Everyday adaptability in Ghanaian hospital laboratories
—
Abstract
Implementing global health policy and procedures within countries that are largely underdeveloped and rural is a challenge. Unequal resource availability and distribution can lead to disparities in the care provided to patients. In Ghana, although all health care providers are trained according to national and international standards, discrepancies in laboratory technologies at hospitals in rural and urban areas can impact how health care is provided. While shadowing physicians and laboratory staff within two hospitals, one in a rural area, the Agona-Asamang Seventh-Day Adventist (SDA) hospital, and one in an urban area, the Kumasi South Hospital, I saw health care providers undertaking procedures utilizing differing materials due to the resources available to the hospitals. Notably, the hospitals had identical outcomes.
In circumstances where resources are outdated or lacking, health workers must modify the care they provide while continuing to follow their national health policies as well as the policies recommended by international health organizations (Livingston 2012). In rural Ghana, laboratory technicians modify policies and procedures to provide care that is similar to their urban counterparts. Policies recommended by international health campaigns, such as those from the World Health Organizations (WHO), are implemented when appropriate and possible, depending on the resources available. These rural hospitals strive to provide the care recommended by national health campaigns in Ghana even while they face unfounded criticism from skeptics of advanced medicine. The following photographs depict how technicians apply their deep knowledge of their field to perform laboratory tests in rural areas with limited resources.
 1. Blood grouping and staining, Seventh-day Adventist Hospital-Asamang. Ashanti Region, Ghana, 2018.
1. Blood grouping and staining, Seventh-day Adventist Hospital-Asamang. Ashanti Region, Ghana, 2018.At the Seventh-Day Adventist (SDA) Hospital in Asamang, laboratory technicians, ranging from twenty-two to thirty-five years of age, begin their shift by sanitizing the tools left out from the day before or by completing unfinished tasks. All resources available are utilized each day and then sterilized. In this small missionary hospital laboratory, each station has been reduced to just the essentials. Because of the prevalence of malaria within the region, the miniature staining station to the left, propped up on a piece of foam, is stained purple due to the amount of Giemsa stains performed to visualize the malarial parasite. While the Styrofoam houses the staining materials, a sterile tile is used for cross-matching donor blood.
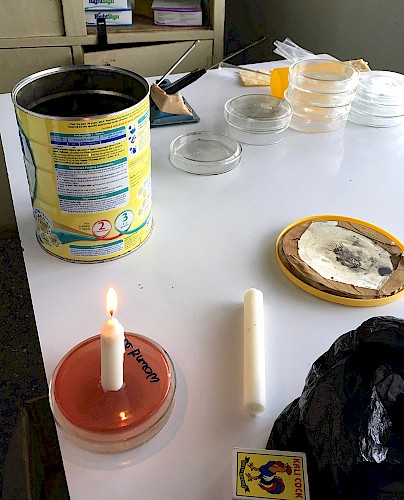
Physicians and laboratory technicians in under-resourced settings like this one face a challenging situation. They need to provide medical care which is current with medical advances while employing only the limited resources available to them. For example, laboratories in developed nations and urban Ghanaian hospitals may use more advanced means to eliminate oxygen, such as the use of a GasPak, which creates an environment devoid of oxygen, thus vital for the diagnosis of anaerobic bacterial infections. In this rural Ghanaian hospital, staff instead seal a can containing a used candle. Image 2 depicts these tools. By enclosing the powdered milk container, covering a cultured agar plate and a candle; the ignited candle will burn the oxygen in the container and extinguish once the anaerobic conditions needed for growth are achieved. These rudimentary laboratory techniques harnessed by the SDA hospital demonstrate the deep understanding of microbiology needed by their technicians, as procedures written by scientists in developed nations must be modified to make use of the resources available.
Laboratory technicians in these areas show great dedication to their jobs. At the SDA’s remote location, forty-five minutes to an hour off the main roads in Kumasi, it is difficult to maintain an adequate supply of agar plates. Knowing this, one of the few microbiologists at this hospital came in during his honeymoon to create blood agar plates from scratch. The agar dishes, while occasionally bought in well-funded hospitals, are prepared in the laboratory within Asamang’s SDA hospital. The laboratory technicians perfect this task by using protein, salts, and agar mixes to create environments suitable for culturing bacteria. These mixes are placed in old glass Pepsi bottles and then autoclaved in a pressure cooker. The molten agar is then poured into plates on the microbiology lab table until each dish contains its allotted amount. This procedure is completed once every week or two, depending on need.
Other obstacles to medical care stem from traditional beliefs about blood donations. One early morning, while waiting for traffic to clear, my professor and our driver read the front page of the local newspaper, which reported a denial by Ghana’s National Blood Service (NBS) that they had provided tainted blood to patients. A prominent evangelist had alleged on social media that in the process of conducting a community outreach event, blood donated by Despite Group of Companies, a Ghanaian media conglomerate, went to ‘spiritual rituals’ instead of transfusions. Damaging accusations such as this can lead to public mistrust of the NBS. These charges were completely false, and were debunked by the NBS in the DailyGuide. Already facing blood shortages around the country, the NBS strives to encourage citizens to donate blood by assuring participants that the donation will be used for medical purposes only.
Per national protocol, potential blood donors must have a sample of their blood tested for viral pathogens, such as HIV. Outside the testing room on one ordinary weekday at the SDA hospital in Asamang, twenty patients are waiting to have their blood sampled for testing. Laboratory technicians receive on-site training in areas of need to ensure that they are able to efficiently complete the work. A recent university graduate (in the white coat), completing her national service in rural Ghana, studies the skill of sampling blood. The technician-in-training and her teacher will spend their entire day drawing samples from fifty to seventy patients who will need various forms of testing for their hospital stay or who wish to donate blood for a relative. The blood is tested for viral pathogens, and individuals are questioned to ascertain if they may have malaria, but they do not receive diagnostic testing for the blood-borne parasite, differing from some WHO recommendations. Clinicians at both hospitals believe that treating the disease based on the presentation of symptoms saves diagnostic tools, as a majority of the population has a built-up immunity to mild infection.
 6. Analyzing a blood smear for malarial parasites, Kumasi South Hospital. Agogo-Kumasi, Ashanti Region, Ghana, 2018.
6. Analyzing a blood smear for malarial parasites, Kumasi South Hospital. Agogo-Kumasi, Ashanti Region, Ghana, 2018.In the government-funded Kumasi South Hospital, a laboratory technician analyzes a patient’s Giemsa-stained blood smear for malarial parasites. This hospital and its laboratory are allocated more resources, funding, and staff due to their larger patient base and governmental ownership. And because of this, a larger population comes in for outpatient care. This technician has five more stains lined up, drying, waiting to be analyzed, and also a waiting room full of restless patients. These patients range from market women who need outpatient care to businessmen being checked into a ward. In both cases, laboratory tests help diagnose medical issues. During the rainy season, the prevalence of malaria rises significantly, leading to an increased use of microscopy screenings and rapid diagnostic tests to ensure a correct diagnosis. The greater availability of resources in the urban hospitals enables them to treat a large number of patients with more supplies, while rural hospitals must tend to more than one hundred patients a day with their minimal resources.
Conclusion
These photographs highlight the various ways care and laboratory techniques are managed in rural and urban Ghana where common procedures need to be modified based on resource availability. Patients receive suitable treatment and the techniques harnessed are found to be acceptable in both settings. Still, in rural Ghana, technicians must use their own know-how to modify procedures to meet standards. These technicians employ decades-old protocols to meticulously complete tedious tasks necessary to ensure the health and safety of their patients.
About the author
Ian Lichtenstein is a recent graduate from the University of New Hampshire who majored in biomedical sciences with a specialization in microbiology. This photo essay is an extension of his senior thesis, which focused on the transmission of malaria via blood transfusions in rural and urban Ghanaian hospitals.
References
De Cock, Kevin M., Joseph L. Barker, Rachel Baggaley, and Wafaa M. El Sadr. 2019. ‘Where Are the Positives? HIV Testing in sub‐Saharan Africa in the Era of Test and Treat’. AIDS 33: 349–52.
Livingston, Julie. 2012. Improvising Medicine. Durham, NC: Duke University Press.