizing an ‘ok’. The morphine and other drugs were keeping him comfortable; I was anything but comfortable. I thought about making images. What kind of images would he have been interested in seeing? Both Dad and I used the camera as a means for mediating our worlds, oftentimes placing it between ourselves and others to keep from having to fully engage, a defensive strategy of sorts. However, in this moment, the camera helped me be present with my father. It opened my eyes to things I would have missed had I just been sitting there, waiting, or sleeping. Instead, we had reached the end of his journey together and I documented it with one final panorama of him in his hospital bed, surrounded by machines in a sterile environment. This was not the perfect death. This was not what he would have ever wanted or expected given his access to health insurance, medical care, and family support. How did we get here?
Never once did Dad consider the ethical issues surrounding his care. He trusted his medical team to do what was best for him and I believe they feel that they did. Although he wanted to keep living, he accepted the fact that his heart was giving out and no alternatives were left that would not cause potential undue suffering.
About 1:15 am the monitors indicated drastic swings in Dad’s heart rate. He was now experiencing ventricular fibrillation, and the hospice nurse entered the room, saying ‘I think this might be it’. She left the room and I leaned over the bed to hold him.
Dad passed at 1:32 am.
Acknowledgements
I would like to acknowledge the support and feedback from a number of family members, colleagues, and friends who made this photo essay possible. Of the many family who lived with, cared for, and loved Winston, and consented to being a part of this project, are Julia Crowder, Judson Crowder, Emily Frazelle, Alicia Krouse, David Frazelle, Bon Crowder, and Beth and Jim Barrett. Liz Cartwright’s keen eye and sharp pen helped strengthen the relationship between image and text. Arlene Macdonald, Terry Wright, Peggy Determeyer, and Stephanie Takaragawa also provided thoughtful insight and encouragement throughout this project. A heartfelt thank you to the nurses, doctors, and clinic and hospital staff who cared for Winston throughout his various medical events.
About the author
Jerome Crowder, PhD, is a medical and visual anthropologist who has worked in La Paz, Bolivia; Puno, Perú; and Houston and Galveston, Texas. Currently he is an associate professor at the Institute for Medical Humanities, University of Texas Medical Branch. At UTMB he is the course director for Humanities, Ethics, and Professionalism in the Practice of Medicine course for second-year medical students, and he teaches social medicine and qualitative methods in the Graduate School for Biomedical Sciences. Crowder coedited a special issue of Medical Anthropology called ‘Dissecting Images: Multimodal Medical Anthropology’ and is the coauthor of Visual Research: A Concise Introduction to Thinking Visually (Bloomsbury, 2013).
Suggested readings
Avery, Eric. 1983. ‘Hands Healing: A Photographic Essay’. In The Visual Arts in Medical Education, edited by Geri Berg, 10–25. New York: Southern Illinois University Press.
Curry, Timothy J., and Richard H. Strauss. 1994. ‘A Little Pain Never Hurt Anybody: A Photo-Essay on the Normalization of Sport Injuries’. Sociology of Sport Journal 11 (2): 195–208. https://doi.org/10.1123/ssj.11.2.195.
Goldberg, Morton F. 1986. ‘The Ophthalmic Photo Essay: Inception of a Series’. Archives of Ophthalmology 104 (7): 985–86. https://doi.org/ 10.1001/archopht.1986.0105019004303.
Hao, Xu, and Chen Keji. 2008. ‘Integrative Medicine: The Experience from China’. Journal of Alternative and Complementary Medicine 14 (1): 3–7. https://doi.org/10.1089/acm.2006.6329.
Le Marcis, Frédéric, and Vinh-Kim Nguyen. 2015. ‘An Ebola Photo Essay’. Limn 5. https://limn.it/articles/an-ebola-photo-essay/.
Quinn, Gwendolyn. P., Terrance L. Albrecht, Charles Mahan, Bethany A. Bell-Ellison, Tabia H. Akintobi, Beth Reynolds, and Delores Jeffers. 2006. ‘The Photo Essay: A Visual Research Method for Educating Obstetricians and Other Health Care Professionals’. The Qualitative Report11 (2): 229–50. https://nsuworks.nova.edu/tqr/vol11/iss2/2.
Richards, Eugene. 1989. The Knife and Gun Club: Scenes from an Emergency Room. New York: Atlantic Monthly Press.
Seymour, Tom. 2018. ‘The Photographer Who Instagrammed His Father’s Death’. Wired, 5 June. https://www.wired.co.uk/article/photographer-instagrammed-fathers-death.
Sommer, Annemarie. 2007. ‘Photo Essay: Geroderma Osteodysplastica’. American Journal of Medical Genetics Part C: Seminars in Medical Genetics 145C (3): 291–92. https://doi.org/10.1002/ajmg.c.30146.
Squires, Carol. 2005. The Body at Risk: Photography of Disorder, Illness, and Healing. New York: International Center of Photography and University of California Press, Berkeley.
Endnotes
1 Back
The ICD is a device that combines a pacemaker and defibrillator, placed in the chest or abdomen to monitor and regulate heart rate by controlling the signal across the heart muscle. Modern devices transmit their data over Wi-Fi and alert physicians to irregularities.
2 Back
PET scans help identify metabolic processes in the body, highlighting potential cancers, which glow due to activity.
3 Back
A MPOA document names the patient’s proxy if she is unable to communicate her decisions. My sister, mother, and I were listed for Dad. The Directive to Physicians is a living will, stating the patient’s wishes for end-of-life care, specifically addressing which heroic measures may be taken and under what circumstances. The DNR order is placed in the medical record by the attending physician, thereby communicating to the medical team what should be done, or not done, if the patient would require heroic measures to stay alive.