Promises and perils of guan
Mental healthcare and the rise of biopolitical paternalism in contemporary China
—
Abstract
Configuring the family in Chinese psychiatry
If we spend any time in a psychiatric hospital in China, we will likely be struck by the fact that most of the inpatients have been hospitalised against or regardless of their will, usually by their family members. According to a conservative estimate made in the early 2000s (Pan, Xie, and Zheng 2003), involuntary admission of inpatients by families accounted for 60 percent of all psychiatric inpatients, and involuntary admission by police or other public-sector agents accounted for another 20 percent. In China, although families have long been involved in the care of mentally ill patients, [1] the ways in which they are involved have varied over time. It is only with recent market reforms (starting in the 1980s) that families have gradually come to occupy the role of key agent in securing biomedical and institutional treatment for patients. Over the past decade, human rights activists in China have launched a vehement attack on the prevalence of involuntary hospitalisation and on families’ involvement in it. Despite such contingencies and challenges, the Mental Health Law (effective since May 2013), China’s first-ever national legislation regarding the mentally ill, has reinforced the rights and responsibilities of families in patient care and management. Under the law, psychiatric patients are automatically subjected to the guardianship of their family members, listed in the order of spouses, parents, adult children, and other close relatives. While the law stipulates that psychiatric hospitalisation should be voluntary in principle, it also allows family members to hospitalise patients who are at risk of harming themselves or others. [2] Meanwhile, the law charges families with the responsibility to provide for, look after, and rehabilitate patients, whether they were involuntarily hospitalised and/or considered ‘at risk’ or not (National People’s Congress 2012).
Why does the family occupy such a critical role in psychiatric care in China, especially today? This is the central question of my project. While existing studies tend to see the involvement of Chinese families in their relatives’ mental healthcare as an ahistorical, self-contained phenomenon (Lin and Lin 1980; Tseng and Wu 2013), the contingencies and controversies outlined above suggest that they are technological, institutional, and ideological configurations constantly undergoing change. [3] Note that ‘configure’ here means both to represent by an image and to fashion or put together in a certain form; how technological, institutional, and ideological forces represent the family in turn shapes how they interact with and regulate it. By examining the configuration of families in mental health, this article provides a fuller understanding of the effects, ethics, and political economies of medical care and population governance in contemporary China.
Data for this article comes from 32 months of fieldwork I conducted between 2008 and 2014 in a variety of settings actively engaged in serving, monitoring, or challenging family involvement in psychiatric care. They included psychiatric hospitals, community mental health teams, community social work centres, family support groups, and human rights agencies, mostly in Guangdong Province but also across China. My interviews explored how the staff, patients, and family members at these settings conceptualised the role of family, including its rights and responsibilities. I observed how individual people occupied such roles and conveyed their role expectations to each other in interactions, justifying their actions accordingly. Moreover, in order to explore representations of the family in historical and contemporary debates related to Chinese psychiatry, I interviewed lawmakers, attended national conferences, and collected relevant archival and media materials.
Across these sites, I focused on the patient population diagnosed with serious mental illnesses. In the Chinese context, the term ‘serious mental illness’ [ zhongxing jingshen jibing ] is an administrative category covering schizophrenia, bipolar disorder, schizoaffective disorder, paranoid disorder, epilepsy with psychosis, and intellectual disability with psychosis (Ministry of Health 2012), though most of the patients I encountered were diagnosed with either schizophrenia or bipolar disorder. Official statistics estimated that, as of 2011, there were more than 16 million people with serious mental illnesses in China (Xinhua News Agency 2011).
From the fieldnotes, interview transcripts, and historical and contemporary documents collected, I extracted significant themes of mental illness, care, and family involvement. I then traced the convergence and divergence of their meanings and use across different realms. Doing so allowed me to ‘follow the metaphor’ (Marcus 1998) (or construct) of the family across the mental health landscape and discover configuration in action.
Guan and the rise of biopolitical paternalism
A prominent configuration of the family in relation to the seriously mentally ill patient is that of 管 [ guan ] . Guan is written as one Chinese character. In Chinese, a single character often constitutes a word in and of itself. Most single-character words are polysemic; that is, a word has two or more somewhat related meanings, and only the context in which it is uttered can specify its meaning-in-use. Single characters can also be combined with others to make less ambiguous compound words. Therefore, depending on the context and the word combination, guan can refer to what English speakers might think of as the state of concerning oneself with and being responsible for another individual, even caring about or for someone; it can also refer to the act of managing or governing, and carry connotations of intervention and control. In this article, whenever I invoke guan, I will provide my own translation.
Here is an example that illustrates the everyday practice of guan and its intricacies: One day in the autumn of 2013, I accompanied Mrs. Dong, a woman in her late fifties, on a visit to see her daughter Tingting, who was in a locked psychiatric ward in Nanhua. [4] Two months earlier, when Tingting had become distraught and insomniac due to chaotic experiences at work and in her romantic relationship, Mrs. Dong had taken her to the hospital, telling her that the visit would just be for a brief check-up. However, once there, Tingting was diagnosed with bipolar disorder, admitted to the inpatient ward, and was kept there. Now that Tingting’s condition had stabilized through prescribed medication, Mrs. Dong felt the need to plan for Tingting’s life following discharge. As Mrs. Dong saw it, Tingting’s workplace had proven too stressful an environment. In fact, any job that required Tingting to work ‘outside’ on her own would probably expose her to undue stress or unhealthy romantic relationships. It would also make it impossible for Mrs. Dong to monitor her medications. Therefore, without Tingting’s knowledge, Mrs. Dong had sent a resignation letter to Tingting’s company and had bought a small storefront near their home, expecting the two of them to run a herbal tea stall together. On the ward, Mrs. Dong presented her plan to Tingting with a big smile on her face, saying, ‘From now on, life will be more relaxing for you.’
‘No!’ Tingting screamed, ‘I’m 30 years old! Why didn’t you look after [ guan ] me when I was a kid rather than control [ guan ] me now, when I should be enjoying freedom?’ Tingting then explained to me that, throughout her childhood, her mother had worked far away from home while her father had spent his time playing cards with friends.
‘We were indeed at fault,’ Mrs. Dong apologised softly, ‘so let me make it up to you now, OK?’
Tingting shook her head. ‘Before I was sent here, I had been sorting out my work and my moods. I only needed some more time. You threw me in here and that totally messed me up. Please, leave me alone!’
‘You’re sick,’ sighed Mrs. Dong, ‘how can I not care for [ guan ] you?’
Here, the same actions—the mother hospitalising the daughter against her will, planning her future, protecting her from potential harm, and ensuring her medical compliance—seemed like control to the daughter and care to the mother. Yet the same Chinese character they used, guan, allowed them to simultaneously acknowledge, refute, and reframe each other’s perspective. We can thus see that the polysemy of guan allows for struggles as to its practical meanings, ethical orientations, and relational implications.
Guan is not only invoked in everyday family strife. As will be shown later, psychiatrists also use the language of guan as they teach family members to monitor patients’ symptoms and pharmaceutical compliance. Moreover, recent laws and policies have highlighted guan as a principle of mental health work, but they articulate guan specifically as management [ guanli ] on the basis that those with serious mental illnesses constitute risks to themselves and others (Ministry of Health 2012). These regulations also define families as the agent of patient management. For instance, while the Mental Health Law opens by requiring ‘all facets of society’ to participate in guan , or the comprehensive management of mentally ill patients (Article 6), it quickly relegates almost all of this responsibility to the patients’ families. Article 21 of the law states, ‘If it appears that a family member may have a mental disorder, other family members shall help them obtain prompt medical care, provide for their daily needs, and assume responsibility for their supervision [ kanhu ] and management [ guanli ]’ (National People’s Congress 2012).
Anthropologist Jianfeng Zhu and colleagues have identified a culture of guan in China’s mental health services, which they suggest tends to ‘objectify and infantilise its subjects’ and turn families of seriously mentally ill patients into agents of power (Zhu et al. 2018). In this article, I will further trace the circulation of guan between family practices, psychiatric encounters, and legal or policy reforms. Taking its polysemy seriously, I explore how people define, evaluate, and contest guan in different realms; how practices and meanings of guan are transformed when psychiatric and legal discourses come to emphasise but also reconfigure the family’s role as its site and agent; and the power effects of these processes on various actors and relations.
Guan is useful to think with, not only because it permeates mental healthcare in China (and for that matter, many other aspects of contemporary Chinese life) but also because it helps us think through the relationship between care and biopower. As Michel Foucault famously argued, modern nation-states have developed in tandem with the rise of biopower—that is, the set of knowledges, experts, and institutions that bring ‘life and its mechanisms into the realm of explicit [political] calculations’ (Foucault 1978, 143). In particular, he used the term ‘biopolitics’ to refer to the ways in which the population is treated as a political problem (Foucault 2009). Chinese psychiatry is a mechanism of biopolitics, for it brings mental illness, especially the various risks it poses to the patient or others (Castel 1991; Rose 2010), into the calculations of how to regulate the population. Building on the growing anthropological literature of how families are entangled in biopower (e.g., Biehl 2005; Povinelli 2006), this study further explores how the family is shaped by the biopolitics of mental health and mediates its operation.
Additionally, the workings of psychiatry hinge upon the ethics of care; in seeking treatment for the patient, family members assume responsibilities for vulnerable others and explore visions of the good life (Mol, Moser, and Pols 2010). The literature on care has shed light on the lived moral experiences and strivings of varied populations in the face of suffering (e.g., Kleinman 2009; Mattingly 2014; and Stevenson 2014), as well as the conditions of possibility and impossibility for care (Biehl 2005; Scheper-Hughes 1993). However, some of this literature tends to idealise care, treating it as transparent, harmless, and spontaneously springing from loving family feelings. My research looks at guan , a locally specific practice of intimate relation—a care-like relation, if you will—that has political import. It illustrates how biopower requires and transforms intimate practices of care, as well as assumptions of personhood, interpersonal desires, and power dynamics in the provision of care.
As we saw in Tingting’s case, guan , at least for those who perform or promote it, means caring for the vulnerable other by intervening in and making decisions for their life, because ‘mother (or father, or psychiatrist, or the state) knows best’. Therefore, examining the enactment and circulation of guan can provide insights into the ethics and politics of paternalism. In the literature of medical ethics, paternalism is defined as ‘the interference with a person’s liberty of action justified by reasons referring exclusively to the welfare . . . of the person being coerced’ (Dworkin 1972). Grounded in the tradition of liberal individualism, this literature ignores how the very definition of the individual subject is shaped by different sociopolitical conditions and different imaginations of the social order. In China, the individual is typically not seen as absolutely independent, but rather as produced by and woven into layers of social fabrics. For instance, Confucianism saw the father as endowing his son with essences of life and order, with the expectation that the son would reciprocate with filial piety; this father–son relationship then formed the basis of the ruler–subject relationship (Hsu 1971). Building on this Confucian paternalism, the Maoist regime fashioned itself as an overarching ‘parent state’ by organising its working-class people into work units and communes, arranging their lives and distributing resources accordingly, and encouraging their direct parental identification with Mao (Steinmüller 2015).
In the market reform era that started in the 1980s, socialist institutions (such as work units and communes) and accompanying public welfare systems have largely been eroded. Still, the state often invokes the idea of paternalism to present itself as caring and legitimise its governance. We have to ask to what extent the state actually upholds the legacy of paternalism and who actually assumes the responsibility of being ‘paternal’. Also, as dreams of scientific modernity loom large in post-Mao China, how do scientific discourses—including the psychological and psychiatric discourses that the state increasingly promotes (Huang 2014; Yang 2015; and Zhang 2017)—re-constitute both the target and the agent of paternalistic practices? Moreover, if the notion of paternalism implies an omniscient and omnipotent authority, what does it look like to practise paternalistic governance in everyday life, especially if the practising agent is not so powerful? By tracking the circulation of guan in different realms and paying attention to its power effects, we can address these questions and understand how paternalism as a historical ideology and an everyday ethic is enacted.
I argue that in contemporary China, a guan- style biopolitical paternalism has emerged. It sees in mentally ill patients the chronic risk of illness relapse and violent behaviour, and asserts that these risks necessitate perpetual management. The cultural ethics and ideological legacies that approve paternalism help legitimise the state’s control over the population; meanwhile, through the circulation of paternalistic values from the state to the medical professional and then to the family, the actual responsibilities of care and control end up falling to families, particularly female and elderly caregivers. This biopolitical paternalism then produces relatively novel desires, vulnerabilities, and harms within families. To demonstrate my argument, below I will consider the cultural ethics of guan as an idealised practice of parenting and socialisation. I will then move on to analyse how this default meaning of guan is mobilised and moulded by Chinese psychiatric discourse and the state’s practices of mental health management. Next, I will discuss the power effects of this reconfiguration for both patients and their family members. I will conclude this article by considering the conceptual and practical implications of biopolitical paternalism.
From hopeful parenting to chronic risk management
Despite its polysemy, guan has a common established meaning for many Chinese speakers: the ethical practice of parenting. As cultural psychologists and anthropologists have told us, when Chinese parents practice guan with their children, their seemingly stern behaviour—characterised by control, discipline, and restraint—is often accompanied by care, love, and sacrificial labour (Fong 2004; Xu 2017). Underlying these practices is the idea that children are ‘weak, vulnerable, and dependent beings’ (Saari 1990) who have to be protected and trained in an optimal environment by their more mature and knowledgeable parents. Parents engage in guan with the hope that their children can become fully human [ chengren ] and capable of acting in harmony with the social order (Chao 1994), at which point they will no longer need guan . Because this guan seamlessly links individual development, parental aspiration, and social order together, scholars have argued that guan is ‘the characteristic feature of Chinese socialisation’ (Wu 1996).
This idea of guan as synonymous with Chinese practices of parenting was shared by Tingting and Mrs. Dong, except that Tingting saw herself as an adult no longer bound by guan , whereas Mrs. Dong saw her as a vulnerable and childlike being still in dire need of it. Indeed, guan in parenting finds many parallels with popular approaches to guan for the mentally ill. Chinese people I have interviewed say that they commonly experience mental illness as a radical breakdown of the orderly world. This disorderly experience incites their desire for treatment [ zhi ] and management [ guan ], both of which signify a quest for proper order. In particular, because mental illness is seen as a force that renders patients extremely vulnerable, even returning adults to a childlike and fragile state, family members—including those who are not parents, like spouses and siblings—often feel it necessary to take all matters of the patient’s life into their own hands. Like Mrs. Dong, they take great pains to build a ‘stress-free’ environment for the related patient, to restrict the patient’s potentially harmful behaviour, and retrain them in matters of emotional management, social skills, and pharmaceutical compliance. Such practices of guan entail much sacrificial labour, especially on the part of female caregivers such as mothers, sisters, and wives. When Tingting was receiving treatment on the ward, Mrs. Dong spent a lot of time running around the city to check every livelihood option for Tingting, and she tirelessly brought her home-cooked meals every day. These efforts, Mrs. Dong hoped, would make Tingting become a happy and healthy human again.
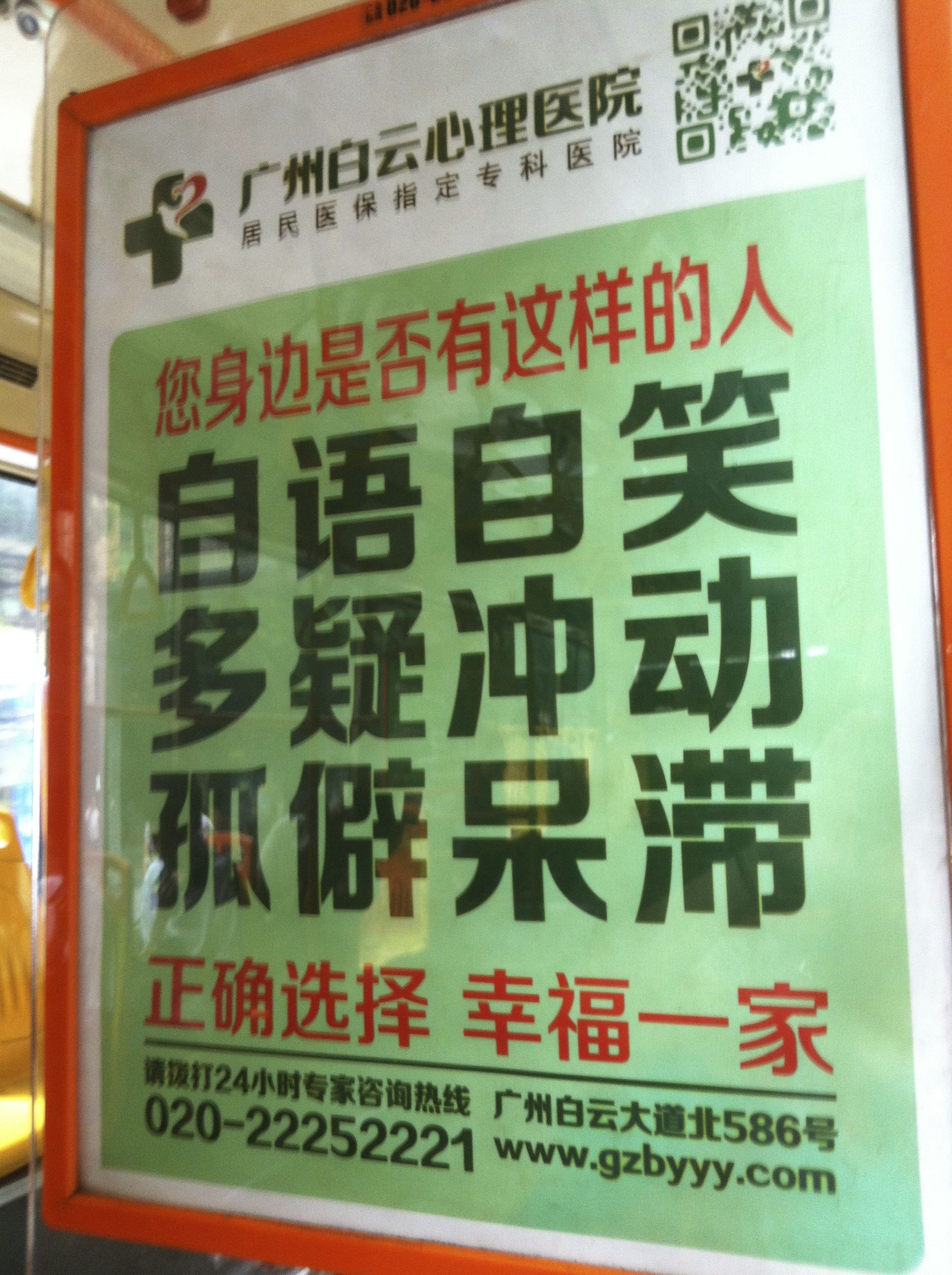 1. Bus poster advertisement for a psychiatric hospital.
[5]
Photo by Zhiying Ma
(2013).
1. Bus poster advertisement for a psychiatric hospital.
[5]
Photo by Zhiying Ma
(2013).
When Mrs. Dong first sent Tingting to the hospital, her doctor friend there promised her that medications would soon calm her daughter down. After two weeks of treatment with psychotropics, Tingting’s symptoms did subside. However, the doctor told Mrs. Dong not to celebrate too soon; he pointed to Tingting’s occasional sleeplessness and expressions of frustration as signs of illness fluctuation, indicating a risk of relapse. Because of this apparently high risk of relapse, he said, Tingting would have to keep taking the medications after discharge for anywhere from two years to the rest of her life. He also admonished Mrs. Dong to closely monitor [ guan ] Tingting’s pharmaceutical compliance and symptoms, even when Tingting’s condition seemed stable. At the same time, however, the doctor rejected other practices of guan suggested by Mrs. Dong. For example, when Mrs. Dong told the doctor her concern that the antipsychotics were making Tingting overweight, self-conscious, and worried again about the prospect of finding love, he chastised her for micromanaging or engaging too much in guan [ guan taiduo ] , and for interfering in his treatment plan.
From this case, we can see how hospital psychiatry reconfigures intimate practices of guan into a form of biomedical risk management. While families seek help from psychiatry motivated by the desire for a quick cure, psychiatry replies by inscribing patients into a chronic trajectory of remission, risk, and relapse. Because patients are seen to lack insight—that is, they do not know that they are mentally ill and need medical help—psychiatrists often recruit and teach family members to guan them. Note that as people have diverse perspectives on the nature of a given disorder, the types of guan they practice are also diverse. For instance, influenced by traditional Chinese medicine, many family members accept mental illness as a result of qi [vital energy] stagnation caused by the bodymind’s temporarily disturbed relationship with its milieu, instead of (or in addition to) the psychiatric explanation of a neurochemical disorder. They thus use techniques ranging from herbal medicine to diet regimen to adjustments of family relationships to help bring order back to patients’ lives and to ameliorate the disturbances that psychopharmaceuticals incur in patients (Ma 2012). Yet, as shown in the comments of Tingting’s doctor, the only appropriate guan from the medical point of view is to manage patients’ risk of relapse and deterioration. As such, family members should mobilise their authority to ensure patients’ compliance with psychopharmaceuticals; use their intimate knowledge of and attentiveness to the patient to detect possible signs of relapse; and, if signs of relapse or deterioration do occur, use family funds to re-hospitalise the patient. Since mentally ill patients’ illness trajectories are often projected by psychiatrists to be chronic, family members’ responsibilities of guan, in the form of biomedical risk management, also become chronic.
The healthcare structure in which guan operates is a relatively recent market formation. Compared to today, the socialist era preceding the early 1980s saw more agents involved in the care of mentally ill patients. Those agents included not just families, but also work units, neighbourhood committees, the police, local governments, and so on. Additionally, the services provided were much more diverse and community-based (Kao 1979). However, since the market reform, the community healthcare system in China has basically collapsed, and the public health insurance system has also been severely disrupted. Granted, the state has not completely withdrawn from healthcare provision, but its spending has been concentrated on building hospital infrastructures, especially large secondary- or tertiary-care hospital centres. These hospitals run on a fee-for-service model. In the field of psychiatry, the rise of big hospitals has been accompanied by the dominance of a biomedical and pharmaceutical approach to mental health (Phillips 1998). Therefore, despite harbouring diverse perspectives, many families gradually come to see hospitalisation and pharmaceuticals as the most legitimate and desirable forms of care for people with mental illnesses. Because of the rollback of the welfare state, families are not only the main agents in hospitalising patients, but are also the main payers of expensive hospital bills (Pearson 1995). When patients are discharged, family members are often left as the sole carers—they alone have to look after and provide for their relatives, as, across China, work units, communes, and other forms of collective life have been destroyed or restructured. In recent years, the state has been rebuilding its public health insurance system, but the system works mostly for people already in the workforce (Blumenthal and Hsiao 2005). Meanwhile, unemployed psychiatric patients often have difficulty signing up for the meagre insurance available, which, in any case, often only covers inpatient stays. As a result, the mentally ill patient is constantly shuttled between the psychiatric hospital—typically a locked ward—and the home, with no end in sight. I call this structure of mental healthcare in the market reform era a ‘hospital–family circuit’ (Ma 2014).
When psychiatrists tell family members to manage patients and monitor risks, it is implied that this risk management will lower the chances of patient relapse and rehospitalisation. However, in the hospital–family circuit, family members’ heightened awareness of risks and their desire to guan —as reconfigured by psychiatry—sometimes lead to lowered thresholds for involuntary hospitalisation. In the hospitals I visited, more than half of the total patients had been repeatedly hospitalised by their families. Some complained to me that while the first hospitalisation had been appropriate given their chaotic feelings or behaviours, subsequent commitments had been based on increasingly minor issues, such as their refusal to take medications that had heavy side effects or emotional reactions that were understandable given the circumstances. Without listening to their explanations, their family members—often with the help of hospital staff—forcibly or deceptively brought them back to the hospital. One patient expressed her frustration as follows:
I feel I am being suffocated by all the guan from my sister. Whenever I lift a finger, she’ll say I have relapsed and send me back in here. I am just a puppet on a string, being pulled here and there by others. I am not able to resist the littlest bit.
Mental health policies and the security state
If hospital psychiatry in the reform era has reconfigured familial guan into intimate practices that manage patients’ biomedical risk of relapse and deterioration, then the Chinese state’s recent mental health policies have further redefined guan as bound intrinsically to security concerns and social management, highlighting another kind of risk. In the market reform era, as Michael Dutton (2005) pointed out, the enshrinement of working-class people by the Maoist state has given way to the idea that the Chinese population is something that first and foremost needs to be managed. Particularly since the late 1990s and early 2000s, with the rise of socioeconomic inequality and popular unrest, the state has been increasingly keen on maintaining social stability [ weiwen ] through managing everything from public violence to political dissent as security threats (Cho 2013; Lee and Zhang 2013). The 686 Program, a nationwide community mental health program established by the Ministry of Health in 2004, capitalises on this focus on security. While the program ambitiously claims to fill the large gap of care between the hospital and patients’ homes, so far it has only targeted people diagnosed with serious mental illnesses. In fact, the scope of serious mental illness was by and large defined by community mental health policies. These disorders—schizophrenia, bipolar disorder, schizoaffective disorder, paranoid disorder, epilepsy with psychosis, and intellectual disability with psychosis—almost all have a clear psychotic component, and all are presumed by the program’s policies to make patients prone to violence (e.g., Ministry of Health 2012). [6]
Funded by the security state, the 686 Program has trained cadres of community mental health practitioners to manage [ guanli ] seriously mentally ill patients in the community. [7] My fieldwork, undertaken alongside some of these practitioners, shows that they are increasingly held accountable for incidents of violence committed by patients in their jurisdiction, and that they have learned to pass on this pressure to manage patients to the families themselves. Community mental health practitioners regularly visit patients’ homes to collect information on their symptoms and pharmaceutical compliance and assess the risk of violence. They do so not by talking with patients themselves, but by talking with their family members. The program has a humanitarian component—that is, it provides access to basic psychopharmaceuticals for impoverished patients. Yet community practitioners often dispense the medications into the hands of the patients’ family members so that they can supervise medication intake at home. The program’s official discourse celebrates open therapeutic alliances between patients and caregivers, and it denounces covert or coercive practices such as hidden pharmaceutical treatment (e.g., the mixing of pills into patients’ meals). In practice, however, community practitioners often acquiesce to such practices by families, and sometimes even teach the families how to secretly medicate so that patients’ symptoms and the risk of violence can be better kept in check. Finally, home visits by community mental health practitioners often end with reminders to family members regarding the patient’s riskiness and the family’s responsibility to watch over [ guan ] them. Therefore, in this emerging community mental health apparatus, patients with serious mental illnesses are further constituted as risks to public security and the social order. Correspondingly, guan is further reconfigured as security risk management. The responsibility for such management is passed down through layers of government to community mental health practitioners and, ultimately, to the patients’ families.
More recent processes of mental health legislation show us how the reconfiguration and relegation of guan have been legitimised. In the mid-2000s, after discovering cases in which families or local governments subjected healthy individuals to psychiatric hospitalisation for ulterior interests, human rights activists vehemently criticised the extensive use of involuntary hospitalisation in China for its infringement of people’s personal autonomy (Wu 2016). In response, the psychiatrists drafting the Mental Health Law justified this practice as a manifestation of ‘state paternalism’ [ guojia fuquan ]: literally the power of the state to act as a father. Implicitly invoking socialist legacies, they argued that psychiatric abuse was rare and that state paternalism had protected China from experiencing the disastrous consequences that deinstitutionalisation and an overemphasis on individual freedom had produced for both patients’ wellbeing and the public order in Western societies (Xie and Ma 2011). This logic might sound appealing, especially to the Chinese public, which had benefited from the socialist state’s care and protection in the past and which was anxious to have them continued in the future (Chen and Yang 2012). However, the narrative these psychiatrists used to justify involuntary hospitalisation was incomplete; in reality, the neoliberal state did not shoulder the concrete paternalistic responsibilities of guan . Instead, these framers of the Mental Health Law would go on to invoke the notion of guan as a cultural ideal of kinship practice that could relegate responsibility for paternal care to families. One psychiatrist told me, ‘Fortunately, while American families can simply walk away, Chinese families will always guan their patients.’
Prior to the Mental Health Law, families could hospitalise any member they deemed to be mentally ill as a form of ‘medical protection’ (Shao et al. 2010). As a compromise with human rights campaigners, the Mental Health Law stipulates that admission to a psychiatric hospital should be voluntary in principle, except when patients are at risk of harming themselves or others. Human rights activists and many patients were initially hopeful that this new principle would result in an expansion of patient rights and freedoms. Meanwhile, many family caregivers found the new law’s emphasis on risks vague—indeed, the law does not define what counts as a risk, and it elides the many forms of vulnerability families experience when dealing with patients. In the cases I observed, a patient might have mood swings and frequently curse his parents; they might squander the family’s savings; or they might simply wander off from home. While these behaviours deeply concerned the families, they did not necessarily qualify the patients for (involuntary) hospitalisation. Therefore, in order to secure treatment for such patients, caregivers now have to tactically mobilise the law’s language of risk, emphasising the potentially grave consequences of such errant behaviours, sometimes even fabricating narratives of a given patient’s danger to the general public. Out of their biomedicalised sense of compassion and professional responsibilities, psychiatrists, community mental health practitioners, and other government agents often ‘collude’ with caregivers in this process of strategic assessment (Fan and Wang 2015). According to my observations and several reports from psychiatrists at different hospitals, after the initial few months of adjustment following the Mental Health Law, involuntary hospitalisation again became the practical norm for hospital psychiatry. The only change that the law brought about seems to be that it has solidified the reconfiguration of guan as risk management in the minds of both family members and professionals.
Guan as everyday family practice: Vulnerability, indifference, and unease
When the psychiatrists who drafted the Mental Health Law used the ideas of state paternalism and guan to legitimise involuntary hospitalisation and other types of coercive care, they portrayed both the state and the figure of familial guardian as an omniscient, omnipotent, and ideologically masculine authority. This authority figure presumably always knows what’s best for his subjects, always succeeds in achieving its benevolent aims, and will never harm or be harmed. Echoing the popular Chinese saying of ‘strict father, compassionate mother’, this authority figure also fulfils the cultural imagination of fatherhood by endowing his subject with the essence of life and disciplining them according to normative principles of personhood. Granted, the mother also figures in the popular imaginary of familial guan , but she only adds an element of tender love and does not disrupt the absolute power difference or the disciplinary goal implied in paternalism. However, what happens when this paternalistic ideal is practised in everyday life by family members?
First of all, because of the adult onset of many mental illnesses, the family members who engage in guan of patients usually do not wield much power. Many of them are ageing parents or female relatives who, due to their low-income jobs, are chosen to stay at home and look after familial patients. These vulnerable family members often lack the authority and even the physical strength to coerce good behaviour from their charges, so ‘how should I guan ?’ is a question that preoccupies them every day. For example, in order to get the patients to take their meds, the family caregivers I encountered often engage in trivial yet painful negotiations with the patients in their care. They either dole out ‘bribes’ such as soft drinks or cigarettes, mix the ground pills into meals while fearing discovery, or take the pills themselves in front of the patients in order to prove that the pills are not poisonous. These ‘soft’ tactics they devise for the hard task of guan are still met by their patients with silent aversion, outright resistance, or sometimes even physical resistance. These reactions in turn can deeply upset caregivers, who see the patients as misunderstanding and rejecting their most loving intentions. Such a lack of appreciation could seem especially unfair given that there are often other family members who wash their hands of guan . Tingting’s father, for example, spent his time playing mahjong and avoided all responsibility for her unhappiness. Still, emotional heartaches and physical exhaustion are nothing compared to caregivers’ fears of a precarious future. Because many adult patients don’t have spouses, children, or siblings, and because they are usually unemployed and receive little in the way of welfare subsidy, often it is their ageing parents who need to ‘manage’ them and use their meagre retirement pensions to provide for them. Therefore, across the country, there is a widespread phenomenon perceived as ‘the old raising the disabled’ [ lao yang can ]. These ageing parents repeatedly ask this question to themselves, me, and every professional and bureaucrat they encounter: ‘When I become too old or pass away, who will guan [caringly manage] my child?’
Instead of reducing vulnerability in a patient population, guan reconfigured as biomedical and security risk management sometimes increases the vulnerability of those diagnosed as mentally ill. I have already mentioned how a heightened awareness of risks, inculcated by contemporary Chinese psychiatry, has led some family members to more quickly consider re-hospitalising the patients in their care, and how this in turn has imposed upon patients a sense of suffocation. As Ian Hacking (1999) points out, how we categorise certain people influences how we interact with them and how they perform themselves, producing the ‘looping effects’ that ‘make up people’. In this case, when patients’ lives are disrupted by endless hospitalisations, restrictions, and familial strife, many of them do end up confirming the gloomy psychiatric prognosis, which predicts that two-thirds of all patients with serious mental illnesses will be at least partially disabled throughout their lives. If guan as an idealised kinship practice is hinged on the production of hope—that is, the prospect that the subject of guan will become fully human again and not need to be subject to guan anymore—then what happens when guan in psychiatric practice systematically dashes such hope?
When hope becomes elusive, and especially when a patient’s vulnerabilities make family ties more fragile, caregivers feel uncertain about whether and how to take responsibility. [8] In many of the psychiatric hospitals I visited, scores of patients had been left there for years, or even for the rest of their lives, by their family members. One such long-term patient, Xu Wei, [9] became the plaintiff of the first and most sensational lawsuit under the new Mental Health Law. In May 2013, Xu filed suit against the hospital and his guardian, asking to be discharged. Diagnosed with schizophrenia, Wei had been kept in a rundown hospital in Shanghai since 2003. He desperately wanted to be released in order to start a family with the girlfriend he had met at the hospital. Everyone, including doctors at the hospital, agreed that Wei was stable and could function well outside the institution. Yet his elder brother, who was his guardian but who lived in a faraway city, refused to let him out, citing the petty fight between Xu Wei and their father that had resulted in his long-term commitment to the hospital. The brother said, ‘I’m his guardian! I have to watch over [ guan ] him. I have to be responsible to society!’ Wei suspected that his brother had ulterior motives, such as an unwillingness to share their now-deceased father’s estate. In any case, the judge was initially sympathetic to Wei. He sent court officials to ask Wei’s distant relatives and members of his neighbourhood committee whether they would like to be his guardian instead so they could endorse Wei’s discharge. Nobody would.
In April 2015, Xu Wei lost the case. The court’s verdict stated that, as a patient with schizophrenia, Wei had limited legal capacity and should be constantly managed [ guan ] with regard to his medications and everyday life. His guardian had both the responsibility and the right to arrange for such management. Given the family’s circumstances, the verdict said, hospitalisation was an appropriate mode of management [ guan ] and thus the guardian (Wei’s brother) had fulfilled his responsibility by placing him there. [10] Xu and those of his supporters I talked to found this decision ironic, because the problem was exactly that nobody wanted to guan Xu Wei: to concern themselves with his happiness and wellbeing.
Here we have a paradox of guan , one conditioned by biopolitical paternalism. On the one hand, medical and administrative discourses constitute patients with serious mental illnesses as chronic biomedical and security risks, and then relegate the entire responsibility for risk management to the patients’ families. So long as the risks are under control, where the patients are placed and how they are managed become a matter of legal and ethical indifference. In her recent ethnographic study of how the Canadian state handles tuberculosis and suicide epidemics among the Inuit, Lisa Stevenson (2014) discusses an anonymous kind of state care: a biopolitical indifference. This describes a state ideology that implicitly posits that so long as the physical lives of Inuit people are maintained, it does not matter who it is that lives or dies, or how the life in question is lived. This biopolitical indifference is also found in psychiatric care in China, except that rather than being performed mainly by the state, it is mediated by families. On the other hand, since guan reconfigured as risk management also invokes idealised kinship practices, biopolitical indifference in psychiatric care in China generates affective and ethical unease for people who receive or perceive it. After all, as a cultural ideal, guan hinges upon intimate affects and kin relations, requires the caregiver to pay attention to the vulnerable person’s concrete circumstances, and aims to make a difference in lives. As such, for Xu Wei and those who supported him, guan as an indifferent form of risk management betrays the spirit of hope and the play of difference also inherent in the concept.
This indifference should not be blamed solely on the families that make the decision to restrict or hospitalise a related patient, but also on the broader security state apparatus, which quietly but actively seeks to maintain long-term hospitalisation in cases like Xu Wei’s. In 2014, at a conference in Beijing, I spoke with a psychiatrist who was an appointed mental health expert of the Ministry of Health. Because a few long-term inpatients had requested my help to get them out of the hospital, I asked the psychiatrist whether it might be possible for them to live outside together in a rental apartment, with regular visits from social workers—a dream of those inpatients. ‘No way,’ he responded firmly. ‘The government is concerned with protecting society rather than protecting the patient. If nothing bad happens with such group homes, that’s fine. But if anything goes wrong, who carries the liability?’ Frustrated, I asked him what one should/could do for those inmates, or for people like Xu Wei. ‘You can’t openly help them,’ he said. ‘You might do something under the table. But I’m telling you, the law [regarding discharge] won’t be loosened up.’
Conclusion
In this article, I have traced the circulation, reconfiguration, and transformation of guan through familial, psychiatric, and legal-administrative realms. I have shown the emergence of what I call ‘biopolitical paternalism’ in mental healthcare in contemporary China. This biopolitical paternalism creates a certain kind of biological subject in the patient and a need for its regulation. In particular, the psychiatric, administrative, and legal discourses of Chinese mental health constitute mentally ill patients as subjects posing permanent biomedical risks to themselves and security risks to the public. The subjects constituted as such require constant management so that a healthy citizenry and good public order can be produced and maintained. In this process, the cultural ethics of guan as an idealised kinship practice, coupled with the historical ideology of paternalism, allow the state to co-opt and build upon its socialist legacy and fashion itself as a caring parent state, despite the fact that the practice of guan has now been reconfigured as biomedical and biopolitical risk management. Meanwhile, the flexible circulation of guan enables the state to displace management responsibilities to the families of patients. As for power effects, the biopolitical paternalism articulated by guan produces intimate vulnerabilities and ethical unease in caregivers, patients, and observers, as well as new political potentials. While the agent of paternalism is imagined to be an omniscient, omnipotent, and ideologically masculine authority, in reality it is often vulnerable family members, such as women and elderly parents, who must do the managing. The responsibility for chronic risk management strains caregivers’ relationships with patients, making both sides even more vulnerable. In particular, the chronicity and indifference implied in this form of risk management generate deep ethical unease. Meanwhile (and as I explore in depth elsewhere), in response to the tensions between the ideological legitimation and structural displacement of biopolitical paternalism, some family caregivers I interviewed have begun to ‘flip the script’ (Carr 2010) by demanding that the state take the responsibilities of guan and act as a proper parent, thereby fulfilling the unmet promise of paternity. They ask the state to recognise both their own vulnerability and the vulnerability of patients, and heal the injuries wrought by marketisation. As such, they reframe guan to build what I call ‘paternalistic citizenship’ (Ma 2020).
Mental healthcare in contemporary China is only a special case foregrounding a more general biopolitical paternalism. Because of its striking use of coercion/constraint and the often-clear presence of the state, psychiatry allows ‘the larger social “will” (to power, to social order) [to] show its teeth’ (Lovell and Rhodes 2014). Yet some other mechanisms of governance in contemporary China also share the conditions of biopolitical paternalism: the reconfiguration of ‘the people’ into a ‘population’ that needs to be managed; the neoliberal devolution of welfare and healthcare; and the rise of the security state. For example, the famous one-child policy made married couples responsible for producing not only fewer children, but also children thought to be of better ‘quality’, to save the nation-state from a ‘population crisis’ (Anagnost 1995; Greenhalgh 2008). As the state increasingly expands its social management, other non-familial relations, such as neighbours and schoolteachers, are pulled in to perform guan as well. Throughout the world, as biomedicalised techniques of rule continue to redefine individual wellbeing and population security, and as neoliberal economic policies continue to transfer the responsibilities to enact these new ideals away from the state, scholars have noticed the use of paternalistic strategies in diverse projects of social governance, from poverty alleviation to health promotion. These projects draw on everyday relations and techniques of direction, instruction, and surveillance to produce individual subjects who are either self-governed or well managed (Soss, Fording, and Schram 2011; Shever 2013). These formations of power are of course not equivalent, but, as an analytical concept, ‘biopolitical paternalism’ may illuminate the processes by which, in different relations and governance mechanisms, subjects are constituted and regulated and responsibilities for discipline are legitimised and distributed in social space. It may also allow us to better detect the power effects of such regulations, especially in the context of intimate relations.
An analysis of biopolitical paternalism and its intimate workings can also contribute to our understanding of chronic shortfalls in the provision of healthcare. During the mental health legislation debate in China, whenever critics raised concerns with the pervasiveness of involuntary hospitalisation and its potential abuse, leading psychiatrists would argue that, rather than having too much institutionalisation, China didn’t have enough. This statement is in one sense true. As of 2011, Chinese hospitals averaged only one psychiatric bed per 100,000 patients, which was said to be just slightly better than low- and lower-middle-income countries (0.6 and 0.4 respectively), but which fell far behind upper-middle-income countries (2.7), a group to which China as an economic entity belongs, and high-income countries (13.6) (World Health Organization 2011a, b). However, it was not until after the Mental Health Law was passed that those psychiatrists have begun to admit another, less convenient, fact: hospitalised patients in China are usually hospitalised for much longer, and with far higher readmission rates, than patients of economically comparable countries. [11] While no national statistics have been published yet, local reports have been slowly emerging. In 2013, the director of Anding Hospital in Beijing reported that out of the 800 inpatients of the hospital, over 100 of them were long-term patients; the longest stay had been 25 years. In a survey done by the staff at another psychiatric hospital in Beijing, 180 inpatients out of the total 300 wanted to go home, and, of those, 150 were considered to be in stable condition (Zhang 2013).
Therefore, the answer is not simply to take sides and stake out territory alongside one of these two phenomena (fewer hospital beds on the one hand, longer hospitalisation and higher readmission rates on the other); rather, we should see these two phenomena as emerging from a common landscape of inadequate mental healthcare, and should understand how this landscape is shaped by the political economy as well as intimate anxieties generated by the course of psychiatric care in its present form. As I have pointed out, in the hospital–family circuit, many families with means pull together their own funds or welfare resources to put patients in hospital, only to end up trapped in the chronic trajectory of risk management punctuated by endless cycles of hospitalisation. Meanwhile, families that don’t have the means for hospital care receive little by way of professional services or relief. In order to address this disparity, we must ask, if there are not enough mental health services in China, what kind of services would be more effective in providing genuine care? Proposals for new services, without due consideration, run the risk of duplicating the existing psychiatric institutions that operate on and instil the logic of chronic risk management and rely on familial resources and popular triage to function. The question is, how can we build mental health services that are human-centred and community-based and that allow the state and other social actors to participate in—and share responsibilities for—care?
On 27 September 2017, after 15 years of hospitalisation, Xu Wei was finally released. In July of that year, the Centre for Forensic Science of the Ministry of Justice issued a statement certifying Mr. Xu’s ‘full legal capacity’, which meant that he could make decisions for himself. While celebrating his hard-won freedom, the activists who had been supporting him were hesitant to claim this as a victory. After all, they argued, legal capacity should be inherent in every human being; the fact that it was evaluated and granted by forensic psychiatrists only reinforced the tyranny of the medical authority. Moreover, at the same time as Xu’s release, some major cities issued new policies to bring long-term hospitalisation to patients whose families could not care for them as an explicit attempt to ‘reduce risks to social control’ [ guankong ]. Therefore, instead of an end to long-term hospitalisation, we may be witnessing a slow and quiet change in the formation of biopolitical paternalism: when families fail, the increasingly wealthy state may now be more willing to step up and more fully assume the role of the parent, directly securing the biopolitical order and deciding the fate of all its children.
Acknowledgements
The initial writing of this article was supported by the Doctoral Fellowship of the Chiang Ching-kuo Foundation for International Scholarly Exchange. Comments on drafts were generously provided by Judith Farquhar, Eugene Raikhel, Susan Gal, Don Kulick, members of the Michigan Society of Fellows, and colleagues and friends who have heard the job-talk versions of this paper. I also thank the anonymous reviewers and the editorial team of Medicine Anthropology Theory for their helpful remarks.
About the author
Zhiying Ma is an assistant professor at the School of Social Service Administration, University of Chicago. Trained in cultural and medical anthropology, her work in general concerns how cultural, politico-economic, and technological factors shape the design and implementation of social policies, and how national policies and global development initiatives in turn impact health in/equity, vulnerability, and rights. Her current projects examine family and community care for people diagnosed with serious mental illnesses, as well as the lives and rights of persons with disabilities (both in China). She is also involved in community-based participatory research and advocacy projects with these groups.
Footnotes
-
Note that when I use the word ‘patient’, I am following the customs of the field and paying attention to the social experiences that come with this label; I do not mean to endorse psychiatric knowledge/practice in general or its diagnoses or treatments of specific persons. ↩︎
-
According to the Mental Health Law, when the patient is at risk of harming others, the police may also decide on hospitalisation, but family members may contest that decision. ↩︎
-
Similarly, Emily Baum (2018) has argued that in early 20th-century Beijing, madness was not a stable, ahistorical entity, but rather constantly ‘invented’ by different actors in a way that was shaped by the particular social conditions at that time. ↩︎
-
Nanhua is a pseudonym, as are the names of most persons and organisations mentioned. In China, psychiatric hospitals and other mental health service organisations are few and far between, making them easily identifiable. To protect the privacy of my interlocutors, I choose to anonymise not only the organisations with which they are associated, but also the host cities of the organisations. ↩︎
-
The author translates the poster as follows: Is there someone like this around you? / Someone who talks and laughs to himself? / Someone who is suspicious and impulsive? / Someone who is aloof or dull? / Make the right choice. / Make your whole family happy. ↩︎
-
Tellingly, the 686 Program does not include depression as a targeted illness. As the program’s leaders told me, this is partly because people with depression typically only harm themselves, not others, which is less of a concern to the security state (Ma 2020). ↩︎
-
In policy documents, the full title given to these practitioners is ‘community doctors for preventing and treating mental illness’. They are general practitioners and nurses assigned to work on community mental health. In the layered and geographically diverse administrative structures of China, other agents may also be deployed to work on mental health, including officials on neighborhood committees, police officers, and social workers. The work of these other agents is not bound to the same extent by the 686 Program, and the complexity of their interactions requires further ethnographic investigation. ↩︎
-
Similarly, Sarah Pinto argues that, in India, psychiatric care often mediates the dissolution of kinship bonds and conjugal love. As such, it ‘adds vulnerability to the already—and inherently—vulnerable condition of kinship’ (Pinto 2014, 30). ↩︎
-
This is a pseudonym of the plaintiff that has been universally used by his attorney, other activists, and journalists. ↩︎
-
The verdict further stated that, although Article 44 of the Mental Health Law granted voluntary inpatients the right to voluntary discharge, Xu had been involuntarily hospitalised because of his risk to others and thus could not enjoy this right. Activists have criticised this provision, or rather the court’s interpretation of it, for depriving people of their freedom indefinitely for what is often a one-time act. Some have demanded a legal procedure to be introduced that allows involuntarily hospitalised patients to transition to voluntary hospitalisation, thereby becoming eligible for voluntary discharge. ↩︎
-
Speaking at the 2015 conference of the Society for Psychological Anthropology, held in Boston, MA, Dr. Yu Xin, then director of the Peking University Institute of Mental Health, pointed to ‘longer hospitalisation and higher readmission rate’ as leading problems in China’s mental health system. ↩︎
References
Anagnost, Ann. 1995. ‘A Surfeit of Bodies: Population and the Rationality of the State in Post-Mao China’. Ginsburg, Faye, and Rayna Rapp, eds. Conceiving the New World Order: The Global Politics of Reproduction . Berkeley, CA: University of California Press.
Baum, Emily. 2018. The Invention of Madness: State, Society, and the Insane in Modern China. Chicago, IL: University of Chicago Press. https://doi.org/10.7208/chicago/9780226580753.001.0001.
Biehl, João. 2005. Vita: Life in a Zone of Social Abandonment. Berkeley, CA: University of California Press.
Blumenthal, David, and William Hsiao. 2005. ‘Privatization and Its Discontents: The Evolving Chinese Health Care System’. New England Journal of Medicine 353 (11): 1165–1170.
Carr, E. Summerson. 2010. Scripting Addiction: The Politics of Therapeutic Talk and American Sobriety. Princeton, NJ: Princeton University Press. https://doi.org/10.1515/9781400836659.
Castel, Robert. 1991. ‘From Dangerousness to Risk’. Burchell, Graham, Colin Gordon, and Peter Miller, eds. The Foucault Effect: Studies in Governmentality. Chicago, IL: University of Chicago Press. https://doi.org/10.7208/chicago/9780226028811.001.0001.
Chao, Ruth K. 1994. ‘Beyond Parental Control and Authoritarian Parenting Style: Understanding Chinese Parenting through the Cultural Notion of Training’. Child Development 65 (4): 1111–1119.
Chen, Lijun, and Dali L. Yang. 2012. ‘Old Age Care Concerns and State–Society Relations in China: Public Anxiety and State Paternalism’. Journal of Asian Public Policy 5 (2): 136–154.
Cho, Mun Young. 2013. The Specter of ‘The People’: Urban Poverty in Northeast China. Ithaca, NY: Cornell University Press.
Dutton, Michael. 2005. Policing Chinese Politics: A History. Durham, NC: Duke University Press. https://doi.org/10.1215/9780822397625.
Dworkin, Gerald. 1972. ‘Paternalism’. The Monist 56 (1): 64–84. https://doi.org/10.5840/monist197256119.
Fan, Ruiping, and Mingxu Wang. 2015. ‘Taking the Role of the Family Seriously in Treating Chinese Psychiatric Patients: A Confucian Familist Review of China’s First Mental Health Act’. Journal of Medicine and Philosophy 40 (4): 387–399.
Fong, Vanessa L. 2004. Only Hope: Coming of Age under China’s One-Child Policy. Palo Alto, CA: Stanford University Press.
Foucault, Michel. 1978. The History of Sexuality, Volume I: The Will to Knowledge. 1st American ed. New York: Pantheon Books.
Foucault, Michel. 2009. Security, Territory, Population: Lectures at the Collège de France 1977–1978. Burchell, Graham, trans. New York: Picador.
Greenhalgh, Susan. 2008. Just One Child: Science and Policy in Deng’s China. Berkeley, CA: University of California Press.
Hacking, Ian. 1999. ‘Madness: Biological or Constructed?’ In The Social Construction of What? Hacking, Ian, ed. Cambridge, MA: Harvard University Press.
Hsu, Francis L. K. 1971. Under the Ancestor’s Shadow. Palo Alto, CA: Stanford University Press.
Huang, Hsuan-Ying. 2014. ‘The Emergence of the Psycho-Boom in Contemporary Urban China’. Chiang, Howard, ed. Psychiatry and Chinese History. London: Pickering & Chatto. https://doi.org/10.4324/9781315654379.
Kao, John J. 1979. Three Millennia of Chinese Psychiatry. New York: Institute for Advanced Research in Asian Science and Medicine.
Kleinman, Arthur. 2009. ‘Caregiving: The Odyssey of Becoming More Human’. The Lancet 373 (9660): 292–293. https://doi.org/10.1016/S0140-6736(09)60087-8.
Lee, Ching Kwan, and Yonghong Zhang. 2013. ‘The Power of Instability: Unraveling the Microfoundations of Bargained Authoritarianism in China’. American Journal of Sociology 118 (6): 1475–1508.
Lin, Tsung-Yi, and Mei-Chen Lin. 1980. ‘Love, Denial and Rejection: Responses of Chinese Families to Mental Illnesses’. Kleinman, Arthur, and Tsung-Yi Lin, eds. Normal and Abnormal Behavior in Chinese Culture. Boston, MA: Kluwer. https://doi.org/10.1007/978-94-017-4986-2_20.
Lovell, Anne M., and Lorna A. Rhodes. 2014. ‘Psychiatry with Teeth: Notes on Coercion and Control in France and the United States’. Culture, Medicine, and Psychiatry 38 (4): 618–622. https://doi.org/10.1007/s11013-014-9420-9.
Ma, Zhiying. 2012. ‘Psychiatric Subjectivity and Cultural Resistance: Experience and Explanations of Schizophrenia in Contemporary China.’ Kipnis, Andrew, ed. Chinese Modernity and the Individual Psyche . New York: Palgrave MacMillan. https://doi.org/10.1057/9781137268969.0016.
Ma, Zhiying. 2014. ‘Qinmi de Shengming Zhengzhi—Jiating Quanze Zhuti yu Jingshen Weisheng Lifa’ [Intimate Politics of Life: The Family Subject and Mental Health Legislation]. Sixiang Zhanxian [The Ideological Front] 40 (3): 42–49.
Ma, Zhiying. 2020. ‘Numbers and the Assembling of a Community Mental Health Infrastructure in Post-Socialist China’. Greenhalgh, Susan, and Li Zhang, eds. Can Science and Technology Save China? Ithaca, NY: Cornell University Press. https://doi.org/10.7591/9781501747045.
Ma, Zhiying. 2020. ‘Waiting for the Parent State: Suffering, Sociality, and Citizenship among Family Caregivers of People with Serious Mental Illnesses in China’. Unpublished.
Marcus, George. 1998. Ethnography through Thick and Thin. Princeton, NJ: Princeton University Press.
Mattingly, Cheryl. 2014. Moral Laboratories: Family Peril and the Struggle for a Good Life. Berkeley, CA: University of California Press. https://doi.org/10.1525/california/9780520281196.001.0001.
Ministry of Health, the People’s Republic of China. 2012. Zhongxing Jingshen Jibing Guanli Zhiliao Gongzuo Guifan [Rules for Management and Treatment of Serious Mental Illnesses].
Mol, Annemarie, Ingunn Moser, and A. J. Pols. 2010. Care in Practice: On Tinkering in Clinics, Homes and Farms . Bielefeld, Germany: Transcript Verlag. https://doi.org/10.14361/transcript.9783839414477.
National People’s Congress, the People’s Republic of China. 2012. Zhonghua Renmin Gongheguo Jingshen Weisheng Fa [Mental Health Law of the People’s Republic of China]. Beijing: Falv Chubanshe [Law Press China].
Pan, Zhongde, Bin Xie, and Zhanpei Zheng. 2003. ‘Woguo Jingshen Zhang’ai Zhe de Ruyuan Fangshi Diaocha’ [A Survey on Psychiatric Hospital Admission and Related Factors in China]. Linchuang Jingshen Yixue Zazhi [Journal of Clinical Psychological Medicine] 13 (5): 270–274.
Pearson, Veronica. 1995. Mental Health Care in China: State Policies, Professional Services and Family Responsibilities. London: Gaskell.
Phillips, Michael. 1998. ‘The Transformation of China’s Mental Health Services’. The China Journal 39 (1): 1–36. https://doi.org/10.2307/2667691.
Pinto, Sarah. 2014. Daughters of Parvati: Women and Madness in Contemporary India. Philadelphia, PA: University of Pennsylvania Press. https://doi.org/10.9783/9780812209280.
Povinelli, Elizabeth. 2006. The Empire of Love: Toward a Theory of Intimacy, Genealogy, and Carnality. Durham, NC: Duke University Press. https://doi.org/10.1215/9780822388487.
Rose, Nikolas. 2010. ‘“Screen and Intervene”: Governing Risky Brains’. History of the Human Sciences 23: 79–105.
Saari, Jon L. 1990. Legacies of Childhood: Growing up Chinese in a Time of Crisis, 1890–1920. Cambridge, MA: Harvard University Asia Center. https://doi.org/10.2307/j.ctt1tg5mpf.
Scheper-Hughes, Nancy. 1993. Death Without Weeping: The Violence of Everyday Life in Brazil. Berkeley, CA: University of California Press.
Shao, Yang, Bin Xie, Mary-Jo Good, and Byron Good. 2010. ‘Current Legislation on Admission of Mentally Ill Patients in China’. International Journal of Law and Psychiatry 33 (1): 52–57. https://doi.org/10.1016/j.ijlp.2009.10.001.
Shever, Elana. 2013. ‘“I Am a Petroleum Product”: Making Kinship Work on the Patagonian Frontier’. McKinnon, Susan, and Fenella Cannell, eds. Vital Relations: Modernity and the Persistent Life of Kinship. Santa Fe: School for Advanced Research Press.
Soss, Joe, Richard C. Fording, and Sanford F. Schram. 2011. Disciplining the Poor: Neoliberal Paternalism and the Persistent Power of Race. Chicago, IL: University of Chicago Press. https://doi.org/10.7208/chicago/9780226768786.001.0001.
Steinmüller, Hans. 2015. ‘“Father Mao” and the Country-Family: Mixed Feelings for Fathers, Officials, and Leaders in China’. Social Analysis 59 (4): 83–100. https://doi.org/10.3167/sa.2015.590406.
Stevenson, Lisa. 2014. Life Beside Itself: Imagining Care in the Canadian Arctic. Berkeley, CA: University of California Press.
Tseng, Wen-Shing, and David Y. H. Wu. 2013. Chinese Culture and Mental Health . Orlando, FL: Academic Press.
World Health Organization. 2011a. Mental Health Atlas 2011 . Geneva, Switzerland.
World Health Organization. 2011b. Mental Health Atlas 2011—China . Geneva, Swizerland.
Wu, David Y. H. 1996. ‘Parental Control: Psychocultural Interpretations of Chinese Patterns of Socialization’. Lau, Sing, ed. Growing up the Chinese Way: Chinese Child and Adolescent Development. Hong Kong: the Chinese University Press.
Wu, Harry Yi-Jui. 2016. ‘The Moral Career of “Outmates”: Towards a History of Manufactured Mental Disorders in Post-Socialist China’. Medical History 60 (1): 87–104.
Xie, Bin, and Hong Ma. 2011. ‘Youguan Jingshen Weisheng Fa de Liuge Misi’ [Six Myths Concerning the Mental Health Law]. Ma Hong’s Blog . https://mahong2006.blog.hexun.com/65403321_d.html.
Xinhua News Agency. 2011. ‘Weisheng Bu Buzhang: Woguo You Yanzhong Jingshen Zhang’ai Huanzhe 1600 Wan Ren’ [Director of Ministry of Health: 16 Million Patients with Severe Mental Disorders in China]. https://politics.people.com.cn/GB/1027/15996111.html.
Xu, Jing. 2017. The Good Child: Moral Development in a Chinese Preschool. Palo Alto, CA: Stanford University Press.
Yang, Jie. 2015. Unknotting the Heart: Unemployment and Therapeutic Governance in China. Ithaca, NY: Cornell University Press. http://doi.org/10.7591/9780801456183.
Zhang, Li. 2017. ‘The Rise of Therapeutic Governing in Postsocialist China’. Medical Anthropology 36 (1): 6–18. https://dx.doi.org/10.1080/01459740.2015.1117079.
Zhang, Ran. 2013. ‘Jingshen Weisheng Fa Xiayue Shishi, Jingshen Zhang’ai Fangzhi Duoge Wenti Daijie’ [Mental Health Law to Be Implemented Next Month, Many Problems to Be Solved for the Prevention and Treatment of Mental Disorders]. Jinghua Shibao [Jinghua Times], 18 April 2013. https://News.Ifeng.Com/Mainland/Detail_2013_04/18/24337106_0.Shtml.
Zhu, Jianfeng, Tianshu Pan, Hai Yu, And Dong Dong. 2018. ‘ Guan (Care/Control): An Ethnographic Understanding of Care for People with Severe Mental Illness from Shanghai’s Urban Communities’. Culture, Medicine and Psychiatry 42: 92–111. https://doi.org/10.1007/S11013-017-9543-X.
