Within the last decade, challenges of diagnosis have emerged on the global health agenda, accompanied by an expansion in the use of point-of-care and rapid detection devices in low-resource contexts where laboratory facilities are scarce. Few studies have explored how these changes are shaping people’s diagnostic journeys and their modes of accessing such technologies. In this paper I show how sick people and their families in a peri-urban area in Burkina Faso attempt to access diagnostic technologies and make themselves visible to the healthcare system through papers. In this context, I show how referral papers and diagnostic papers take on significance for people as they attempt to access care and diagnostic technologies and ‘carry’ knowledge between different levels of the healthcare system. The use of papers is often an uncertain undertaking, as they remain unintelligible to the sick and the layperson. I highlight how the form of the papers makes a crucial difference to the ways that sick people are able to use them. Papers and diagnostic technologies present both opportunities and challenges, and simultaneously engender hope, uncertainty, disappointment, and despair for the sick seeking a cure. Uncertainties, especially financial ones, arise with the possibility of new referrals and diagnostic tests, and along the way many give up or are immobilised when faced with diagnostic ambiguity.
(In)Visible Disease
Motions and Emotions Engendered by Papers and Diagnostics of People Accessing Healthcare in Burkina Faso
—
Abstract
Introduction
In early February 2020 we sit on plastic chairs in the shade of the tree in Caroline’s[1] household courtyard and discuss how she is doing now and what has happened since we saw her last. When we visited Caroline at the end of November 2019, she had just been discharged from the hospital where she had been treated for dengue fever.
‘Why did you choose to do the test for dengue fever?’ I ask her, knowing that it had cost her 10.000 CFA[2] francs (around 18 US dollars), a significant amount of money for Caroline and her husband.
‘Today, they no longer treat patients at random. If you go to the hospital sick, you need to do tests to find out what disease you have. This is why the doctors told us to go for the tests and return to them, so that they will see what disease I suffer from. We should first test to see what disease it is, before we do the treatment,’ she replies.
Caroline’s emphasis, efforts, and emotions involved in making her ailment and herself visible to the public healthcare system in Burkina Faso make up the empirical backbone of this research article. Caroline employed various health documents or papers and actively sought out different diagnostic technologies within the public healthcare system. The ethnographic material for this article was gathered at a time of heightened global focus on diagnostic testing before treatment in low-income countries, as a way, for example, to limit the spread of antibiotic resistance (Chandler and Dixon 2019). For many years, large-scale funding programmes for the diagnostic testing, monitoring, and medication of infectious diseases such as HIV, tuberculosis, and malaria have dominated the global health agenda. Much less attention in this respect has been given to non-communicable conditions such as diabetes, hypertension, and cancer, for which no such large-scale programmes exist. In relation to flows of global funding, Ruth Prince shows how certain groups of people have higher ‘social visibility and political traction while others faded into the background’ (Prince 2019, 135). Within the last decade, diagnostic concerns have emerged on the global health agenda, receiving levels of attention similar to those given to access to essential medicines in the early years of this millennium. As a result, the use of innovative and inexpensive point-of-care and rapid detection devices, capable of being used in settings with no functioning laboratory facilities, has gained momentum in resource-poor settings (Street et al. 2014; Street 2018; Ansumana et al. 2020). Such diagnostic instruments have to a large degree become the means by which disease is made visible at policy, practitioner, and population level. As, on the individual and population level, pharmaceuticals in many different settings represent ‘good care’ (Whyte, van der Geest, and Hardon 2002; Haenssgen et al. 2018), so diagnostic technologies, as an ‘increasingly high-tech form of pharmaceuticalised care’ as termed by Chandler and Dixon (2019, 70), have come to signify good care.
In this article I explore how sick people like Caroline, and their families, attempt to become visible to the public healthcare system in Burkina Faso. In doing so, I delve into the papers that these people employ when interacting with the healthcare system, and I show the motions and emotions that these ‘technologies of visibility’ (in contrast to Biehl’s (2005) notion of ‘technologies of invisibility’) engender in them. In some instances, papers are the means by which access to other technologies of visibility, i.e., diagnostic technologies, can be obtained. In others, they contain knowledge that the sick person is responsible for carrying between the different levels of healthcare. Lastly, I show how such technologies of visibility simultaneously evoke uncertainty, hope, disappointment, and despair in the sick.
Medical (in)visibility, (in)visible work, and access to healthcare
In the social sciences, the clinic or the hospital has been a classic site in which to study visibility and knowledge. Here, the biological body is opened up to the expert biomedical gaze and diseases are made visible and knowable (Foucault 2012). However, in recent years, hospital ethnography in the global south has demonstrated how fragmented and under-resourced healthcare systems struggle to diagnose disease (Wendland 2010; Livingston 2012, 2020; Street 2011). The institutional and intellectual architectures of these healthcare systems have largely been designed to handle diseases separately; yet, diseases often appear as co-infections or co-morbidity (Livingston 2020).
Social science scholars are increasingly drawing attention to how, in the global south, patients’ diagnostic journeys to, for example, tuberculosis and diabetes diagnoses, often involve diagnostic detours and lost money and time (Liggins 2020; Yellapa et al. 2017). Less attention has been given to the ‘work’ patients do, or are expected to do, to access diagnostic services and arrive at a diagnosis (Yellapa et al. 2017). This work is often invisible to policymakers and those not performing the work, moving scholars to call for a rigorous analysis of the dynamic interplay of visible and invisible work (Yellapa et al. 2017; Oudshoorn 2008; Star and Strauss 1999). Alice Street employs the concept of ‘visibility work’ to highlight how, for example, patients in a public hospital in Papua New Guinea actively try to render their bodies visible and knowable to the clinical gaze and to construct productive relationships with other people, for example health staff and family members (Street 2014). In this context, patients and healthcare professionals grapple with invisibility and diseased bodies that ‘rarely crystalize into clear biomedical objects’ (Street 2014, 12) because technology is unreliable, lacking, or not working. Street reverses the classic Foucauldian analysis of visibility, knowledge, power, and control, and highlights the agentic dimension of being seen when she writes that ‘not only is there a form of seeing, but also a form of being seen’ (2014, 26). Patients in Papua New Guinea actively employ their health booklet and other health documents to become visible to, and elicit a response from, the healthcare system (Street 2012). Similarly, other scholars have drawn attention to how, in low-resource contexts, public and non-governmental medical care and social services are provided through a range of documentary and bureaucratic practices demanded by transnational funding agencies who, to a large degree, rely on quantitative approaches to evaluating services (McKay 2012, 2018; Cogburn 2020). While such documentary and bureaucratic practices enable possibilities for care and knowledge, they also exclude patients and users who for various reasons are not able to present these documents (McKay 2012, 2018; Cogburn 2020). Writing about land conflicts in the valley of Autlán in Jalisco, Mexico, Monique Nuijten describes how documents and maps acquire special and magical meaning for the people involved. She calls this paperwork a ‘hope-generating machine’ because it creates great expectations; however, many promises are never fulfilled (2004, 211).
Andrea Brighenti emphasises the style and mode of access to places of visibility. One is not just invisible when one cannot access places of visibility; the mode of accessing such places is also largely or completely out of one’s control (2007). It is precisely the mode or way in which sick people and their family members access diagnostic technologies, care, and treatment in the public healthcare system in Burkina Faso that I explore here. I contribute to the literature on visibility and access to healthcare in low-resource contexts by spelling out the concurrent opportunities and challenges, as well as the emotions that visibility technologies engender—emotions that incline people to engage with them but which also make many give up along the way. By doing so, I shed light on the more subtle exclusions of healthcare.
Health priorities and diagnostics in Burkina Faso
Public health services in Burkina Faso are provided under the principle of user fees. However, user-fee exemptions have long existed for tuberculosis, HIV, and malnutrition, and since 2006 there has been a subsidy policy for births and newborns under seven days of age (Ridde and Yaméogo 2018). Furthermore, in 2016 the country initiated a free healthcare policy for children under five and pregnant women, with basic services such as free diagnostics, treatment, and care for malaria available free of charge (Ouédraogo et al. 2020; Ridde and Yaméogo 2018).
For many years, malaria has been Burkina Faso’s main health priority, funded and supported by the President’s Malaria Initiative, the Global Fund to Fight AIDS, the Bill & Melinda Gates Foundation, the World Health Organisation (WHO), and the Malaria Consortium. Because of the country’s limited laboratory facilities and diagnostic capacity, all febrile illnesses have largely been treated presumptively, as malaria was in the past. Helle Samuelsen shows how the country’s monthly health reports, with their overwhelming focus on malaria, function as a ‘technology of invisibility’ (Biehl 2005) whereby other diseases are rendered invisible because symptoms of fever are automatically registered as malaria (Samuelsen 2020). In accordance with the WHO’s recommendation to confirm malaria infection prior to treatment, national policies today recommend the confirmation of malaria by either microscopy or rapid diagnostic tests (RDTs) before treatment. Microscopy tests are available in the country’s nine district hospitals and four university hospitals only. As a result, in 2016 the availability of RDTs for malaria was expanded throughout the country (Bonko et al. 2019; Ridde et al. 2014; President’s Malaria Initiative 2019).
However, the screen and test strategy for malaria has created a dilemma for non-malarial infections in terms of how to diagnose and manage them (Bonko et al. 2019; Chandler and Dixon 2019). Antibiotics are systematically prescribed when malaria infection is excluded, and in cases of a confirmed malaria diagnosis there is a tendency to prescribe antibiotics alongside antimalarial drugs (Bonko et al. 2019). However, the ability to confirm malaria infections has brought attention to other, non-malarial fevers in Burkina Faso. Dengue fever has (re)surfaced—several outbreaks have been recorded in recent times (in 2013, 2016, and 2017)—and is thus becoming more and more visible to policymakers, healthcare workers, and the population as a whole (Zongo et al. 2018). After the 2016 outbreak, the country set up laboratory facilities to detect dengue fever in Ouagadougou and Bobo-Dioulasso, the two largest cities in the country (Rasmussen and Sahay 2017). In addition, today RDTs for dengue fever are sporadically available in some public health facilities and private clinics across the country.
The entry level to public healthcare in Burkina Faso is the dispensary, known as Centre de santé et de promotion sociale (CSPS) in French. In some places, however, a medical centre, Centre Médical (CM), constitutes the first level of care. In general, equipment in these facilities is limited to that needed to perform basic examinations, such as thermometers, scales, and blood-pressure machines, as well as RDTs for malaria and at times for dengue fever. A nurse heads up the dispensary while a physician heads up the medical centre, and when the medical centre also contains a laboratory, a technician is employed. The second entry point at the district level are the district hospitals, called Centres Médicaux Avec Antenne Chirurgicale (CMAs) in French. Compared with the dispensaries and medical centres, these district hospitals are better equipped in terms of staffing, facilities, and equipment, and have laboratories and a surgical department. Here, it is possible to perform blood glucose tests and certain other laboratory tests. However, the units are not equipped to carry out diagnostic confirmations and patient follow-ups. The country’s nine regional hospitals, Centres Hospitaliers Régionaux (CHRs), together with its single national hospital and four university hospitals, Centres Hospitaliers Universitaires (CHU), constitute the highest specialised care available. At all levels of the public healthcare system there are problems pertaining to human resources, broken equipment, and out-of-stock diagnostics including RTDs and the reagents used in laboratory testing.
Various non-governmental and associated organisations conduct screenings for HIV, hypertension, diabetes, sickle cell anaemia, and breast, cervix, and prostate cancer. However, these activities are uncoordinated and erratic, and rarely happen in entry-level establishments (Ministère de la Santé du Burkina Faso 2016). Insulin and cancer medications are available only from private pharmacies and private hospital pharmacies, and some are not available in the country at all (Klatman, McKee, and Ogle 2019; Ministère de la Santé du Burkina Faso 2016). Treatment of certain types of cancer is referred to specialised hospitals in the neighbouring country of Ghana. Currently, four centres for specialised care are under construction: a centre for cancer, a centre for neurosurgery, a centre for physical rehabilitation, and a centre for traditional medicine and integrated care (INSP 2020).
The study
Ethnographic material was gathered during four months of fieldwork in Burkina Faso, between September and November 2019 and between February and March 2020. It forms part of my doctoral thesis on people’s lived experience of epidemic disease. The ethnographic study took place in Koutenga,[3] a peri-urban area around 15 km outside the capital Ouagadougou. Despite being categorised as a rural commune, central Koutenga resembles a modern Burkinabe town, with its contemporary buildings, billboards, traffic lights, and paved main street carrying the heavy traffic of trucks, cars, and motorcycles, and to a smaller degree, bicycles. However, after taking a turn off the main road, Koutenga quickly develops a more rural feel, with dirt roads, simple square houses, and goats and chickens running around freely. The Mossi are the original inhabitants of this area. However, as a result of the country’s highly mobile population and high population growth, Koutenga is today home to many different ethnic groups. In 2019, the estimated population of the municipality of Koutenga was around 285,000 (INSP 2020). Moreover, it is difficult to see where Ouagadougou ends and Koutenga starts, as the two have grown together. Koutenga is greatly affected by zoning operations (called lotissement in French) through which farmland is being transformed into land plots, a common urban planning method in neighbouring countries too (Körling 2020; Hilgers 2011; Hauer, Østergaard Nielsen, and Niewöhner 2018). Large areas of Koutenga town and two bordering villages were apportioned into more than 7,000 parcels of land between 1998 and 2014. While these zoning operations have come with the promise of further modernisation, such as electricity, modern housing, and businesses, few of the original local inhabitants have the means to afford them. In addition, many have had to change their way of life as their agricultural fields and gardens are transformed into land plots.
In Koutenga town there is a medical centre with a physician, an assistant doctor, a lab technician for the laboratory, various nurses, midwifes, and some administrative and technical staff such as pharmacists and cleaners. In the neighbourhood in which our study took place there is also a dispensary, run by a Catholic mission, which opened at the beginning of 2019. Around Koutenga town there are more than ten different private healthcare clinics. Many have laboratories and the ability to test for diseases, something neither the medical centre nor the dispensaries are able to do because of equipment being unavailable, broken, or out of stock. Because of the relative closeness of Ouagadougou, where higher level healthcare, diagnostics and services are available, it is common for families in Koutenga to host sick family members who have travelled from various villages in the country in the hope of treatment and a cure.
I conducted the study in close collaboration with a trained, local male research assistant (Landry) fluent in Moore, the main language spoken in the area. We initially conducted 50 semi-structured interviews with main caregivers,[4] of whom 35 were women and 15 men, and who were at times themselves sick. These caregivers were identified randomly by going from household to household in Koutenga, presenting the study and asking for permission to interview the main caregiver in the household. The interviews covered current or recent illnesses and deaths in the household. They were mainly conducted in Moore, although seven were conducted in French and one in Bissa. We both took notes during these interviews and more detailed notes after each one.
We subsequently conducted follow-up interviews (one or more) with 15 of these caregivers or sick persons[5] to get further details on the progression of the illnesses. These interviews were audio-recorded with the permission of the participant and then transcribed and translated into French. With ten of the caregivers or sick persons we kept in contact throughout the study, developing trusting relationships with them. We paid them informal visits, interviewed other family members about specific cases of illness or death (with the permission of the original interviewee), and on a few occasions accompanied them to healthcare services in Koutenga or Ouagadougou. In addition, several other sick people and caregivers, whom we met at the medical centre in Koutenga while they were waiting for their scheduled consultation, became our interlocutors.
When the COVID-19 pandemic hit Europe in March 2020, I was called home and Landry continued to carry out fieldwork as far as it was safe to do so.[6] Below, I briefly recount the diagnostic story of Caroline, one of the people we came to follow throughout our fieldwork.
Caroline and the blue plastic bag
We first met Caroline, a 36-year old woman and mother of three, at the beginning of October 2019. She had just been discharged from the nearby dispensary where she had been admitted for three days. She had initially fallen sick more than a month earlier, at the end of August, with dizziness, joint pains, and fever. Believing that it was ‘just’ a common type of malaria, which they confirmed at the medical centre where she went to take the test a couple of days later, she did not think it was anything serious. However, because she continued to be sick she went back to the medical centre a second and a third time. A diagnosis became important when Caroline’s condition worsened—one day she fainted while at work and had to be driven home on the back of a colleague’s motorbike. Later that same day her husband took her to the newly opened dispensary, run by a Catholic mission, where she tested positive for dengue fever, or palu dengue as it is referred to locally. Throughout our fieldwork, Caroline received a number of diagnoses, including malaria, dengue fever, and sinusitis, and treatments (Fig. 1). However, she never fully regained her health.
Caroline was ill throughout our fieldwork, and when I left Burkina Faso in March 2020 she had still not recovered. As her pain continued—a pain she described as feeling ‘as if her head was going to explode’—and time passed, Caroline and her family got more and more worried; worried as to what was the matter and worried about money, as it became more and more difficult for them to pay for examinations, tests, and treatments. After falling ill, Caroline had had to leave her job at the local water-filling factory, a job that paid her a daily income of approximately 2 US dollars. Her husband’s job, working in gardens several kilometres away from their home, did not bring much money into the household.
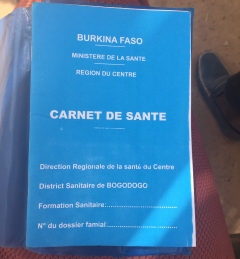
A large, blue plastic bag was central to Caroline’s interactions with the healthcare system. This blue plastic bag was filled with a mix of prescribed tablets, empty tablet cartons, prescriptions, diagnostic and test result papers, and her carnet de santé or health booklet. The tablets consisted of various antimalarial drugs, antibiotics, painkillers, and vitamins. However, Caroline herself did not know what all these prescribed drugs were; nor could she read what had been written on the prescriptions, on the diagnostic papers, or in her carnet de santé, as she had never been to school and is illiterate. Instead, she would point to the price written in red pen next to each drug on the prescription, as if to say that they had been able to purchase all the products she had been prescribed (the price of drugs is often written in red or green pen to distinguish it from the drugs themselves, which are listed in blue). The items in her plastic bag were important to Caroline, despite not being able herself to decode their specific meaning, and she kept the bag safe, next to her mattress in the corner of her small house. Being illiterate made it difficult for her to distinguish between the various papers which, with their biomedical language or practitioners’ unreadable handwriting, were difficult for a layperson to understand. Hence, Caroline made sure to take the plastic bag with her every time she went for a consultation.
Throughout Caroline’s diagnostic journey papers played a central role, as they often did for the people we met in Koutenga. During informal visits and talks about cases of illness or death, our interlocutors would often show us a clutch of medical papers, X-rays, scans, and prescribed medications as though they were pieces in a puzzle that could be put together. Two types of papers in particular,[7] referral papers and diagnostic papers, take on importance in diagnostic journeys. In the next sections, I show the motions and emotions these papers set off in sick people like Caroline.
Referral papers: Action and access
Among our interlocutors in Koutenga, referral papers take on importance because they trigger motion in the healthcare system. We often heard statements such as, ‘They gave us a paper to make the test […]’, or ‘They gave us the paper to go to XXX [one of the national hospitals]’, when our interlocutors described their diagnostic journeys. In this way, referral papers in the Burkinabe context work as technologies of visibility in themselves, rendering people visible between different levels of public healthcare. However, referral papers are also the means by which other technologies of visibility, that is, diagnostic technologies, can be accessed. Referral papers granted access (albeit not free access) to regional hospitals or national and university hospitals with their wider range of diagnostic possibilities compared with those of the dispensaries or medical centre in Koutenga. For Caroline, the referral paper was her means of getting access to higher levels of healthcare and diagnostics when the diagnostics and treatment at the dispensary and medical centre did not bring about the hoped-for cure:
There [at the dispensary] we were given two examinations to do, palu dengue and simple malaria. We were told it was palu dengue, not simple malaria. They started to treat me, treat, treat, treat, but as that did not heal, they gave us a paper to go to XXX [one of the national hospitals].
At the national hospital, Caroline took three blood tests which again came back positive for dengue fever.
Referral papers are essential if one is going to dare to turn up at a hospital, in order to mitigate the not uncommon risk of being refused entry at the door. In this way, referral papers represented a sense of confidence and assurance that one would be received by the hospital. Even when cases of illness had become critical, to the point of the sick person losing consciousness or having severe difficulties breathing, for example, our interlocutors would describe how they would first go to the dispensary or medical centre to get the paper. Only then would they continue on to one of the hospitals, where not just more diagnostics but also more medical equipment was available. Often, critically sick people died before they ever reached the hospital and before they received the referral paper from the medical centre or the dispensary. In these cases, the work of obtaining the technology of visibility, i.e., the referral paper, undermines the urgency of the situation and the health of the critically sick person. Thus, paperwork, in terms of referral papers, presented opportunities for action and access to higher levels of care and diagnostics, but also served as a bureaucratic obstacle especially in cases of critical illness and emergency.
Diagnostic papers: Knowledge
Fifty-six-year-old Boureima suffers from tuberculosis. We met him yesterday and got talking to him at the medical centre in Koutenga, where he had come for his weekly follow-up and medication. He invited us to his home, and so this morning we sit on the floor, in the shade of the overhang of his house.
‘Can you tell us a bit about your disease? How did it start?’ I ask.
‘When my illness started I was smoking cigarettes, and at one point I started having breathing problems. Then came the cough to the point I could not breathe. They told me I suffered from cough. It lasted for a long time. I was lucky, had I not gone to XXX [one of the national hospitals], I would have been dead already,’ Boureima replies.
‘Have you been told what illness you have?’ I continue.
‘It is what you said earlier, tuberculosis or whatever it is,’ Boureima replies and then pauses for a while before he gets up while saying, ‘I’ll get the papers, the results of the X-ray. Then we can see what is in there.’ A couple of minutes later he comes out with papers and X-ray images.
Our visit to Boureima was similar to many of our visits to people who had been searching for a diagnosis, often for several months and sometimes for more than a year. People would pull out their various health papers, X-rays, and scan images to show us. Boureima, unlike most others, had received a diagnosis and was undergoing care and treatment. He did not place a lot of emphasis on the specific diagnosis of tuberculosis, knowledge he considered to be for medical and educated people—sébe-ramba in Moore, literally meaning ‘paper people’ and referring to people working in administrative positions or those with degrees. Other scholars have similarly highlighted how rather than knowledge it is action and recognition that patients seek when looking for a diagnosis (Whyte 1997; Street 2014).
Diagnostic papers in all their forms—papers, images, scans, as well as the health booklet (in which test results and a presumptive diagnosis would often be noted down)—took on importance for sick people in Koutenga in their dealings with the public healthcare system at all levels. For them, the referral papers indicated an action while diagnostic papers and the health booklet contained knowledge to be kept and stored. Such knowledge is largely incomprehensible to the illiterate and the layperson in general. Thus, the importance of these papers lies in their contained knowledge, knowledge accessible only to healthcare workers. As the country’s healthcare system has no electronic or shared record-keeping, responsibility for keeping such papers safe and conveying them to the different facilities rests with the sick or their caregivers. They become an ‘archivist of their own interactions with the state health system’, as described by Street (2012, 11) in reference to patients in Papua New Guinea transporting their health booklets between scattered and disparate state health facilities. In this way the health booklet becomes a technology of social visibility, ‘a process by which patients are made apparent in a recognisably treatable form’ and elicit a response from the health system (Street 2012, 14).
As Brighenti notes, when accessing places of visibility attention needs to be paid to the modes of access, which for the marginalised may often be largely out of their control (2007). For many of our interlocutors in Koutenga, being responsible for the papers is a highly difficult and uncertain undertaking and some did not manage as well as Caroline did to keep everything safe. The incomprehensibility of the knowledge contained in the diagnostic papers might be why such papers were often lost, mixed up, or forgotten by the sick, as happened at times when people went to the hospitals in Ouagadougou; perhaps the similarity of the various papers to one another also contributed to the confusion. By contrast, we never observed instances of images of scans or X-rays being lost, forgotten, or mixed up. Thus, our observations in Burkina Faso suggest that the form of the papers plays a crucial role in the different ways that sick people like Caroline are able to engage with such technologies of visibility. When sick people fail to bring their diagnostic papers to their consultation, it is difficult for the practitioner to know what exactly has been done and what assumptions about their condition have been made. Consequently, tests and examinations might have to be conducted again. This was the case when Caroline was referred to the national hospital and the paper confirming her dengue fever diagnosis was not in her plastic bag. Having to take the test again was a costly affair, at 10.000 CFA francs (around 19 US dollars). It too came back positive for dengue fever and she was admitted to the hospital for one night for treatment and care.
The subtle difficulties and burdens that such papers give rise to are different from more deliberate exclusions from healthcare faced by sick people. Examples of the latter might include punishments, such as withholding health cards (which grant their holders access to free national healthcare services), meted out by health staff, as described by Cogburn (2020) in the context of maternal health in Tanzania. However, the papers may themselves lead to exclusion from care, by being liable to be lost or forgotten and thus requiring their holders to retake expensive and therefore sometimes unattainable tests. In these ways, paperwork, in terms of its role in conveying diagnoses and knowledge between health institutions, thus simultaneously presented both an opportunity and a burden for many people.
Technologies of visibility—between hope and despair
By means of technologies of visibility, various papers, and diagnostic technologies, sick people and their families hope not just for any action or treatment but for targeted and effective treatment. As Caroline’s husband stated, with Caroline nodding in agreement when we were discussing the importance of testing:
If you do not test to know the disease, you can spend your money unnecessarily by paying for products that are not the medicines for the disease you are suffering from. But if you take the test and you will know the disease you suffer from, then it is easy to do the treatment.
Thus, testing to know or to see the disease was about receiving targeted treatment, being able to treat the condition effectively, and not wasting money. The ’cost-effectiveness’, the need ’not to waste money’, is naturally important to people in this context, where almost all health services are provided on the principle of user fees. Undergoing tests, laboratory examinations, X-rays, and CT scans, and buying prescribed medicine is expensive; in Caroline’s case, her CT scan cost 40.000 CFA francs, which is around two months’ salary for her. When people showed us X-rays and scan images there was almost a sense of pride in that they also showed that they or their families had been able to pay for these examinations.
Unlike Caroline and most of the other sick people we visited in Koutenga, Boureima had received a diagnosis and targeted treatment and care. He felt lucky. This ’feeling lucky’ points to the considerable uncertainty surrounding receiving a diagnosis and care, as well as to the life and death stakes involved. In our interlocutors’ quest for health within the healthcare system, papers and diagnostic technologies become objects of hope: hope that these technologies will set things in motion; hope that they will make them and their physical ailment visible to the healthcare system; and ultimately hope that they will regain their health. At the same time, these same items inspired uncertainty, in terms of their having to manage the various papers and the financial uncertainties arising from the possibility of new referrals for further tests and examinations. Lastly, they engendered despair, when diagnostic technologies failed to realise the potential of visibility. When Caroline received the referral for her CT scan, she expressed both uncertainty and hope: ’There is no money but we will ask for some and if we get it, we will go and do the scanner and see. If we do the scanner, maybe they will see the disease. If they see the disease, they might help us to cure it’. Thus, with this referral paper new questions and financial uncertainties now arose. Should she have the CT scan, and if so, how would they be able to pay for it? Such uncertainties arose throughout Caroline’s diagnostic journey. On the one hand, when she obtained papers that granted her access to different diagnostic technologies it generated hope and expectations. On the other hand, when diagnostic tests or examinations that they had gone to great lengths to access were indeterminate or did not show anything, it caused her frustration and disappointment. When she managed to do the CT scan but it did not reveal anything that could lead to a diagnosis, Caroline found herself immobilised, not knowing what to do next:
[The doctor] told me that by doing the CT scan you can tell if it is [in fact] sinusitis. Because it could be another disease and that is why it does not cure when we treat it. […] But if we do the scanner, that is where we will detect all diseases. I did it and then we saw nothing there. […] When we did the scanner and it was the machine which took out the paper and stated that there is nothing there, then they [health staff] do not know what to do.
Because the scan, perceived to be a more accurate diagnostic technology than the X-ray, could not reveal anything, and because the healthcare staff therefore did not know what to do, according to Caroline, the uncertainty and powerlessness seemed profound. Caroline did not know what to do next. All the activity she had engaged in up until now seemed to be at an end. She was filled with not anger or blame but rather resignation, as she uttered: ‘You know, when you're sick today, they are just going to try everything, as you are seeking a cure’. Caroline’s statement reflected her feelings on having been sent to take various tests and treatments without success, and about the endless possibilities for referrals and tests there are within the healthcare system.
This latter sentiment in many ways resembles the bureaucracy described by Nuijten as a ‘hope-generating machine’, giving the message that everything is possible but rarely fulfilling such promises (2004, 211). Unlike the bureaucracy and its officials in Mexico who ‘are always willing to initiate procedures’ (Ibid., 211), healthcare workers in Burkina Faso’s public sector often seem reluctant to do the same. Instead, they often give a presumptive diagnosis, possibly in the hope that when the sick return home they recover or find a way to relieve their symptoms themselves. That certainly appeared to be the case when the doctor at the medical centre told Caroline that she suffered from chronic sinusitis, despite not being able to confirm that from her X-ray. He then gave her advice on how she could use a face cloth to protect herself from dust and from smoke when cooking and had prescribed some painkillers to stop the worst of the pain. In other instances where people had become critically ill and the healthcare system had little or no means to help, family members often revealed that healthcare workers had given them a (non-confirmed) diagnosis as a way of generating hope. This was the case with 40-year old Paul, who had died the year before. As his brother Charles explained: ‘When we were told that he had tuberculosis, Paul was happy because he knew that if it was this, then it would be enough that we put him on treatment, he would be cured’. In retrospect, Charles saw the attribution of a diagnosis of tuberculosis as a way of providing hope for his brother. Tuberculosis was something that could be treated. Paul died a few days later.
In the same way, most of the sick people we followed in Koutenga never became visible to the clinical gaze in terms of receiving a diagnosis followed by effective treatment and care. Some, like Paul, died; some continued their search; and others returned to their home village when the symptomatic treatment they received relieved their pain. I do not know what next steps Caroline and her family initiated—whether she continued in her struggle to make herself visible to the healthcare system, whether she gave up, or whether, as many did, she resorted to taking the traditional medicine of the villages.
Conclusion
In this article, I have shown how sick people like Caroline attempt to make themselves and their conditions visible to the public healthcare system in Burkina Faso by means of papers and diagnostic technologies. I have followed other scholars in exploring how people engage with such technologies of visibility and specifically I have shed light on how two types of papers—referral papers and diagnostic papers—take on significance in the quest for access to other technologies of visibility, i.e., diagnostic tests, and in conveying knowledge between the different healthcare levels. However, the illegible form of such papers for the sick and their family members often obscures which papers are important and in which situations and can therefore hinder people’s effective interaction with, and access to, diagnostic technologies and care. This leads to subtle exclusions of care. Furthermore, papers and diagnostic technologies simultaneously engender hope, uncertainty, disappointment, and despair for the sick seeking a cure. There are copious numbers of referral papers that can be written and diagnostic examinations that can be performed. However, with each of these possibilities, new uncertainties, especially financial ones, arise. Along the way many people give up or are immobilised and despairing, as Caroline was, when faced with diagnostic ambiguity after all their pain and their emotional and financial struggles. In low-resource contexts, where healthcare systems are in many ways designed to handle diseases separately, there are bound to be gaps in the clinical gaze (Gibson 2004) and there are bound to be people like Caroline and Paul who fall outside of it. Focusing on technologies of visibility such as papers and diagnostic tests, and on the opportunities (hope) and challenges (uncertainty) they engender, extends the growing literature on ways of becoming visible in order to access healthcare. Bringing the experiences of sick people to the fore is especially important in an era of evidence-based medicine in which the focus on quantifiably measurable forms of reason and accountability readily overlook such experiences (Adams 2016).
Acknowledgements
I would like to express my sincere gratitude to our interlocutors in Koutenga, who welcomed us into their lives and participated in this research; and to Landry Bambara, my research assistant, for his valuable contribution to the study. Thanks also to Helle Samuelsen, Brian McGahey, Eva Otte, Erika Skov, Ida Vandsøe Madsen, and colleagues in the Health and Life Conditions research group at the Department of Anthropology, University of Copenhagen, for their valuable comments on ethnographic cases and drafts of this article. I am grateful to the two anonymous reviewers and the editors of MAT for their constructive comments, which have strengthened the article. This study is part of a larger collaborative research project, ‘Emerging Epidemics: Improving Preparedness in Burkina Faso’, that is supported by a grant awarded by the Ministry of Foreign Affairs, Denmark (project no. 17-06-KU).
About the author
Pia Juul Bjertrup is a medical anthropologist and PhD student at the Department of Anthropology, University of Copenhagen. She has been part of several research projects in the areas of refugee mental health, HIV and TB, epidemics and COVID-19, and has conducted ethnographic fieldwork in Greece, Eswatini, Burkina Faso, Uganda, and Malawi.
Footnotes
-
All names are pseudonyms.↩︎
-
CFA stands for Communauté financière d'Afrique or African Financial Community and refers to both the Central African CFA franc (XAF) and the West African CFA franc (XOF), which are interchangeable as they hold the same monetary value against other currencies.↩︎
-
Koutenga is a pseudonym. I use the term to denote the municipality, the town centre, and the specific neighbourhood in which the study took place.↩︎
-
A caregiver is defined as a mother or father to children below the age of 18 years.↩︎
-
I use the term ‘sick person’ rather than ‘patient’ because I believe it better captures the experience of the people in Burkina Faso. According to the Merriam–Webster dictionary, the noun ‘patient’ refers to 1) an individual awaiting or under medical care and treatment, 2) the recipient of any of various personal services, or 3) one that is acted upon (Merriam–Webster 2021). These definitions hint at the more passive connotations of the role and to someone receiving services. This does not correspond well with the activity, work, and struggles that people in Burkina Faso undergo when attempting to make themselves visible to the biomedical gaze.↩︎
-
Telephone interviews were conducted with interlocutors where rapport had already been built.↩︎
-
The Moore word sébrè can mean book, booklet, and paper, and in its entirety refers to all written documents.↩︎
References
Adams, Vincanne. 2016. ‘Introduction’. In Metrics: What Counts in Global Health, edited by Vincanne Adams, 1–17. Durham, NC: Duke University Press.
Ansumana, Rashid, Fatmata Bah, Kan Biao, Doris Harding, Mohamed B. Jalloh, Ann H. Kelly, Francess Koker, et al. 2020. ‘Building Diagnostic Systems in Sierra Leone: The Role of Point-of-Care Devices in Laboratory Strengthening’. African Journal of Laboratory Medicine 9 (2): 1–5. https://doi.org/10.4102/ajlm.v9i2.1029.
Biehl, João. 2005. ‘Technologies of Invisibility: Politics of Life and Social Inequality’. In Anthropologies of Modernity: Foucault, Governmentality, and Life Politics, edited by Jonathan Xavier Inda, 248–71. Malden, MA: Blackwell https://doi.org/10.1002/9780470775875.ch10.
Bonko, Massa dit Achille, Francois Kiemde, Marc Christian Tahita, Palpouguini Lompo, Athanase M. Some, Halidou Tinto, Michael Boele van Hensbroek, Petra F. Mens, and Henk D. F. H. Schallig. 2019. ‘The Effect of Malaria Rapid Diagnostic Tests Results on Antimicrobial Prescription Practices of Health Care Workers in Burkina Faso’. Annals of Clinical Microbiology and Antimicrobials 18 (5): 1–9. https://doi.org/10.1186/s12941-019-0304-2.
Brighenti, Andrea. 2007. ‘Visibility: A Category for the Social Sciences’. Current Sociology 55 (3): 323–42. https://doi.org/10.1177/0011392107076079.
Chandler, Clare, and Justin Dixon. 2019. ‘Opening up “Fever”, Closing down Medicines’. Medicine Anthropology Theory 6 (4): 53–79. https://doi.org/10.17157/mat.6.4.676.
Cogburn, Megan D. 2020. ‘Homebirth Fines and Health Cards in Rural Tanzania: On the Push for Numbers in Maternal Health’. Social Science & Medicine 254 (June): 112508. https://doi.org/10.1016/j.socscimed.2019.112508.
Foucault, Michel. 2012. The Birth of the Clinic. London: Routledge. https://doi.org/10.4324/9780203715109.
Gibson, Diana. 2004. ‘The Gaps in the Gaze in South African Hospitals’. Social Science & Medicine 59 (10): 2013–24. https://doi.org/10.1016/j.socscimed.2004.03.006.
Haenssgen, Marco J., Nutcha Charoenboon, Thomas Althaus, Rachel C. Greer, Daranee Intralawan, and Yoel Lubell. 2018. ‘The Social Role of C-Reactive Protein Point-of-Care Testing to Guide Antibiotic Prescription in Northern Thailand’. Social Science & Medicine 202 (April): 1–12. https://doi.org/10.1016/j.socscimed.2018.02.018.
Hauer, Janine, Jonas Østergaard Nielsen, and Jörg Niewöhner. 2018. ‘Landscapes of Hoping—Urban Expansion and Emerging Futures in Ouagadougou, Burkina Faso’. Anthropological Theory 18 (1): 59–80. https://doi.org/10.1177/1463499617747176.
Hilgers, Mathieu. 2011. ‘L’autochtonie comme capital: Appartenance et citoyenneté dans l’Afrique urbaine’. Social Anthropology 19 (2): 143–58. https://doi.org/10.1111/j.1469-8676.2011.00145.x.
INSP, Institut National de Santé Publique. 2020. ‘État de Santé de la Population du Burkina Faso. Rapport 2019’. https://dicames.online/jspui/bitstream/20.500.12177/3982/1/Rapport_Etat_Sante_Pop_BF%202019_Final.pdf.
INSP, Institut National de Santé Publique. 2020. ‘Cinquième Recensement Général de la Population et de l’Habitation du Burkina Faso. Résultats Préliminaires’. https://www.insd.bf/contenu/documents_rgph5/RAPPORT_PRELIMINAIRE_RGPH_2019.pdf.
Klatman, Emma Louise, Martin McKee, and Graham David Ogle. 2019. ‘Documenting and Visualising Progress towards Universal Health Coverage of Insulin and Blood Glucose Test Strips for People with Diabetes’. Diabetes Research and Clinical Practice 157 (November): 107859. https://doi.org/10.1016/j.diabres.2019.107859.
Körling, Gabriella. 2020. ‘Bricks, Documents and Pipes: Material Politics and Urban Development in Niamey, Niger’. City & Society 32 (1): 23–46. https://doi.org/10.1111/ciso.12240.
Liggins, Arlena Siobhan. 2020. Making Diabetes: The Politics of Diabetes Diagnostics in Uganda. Bielefeld, Germany: Transcript-Verlag.
Livingston, Julie. 2012. Improvising Medicine: An African Oncology Ward in an Emerging Cancer Epidemic. Durham, NC: Duke University Press.
Livingston, Julie. 2020. ‘When Sickness Comes in Multiples: Co-Morbidity in Botswana’. In Biosocial Worlds: Anthropology of Health Environments beyond Determinism, edited by Jens Seeberg, Andreas Roepstorff, and Lotte Meinert, 146–67. London, UK: UCL Press. https://doi.org/10.2307/j.ctv13xpsqt.12.
McKay, Ramah. 2012. ‘Documentary Disorders: Managing Medical Multiplicity in Maputo, Mozambique’. American Ethnologist 39 (3): 545–61. https://doi.org/10.1111/j.1548-1425.2012.01380.x.
McKay, Ramah. 2018. Medicine in the Meantime: The Work of Care in Mozambique. Durham, NC: Duke University Press.
Merriam-Webster. 2021. ‘Patient’. Merriam–Webster.Com Dictionary. 2021. https://www.merriam-webster.com/dictionary/patient.
Ministère de la Santé du Burkina Faso. 2016. ‘Plan stratégique intégré de lutte contre les maladies non transmissibles 2016–2020’. https://www.iccp-portal.org/system/files/plans/BFA_B3_Plan%20SIMNT_FINAL_27-09-2016_F.pdf.
Nuijten, Monique. 2004. ‘Between Fear and Fantasy: Governmentality and the Working of Power in Mexico’. Critique of Anthropology 24 (2): 209–30. https://doi.org/10.1177/0308275X04042655.
Oudshoorn, Nelly. 2008. ‘Diagnosis at a Distance: The Invisible Work of Patients and Healthcare Professionals in Cardiac Telemonitoring Technology’. Sociology of Health & Illness 30 (2): 272–88. https://doi.org/10.1111/j.1467-9566.2007.01032.x.
Ouédraogo, Mady, Toussaint Rouamba, Sékou Samadoulougou, and Fati Kirakoya-Samadoulougou. 2020. ‘Effect of Free Healthcare Policy for Children under Five Years Old on the Incidence of Reported Malaria Cases in Burkina Faso by Bayesian Modelling: “Not Only the Ears but Also the Head of the Hippopotamus”’. International Journal of Environmental Research and Public Health 17 (2): 417. https://doi.org/10.3390/ijerph17020417.
President’s Malaria Initiative. 2019. ‘Burkina Faso Malaria Operational Plan FY 2019’. www.pmi.gov.
Prince, Ruth. 2019. ‘Pandemic Publics: How Epidemics Transform Social and Political Collectives of Public Health’. In The Anthropology of Epidemics, edited by Ann H. Kelly, Frédéric Keck and Christos Lynteris, 135–53. New York, NY: Routledge. https://doi.org/10.4324/9780429461897-9.
Rasmussen, Stine Loft, and Sundeep Sahay. 2017. ‘Handling Uncertainty in Disease Surveillance and Response’. Working Paper 3/2017, Information Systems Working Papers, University of Oslo, Norway. http://www.mn.uio.no/ifi/english/research/groups/is/publications/working-papers-in-information-systems.
Ridde, Valéry, Mabel Carabali, Antarou Ly, Thomas Druetz, Seni Kouanda, Emmanuel Bonnet, and Slim Haddad. 2014. ‘The Need for More Research and Public Health Interventions on Dengue Fever in Burkina Faso’. PLOS Neglected Tropical Diseases 8 (6): e2859. https://doi.org/10.1371/journal.pntd.0002859.
Ridde, Valéry, and Pierre Yaméogo. 2018. ‘How Burkina Faso Used Evidence in Deciding to Launch its Policy of Free Healthcare for Children under Five and Women in 2016’. Palgrave Communications 4 (1): 1–9. https://doi.org/10.1057/s41599-018-0173-x.
Samuelsen, Helle. 2020. ‘Accelerated Fragility: Exploring the Supply–Demand Nexus in Health Facilities in Rural Burkina Faso’. Africa 90 (5): 934–51. https://doi.org/10.1017/S0001972020000662.
Star, Susan Leigh, and Anselm Strauss. 1999. ‘Layers of Silence, Arenas of Voice: The Ecology of Visible and Invisible Work’. Computer Supported Cooperative Work: The Journal of Collaborative Computing 8 (1/2): 9–30. https://doi.org/10.1023/A:1008651105359.
Street, Alice. 2011. ‘Artefacts of Not-Knowing: The Medical Record, the Diagnosis and the Production of Uncertainty in Papua New Guinean Biomedicine’. Social Studies of Science 41 (6): 815–34. https://doi.org/10.1177/0306312711419974.
Street, Alice. 2012. ‘Seen by the State: Bureaucracy, Visibility and Governmentality in a Papua New Guinean Hospital’. Australian Journal of Anthropology 23 (1): 1–21. https://doi.org/10.1111/j.1757-6547.2012.00164.x.
Street, Alice. 2014. Biomedicine in an Unstable Place: Infrastructure and Personhood in a Papua New Guinean Hospital. Durham, NC: Duke University Press.
Street, Alice. 2018. ‘The Testing Revolution: Investigating Diagnostic Devices in Global Health’. Somatosphere, Science, Medicine, and Anthropology (blog), April 9, 2018. http://somatosphere.net/2018/testing-revolution.html/.
Street, Alice, Emma Michelle Taylor, James Smith, and Ian Harper. 2014. ‘Diagnostics for Development’. Somatosphere, Science, Medicine, and Anthropology (blog), May 30, 2014. http://somatosphere.net/2014/diagnostics-for-development.html/.
Wendland, Claire L. 2010. A Heart for the Work: Journeys through an African Medical School. Chicago, IL: University of Chicago Press.
Whyte, Susan Reynolds. 1997. ‘Misfortune and Uncertainty’. In Questioning Misfortune: The Pragmatics of Uncertainty in Eastern Uganda, edited by Susan R. Whyte, 13–33. Series Number 4 of Cambridge Studies in Medical Anthropology Cambridge, UK: Cambridge University Press.
Whyte, Susan Reynolds, Sjaak van der Geest, and Anita Hardon. 2002. Social Lives of Medicines. Series Number 10 of Cambridge Studies in Medical Anthropology. Cambridge, UK: Cambridge University Press.
Yellapa, Vijayashree, Narayanan Devadasan, Anja Krumeich, Nitika Pant Pai, Caroline Vadnais, Madhukar Pai, and Nora Engel. 2017. ‘How Patients Navigate the Diagnostic Ecosystem in a Fragmented Health System: A Qualitative Study from India’. Global Health Action 10 (1): 1350452.https://doi.org/10.1080/16549716.2017.1350452.
Zongo, Sylvie, Mabel Carabali, Marie Munoz, and Valéry Ridde. 2018. ‘Dengue Rapid Diagnostic Tests: Health Professionals’ Practices and Challenges in Burkina Faso’. SAGE Open Medicine 6 (August). https://doi.org/10.1177/2050312118794589.