COVID-19, a disease induced by SARS-CoV-2, became a worldwide pandemic while SARS, a disease induced by a closely related virus, SARS-CoV, was successfully contained. This is because COVID-19, unlike SARS, can be spread by people who do not display any symptoms of disease, either because they are in the early stages of the infection or because their infection remains clinically silent. This research article traces the complex history of the diagnosis of symptom-free (or asymptomatic) carriers of pathogens, a term inseparably linked to the rise of the laboratory diagnosis of pathogens. Only such a diagnosis can reveal that an apparently healthy individual harbours dangerous bacteria, parasites, or viruses. The article begins with the iconic story of ‘Typhoid Mary’, a New York cook found to be an asymptomatic carrier of typhoid fever microbes. It then discusses divergent approaches to the treatment of symptom-free carriers of hookworm and controversies around the screening of HIV carriers, especially before the development of anti-retroviral treatments. It concludes with a presentation of the debates on the role of asymptomatic carriers in the spread of COVID-19 and of the differences between the approaches of countries seeking to eliminate this disease, a goal that itself entails tracing and isolation of all asymptomatic carriers of coronavirus, and those trying to contain it, an approach that tolerates the presence of a limited number of ‘invisible’ virus carriers.
Hidden Perils
Diagnosing asymptomatic disease carriers
—
Abstract
Introduction: A truly frightening diagnosis
One of the scariest events in the early history of the COVID-19 pandemic was probably noticed only by a handful of experts. On 24 January 2020, a group of Chinese researchers published in The Lancet a description of a cluster of six infections by the new coronavirus (then temporarily named 2019-nCoV by the World Health Organisation [WHO]) in a family from the city of Shenzhen in Guangdong province who had stayed in Wuhan, the epicentre of the outbreak of the new coronavirus, from 31 December 2019 to 4 January 2020. The first two cases were hospitalised with ‘unexplained pneumonia’ at the University of Hong Kong-Shenzhen Hospital on 10 January. Three other members of the same family were hospitalised with similar symptoms during the following two days. All displayed ‘ground-glass lung opacities’, a visual signature of the new disease, on a computed tomography (CT) scan. In addition, all hospitalised patients tested positive for the RNA of the new coronavirus. In addition, however, one member of this family, a 10-year-old child who had visited Wuhan and who displayed some lung anomalies on a CT scan but did not show any clinical symptoms of coronavirus infection, also tested positive on a reverse transcription polymerase chain reaction (RT-PCR) test.
The Shenzhen patients may have been among the first users of diagnostic tests for the new coronavirus. The RT-PCR test was developed in record time. The WHO learned of the presence of an ‘atypical pneumonia’ in Wuhan on 30 December 2019. By 9 January 2020, Chinese scientists confirmed that this pneumonia was induced by a previously unknown coronavirus and made public the sequence of its RNA. On 16 January, Christian Drosden’s group at the Charité Hospital, Berlin, published a template for a RT-PCR diagnostic test for the new coronavirus. This test examined secretions for the virus, thus indicating whether the tested person was infected and thus could infect others. The new test was rapidly reproduced by Chinese and Hong-Kong scientists, and almost immediately put at the disposal of clinicians. Authors of the article about the Shenzhen cluster immediately recognised the epidemiological importance of the discovery that an individual can be infected, and thus spread the virus, without any perceptible clinical manifestations of disease. They stressed that ‘it is crucial to isolate patients and trace and quarantine contacts as early as possible, because asymptomatic infection appears possible’ (Chan et al. 2020).
The authors of The Lancet article pointed to a theoretical possibility of transmission of the new coronavirus by symptom-free individuals. Less than two weeks later, a group of physicians from the city of Anyang, in the province of Henan, provided formal proof of such transmission, although the article that described their findings was not published until 20 February 2020 (Bai et al. 2020). On 10 January 2020, a young woman travelled from Wuhan to Anyang, where in the next few days she met five relatives. At that time, there were numerous cases of the new coronavirus in Wuhan, but no known cases in Anyang. On 17 January, one of the young woman’s relatives developed symptoms of respiratory infection. Another developed similar symptoms on the 22 January. Two others followed on the 25 January, and the fifth developed symptoms on the 26 January. All five patients were hospitalised at the Anyang District Hospital, two with severe and three with moderate pneumonia. All displayed ground-glass lung opacities on a CT scan and were PCR positive. The young woman strongly suspected to be the index case was also isolated as a precaution. Her PCR test was positive too, but she remained symptom-free and, unlike the child in the Shenzhen cluster, did not display radiological anomalies. The article that described the Anyang cluster concluded that ‘if the findings in this report of presumed transmission by an asymptomatic carrier are replicated, the prevention of COVID-19 infection would prove challenging’ (Bai et al 2020, 1407).
‘Challenging’ was an understatement. The China Health Agency officially notified the WHO of human-to-human transmission of the new coronavirus on 20 January 2020, but persisting rumours about a ‘new SARS’ in Wuhan had started to circulate on social media in the last days of December 2019. These rumours intensified in early January (see, e.g., You 2020; Fang 2020).
The SARS epidemic of 2003, the first major coronavirus outbreak, was a frightening episode that left important traces in Southeast Asia. Successful control of the SARS outbreak was attributed above all to the fact that only symptomatic patients were contagious. Visibility of infectious individuals facilitated their isolation, the strict quarantine of their contacts, the closing of infected sites, and the interruption of transmission chains. Discussing the SARS episode, many experts (e.g., Enserink 2003; Anderson et al. 2004) stressed that humanity was very lucky during this outbreak, but its luck might not hold as well the next time. An akin disease transmissible by symptom-free individuals would be much more difficult to contain (Heymann 2004; Löwy 2020). The seemingly commonplace story of a young woman who infected five of her relatives without falling sick herself strongly pointed to such a daunting possibility.
Until recently, social scientists who have studied diagnosis were mainly interested in topics such as the diagnosis of chronic pathologies; medicalisation and demedicalisation (Brown 1995); the blurring of the boundaries between disease and risk (Rosenberg 2002); and problems linked with the widespread use of genetic tests (Juttel and Nettleton 2011)—that is, problems that are managed on the level of individuals or, when dealing with hereditary conditions, of families. In contrast, the diagnosis of transmissible pathologies is a public health problem. From the early 20th century onwards, scientists have known that symptom-free individuals can spread pathogens, unaware of the danger they represent to others (Mendelsohn 1998). To limit this danger, sanitary authorities have focused on the identification of asymptomatic carriers, the prevention of transmission of pathogens on a population level, or a combination of these two approaches.
Until the 20th century, diagnosis was at the very centre of the ‘intransmissible knowledge’ of the clinician, itself acquired through experience, and was impossible to codify or objectify (Lawrence 1985). Laboratory diagnosis of pathogens radically transformed clinical medicine, but also public health (Latour 1988; Löwy 1994; 2015). The search for pathogens that put the community at risk involved the relatively non-controversial management of pathogen risk ‘without people’—i.e., the surveillance of water supplies and food and the promotion of sanitary measures (Sturdy and Cooter 1998; Hamlin 1990)—as well as the more problematic management of such risk ‘with people’. This latter form of management attempted to prevent the spread of microbes by targeting the carriers of pathogens, not infrequently by coercive means (Worboys 2000; Hardy 2015). Imposing restrictions on sick carriers of microbes was somewhat easier, especially if the disease reduced their mobility. Still, a forced long-term isolation, such as the one described by Betty MacDonald (1948) in her (very amusing, but on some level rather scary) bestselling book The Plague and I, which describes her nine-month-long stay in a tuberculosis sanatorium, might have been very difficult for the patient. Severe curtailment of a person’s freedom is, however, especially problematic when imposed on people who see themselves as perfectly healthy. In these cases, individual and collective rights may clash violently. The historic examples investigated in this research article display the complex dilemmas created by such situations. They make visible the multiple ways expertise and laboratory practices shape collective responses to transmissible pathologies and the complex negotiations regarding the uses and reliability of diagnostic tools.
‘Typhoid Mary’: Science, myth, and the power of the state
The propagation of pathogens by symptom-free individuals is an especially perilous situation because it conjugates two levels of invisibility—that of the pathogen itself and that of the danger of contact with the innocuous-looking people who spread it. Accusations that external or alien groups deliberately provoke epidemics have been made since antiquity. Such accusations reverberate in medieval stories of the poisoning of wells and food sources by Jews, Arabs, or other presumed enemies. Moreover, colonisers often assumed that while native people were ‘racially immune’ to diseases that affected newcomers, they could still spread these diseases, a frequent justification for the physical separation of native and coloniser populations (the observation that the locals were less affected by selected ‘tropical diseases’ was accurate, but not its racial explanation: they became immunised to such diseases through exposure during childhood). The concept of ‘asymptomatic carrier’ of pathogens was, in contrast, a direct consequence of the rise of laboratory studies of invisible pathogens. An ‘asymptomatic person’ is a ‘normal’ and healthy individual until a laboratory diagnosis proves the contrary.
The image of a person who, while looking perfectly harmless, is in fact a terrifying propagator of disease and death is indissociably linked with the history of ‘Typhoid Mary’. Mary Mallon, a skilled Irish cook who worked in New York, was revealed to be an asymptomatic carrier of typhoid bacilli following a series of typhoid outbreaks in the upper-class households where she worked. These outbreaks were seen as especially frightening because typhoid fever, a disease usually linked to poverty and squalor, was rare among the affluent at the time. In 1907, a New York sanitary authority investigation team lead by Georges Soper found that Mallon was the source of these outbreaks. Mallon refused to undergo an ablation of the gall bladder, a risky surgery which was then erroneously believed to cure the carrier state. She also refused to abandon her work as a cook. As a consequence, she was obliged to quarantine on North Brother Island near New York City, an isolation facility for tuberculosis patients. She was also given, against her wishes, treatments meant to reduce the secretion of typhoid bacilli; these treatments did not work, however. Mallon strongly resisted what she believed to be an unjust persecution, all the more so because several other carriers of typhoid bacilli, mostly men of somewhat higher social standing, were not quarantined but instead were given instructions on how to prevent infecting others and made to promise that they would obey these instructions (Leavitt 1992; 1997).
Vilified by New York newspapers, which dubbed her ‘Typhoid Mary’, Mallon decided in 1909 to sue the City of New York for illegal detention. Her petition to the court was rejected. Nevertheless, in 1910, the New York State Commissioner of Health agreed to free her if she would promise not to work as a cook. Mallon at first respected the condition of her release and worked as a laundress, but the job was difficult and poorly paid. She then returned to work as a cook, this time in less prestigious settings, under the assumed name of Mrs Brown. She was found in 1915 following a severe typhoid outbreak in the Sloane Maternity Hospital in Manhattan, where she was working, and was ordered again to quarantine on North Brother Island. This time she did not protest, and remained in isolation until the end of her life. Mallon’s quarantine conditions on North Brother Island improved with time. She was given an individual cottage, was allowed occasional trips to the mainland, and was gainfully employed, first as a helper in the tuberculosis hospital and then, from 1925 onwards, as a laboratory assistant. A photograph of Mallon from the early 1930s shows a tall, solidly built middle-aged woman with round glasses wearing a long laboratory coat. Without the caption, which indicates that this is the in/famous ‘Typhoid Mary’, the photograph might have been interpreted as an image of a female scientist (Leavitt 1997, 196). A stroke in 1932 left Mallon disabled and put an end to her work in the laboratory. Mallon died on North Brother Island in 1938. Right until the end of her life, she was reported to be very angry about her transformation into a symbol of malevolent contagion (Leavitt 1997).
‘Typhoid Mary’ was transformed into a modernised version of the scary figure of the plague-propagating stranger. But, unlike the medieval legends in which a malevolent diffuser of the plague is unmasked by a divine sign such as a bleeding communion wafer, the modern plague spreader is exposed by a microscope and a Petri dish. The icon ‘Typhoid Mary’, a mythical figure in that she was part concept and part human, was often dissociated from the life of the woman Mary Mallon. From the 1980s onwards, historians became interested in the woman behind the symbol. Mary Mallon became the subject of novels, plays, and visual artworks. Newer versions of Mallon’s story have been more sensitive to the sadness of her life, her isolation in New York, and her discrimination as a poor migrant Irish woman. In the AIDS era, the more recent renderings of Mallon’s life stressed the dangers that can lurk in the most unexpected places. The celebrity chef and writer Antony Bourdain published a moving account of Mary Mallon’s life seen from a different perspective. To him, she was a cook, someone proud of her professional and culinary achievements, and who was destroyed by forces she was unable to grasp and powerless to control. This account reminds us that there is more to Mary Mallon’s life than the story of a carrier of pathogenic microbes (Bourdain 2005).
Above all, however, Mary Mallon’s story became intertwined with the social, cultural, and political history of bacteriology, especially in the US. In the early 20th century, bacteriological diagnosis was a young science, only recently applied to the management of public health (Sturdy and Cooter 1998). Mallon’s story made visible the ways scientific expertise and laboratory practices shape responses to outbreaks of infectious diseases (Steere-Williams 2020). A growing awareness of the active role of people in spreading dangerous microbes was extended from careless housewives and untidy servants—problems that could be managed with education and vigilance—to the much more threatening figures of asymptomatic carriers of pathogenic microbes, not infrequently suspected of malicious intentions (Tomes 1998, 237). Since typhoid fever was seen mainly as a disease of the urban poor, one of the most scandalous elements of Mallon’s story was the repeated contamination of upper-class families—people who lived in houses with running water; tiled bathrooms; water closets; and modern, functional kitchens, and who trained their servants to respect hygiene rules (Tomes 1998). The story of typhoid bacilli carriers could be seen as making visible the limits of an exclusive focus on microbes and the need to take into consideration other variables that may affect the diffusion of pathogens (Leavitt 1992). This story could alternatively be presented as the ultimate triumph of the view that put the hunt for dangerous microbes at the very centre of public health endeavours (Mendelsohn 1995). Mary Mallon’s story displays the tensions between individual rights and public health considerations as well as their articulation through debates about the uses and reliability of diagnosis. It also draws attention to issues related to gender, class, and social status (Leavitt 1997). In Mallon’s case, the sanitary authorities elected to focus on tracing and the ‘neutralisation’ of a dangerous spreader of microbes, perhaps because they estimated that long-term symptom-free carriers of typhoid bacilli (especially those who, because of their occupation, put many people at risk) were relatively rare. This was, however, not the case for asymptomatic carriers of hookworm: such carriers were very frequent in affected populations.
Hookworm: Treating a disease or eliminating a risk?
Hookworm is a parasitic disease induced by two closely related species of intestinal worms, Ankylostoma duodenum and Necator americanus. Heavily infected people suffer from weakness, anaemia, and chronic fatigue, while infected children display a marked failure to thrive. This infection, even more than typhoid fever, has been linked with poverty, especially in the countryside, because the spread of hookworm is enabled by, for example, walking barefoot and a lack of latrines, which are typical manifestations of ‘primitive conditions’ in rural areas. Hookworm is relatively easy to diagnose because the parasite’s eggs are visible in the faeces under a low-power microscope. In the early 20th century, physicians used compounds such as thymol and extract of black fern to induce the expulsion of the parasites. The treatment was not always effective and had unpleasant side effects; nevertheless, hookworm was classified as a curable disease (Loss 1905). Hookworm is a disease of warm climates. It is highly infectious and, even today, in some regions the majority of inhabitants carry the worm in their gut, although the severity of the infestation by this parasite varies greatly. A disease strongly correlated with pollution, dirt, and faecal contamination, hookworm has long been seen as a symbol of the inferiority and backwardness of native populations in tropical and sub-tropical areas (Anderson 1995). Because the presence of this intestinal worm induces anaemia and fatigue, hookworm has historically been presented as the cause of the innate ‘laziness’ of inhabitants of warm climates, a charitable explanation for their presumed lower levels of energy and lack of initiative (Ettling 1981).
It is easy to ascertain the presence of hookworm but less easy to decide what a positive diagnosis means and what should be done about it from a public health perspective. An anti-hookworm campaign can either aim at the elimination of the parasite or the elimination of the disease. The two goals are not identical: only people who carry a significant number of worms in their intestines suffer from consequences of their infection. Those who carry only a limited number of worms—often the great majority of an infected population—can infect others but do not themselves suffer any serious harm. Moreover, they often stay infected without developing a symptomatic disease. If one wishes to eliminate the parasite (that is, to reduce its regional presence to an insignificant level), it is necessary to test all people in an infected area and then treat all those who have hookworm eggs in their faeces. Such a ‘parasite-oriented’ approach efficiently prevents re-infection, but it forces people who feel perfectly well to accept unpleasant and occasionally dangerous therapy in the form of purgative substances (Stiles 1909). The alternative is a ‘handicap-oriented’ approach: to treat only people harmed by the parasite. People who suffer from the debilitating effects of hookworm infection have a direct interest in being treated and can be more easily persuaded to accept treatment. With a ‘handicap-oriented’ approach in which only symptomatic people are tested, diagnosis involves not only detecting whether a given person is infected, but also a semi-quantitative evaluation of the severity of the hookworm infection through an estimation of the number of eggs per gram of faecal material. Only people heavily infested by the worm receive an anti-hookworm treatment. Typically, handicap-oriented approaches are coupled with sanitary education, the construction of latrines, encouragement of people to wear shoes, and sometimes a supply of funds to purchase shoes, especially for children. Educational activities include teaching people about the insidious effects of hookworm infection: for example, stunted growth and intellectual development in children and chronic fatigue, which is often attributed to other causes.
The Rockefeller Hookworm Commission, active in the American South in the 1910s, chose a ‘handicap-oriented’ approach that preferred the voluntary treatment of symptomatic parasite carriers and sanitary education (Fosdick 1989) over enforced population treatment. Colonial rule, by contrast, favoured a coercive ‘parasite-oriented’ approach. The anti-hookworm campaign conducted in 1914–1916 by the Rockefeller Foundation (RF) in West India (Trinidad and British Guyana), small territories under colonial rule, was focused on the elimination of the parasite.[1] The goal of the ‘parasite-oriented’ intensive method was to ensure that all the parasite carriers were identified and treated. The first step involved the drawing of a precise map of the area where the eradication campaign was to take place and the collection of information on the number of people in each locality (Howard 1919, 20). The area was then divided into ‘intervention zones’. Each zone was covered by an ‘intervention group’ composed of a physician, two clerks, two ‘microscopists’ (laboratory technicians), 12 male nurses (on horseback), and one or two manual workers. The RF experts calculated that each ‘intervention group’ could provide anti-helminthic treatment for approximately two thousand people; the intervention territory included roughly that number of infected people (Howard 1919, 53–55). Nurses then distributed to everybody in the intervention zone receptacles for faeces. The next day, they collected the faeces samples and brought them to the laboratory. All the individuals diagnosed as parasite carriers were then visited again by nurses and given an anti-helminthic treatment, which they had to swallow in the nurses’ presence. The absolute rule was that every infected individual had to be treated (Howard 1919, 107–108). The ‘task force’ would then move to the next intervention area. The secret of the efficacy of this campaign was the strict codification and rationalisation of the tasks (inspired by Taylorism), the rigid timetable utilised, the careful tracing of interventions through a systematic collection of data on specially designed forms, and the close supervision of interventions in the field by the campaign’s organisers. The RF experts claimed that the West India campaign was highly successful, and attributed this success to the firm support of the British colonial administration and the mobilisation of local elites. They did not say what the hookworm carriers (including the symptom-free individuals who, in all probability, like Mary Mallon, had considered themselves healthy) thought about being forced into unpleasant treatment.
While, as a rule, hookworm is found in warm regions, in cooler climates this parasite had found an ecological niche in the hot and humid micro-environments of carbon mines. In the 19th century, the poor conditions of mines and hygiene of miners favoured the rapid propagation of infection among miners. In the late 19th and early 20th centuries, ‘miner’s anaemia’ was seen as a major professional risk and a serious public health threat. In the German region of Westphalia, mine-owners followed the ‘parasite-oriented’ approach to deal with this threat. In 1900, the government of Westphalia adopted an ordinance that proclaimed that only hookworm-free people could be hired to work in a mine. If a hookworm infestation was discovered in a given mine, all the miners had to be tested, and those found positive had to undergo an anti-helminthic therapy. They were allowed to return to work only when a laboratory declared them parasite-free. Miners’ unions found these rules harsh and arbitrary. Union activists claimed that only 6.5% of the miners who receive anti-parasitic treatment had shown the clinical symptoms of hookworm. The new rule forced symptom-free parasite carriers to undergo an unpleasant and risky treatment. Moreover, the treatment frequently failed, and the affected miners had to follow repeated cycles of therapy; they suffered from both the side effects of the drugs and the economic consequences of unemployment. In 1904, socialist members of the Reichstag protested against the compulsory treatment of asymptomatic hookworm carriers. The majority of the German experts argued, however, that a total ban on parasite carriers was the only way to end chronic infestation of mines by hookworm. They also claimed that complaints about the inefficacy and risks of the anti-helminthic therapy were exaggerated. Only 1.5% of infected people were ‘resistant’ to anti-hookworm drugs and thus needed three or four cycles of treatment (Fuester 1905), while severe accidents linked with this treatment were very rare. In 1905, the miners’ unions accepted the principle of the stringent surveillance of hookworm infection among miners, but successfully negotiated generous financial compensations for miners who ceased their work to undergo anti-parasite treatment (ibid.).
In Northern France, Albert Calmette and his colleagues from the Lille Pasteur Institute, in close collaboration with the local miners’ unions, elected a ‘handicap-oriented’ approach grounded in the voluntary acceptance of anti-hookworm measures (Calmette and Breton 1905). The unions negotiated improvements in the sanitary conditions in the mines and the installation of latrines, showers, and changing rooms at the mine’s entrance, and promoted the development of miner dispensaries (at that time, French workers, unlike their German counterparts, did not have access to state-sponsored health insurance). Union activists, together with sanitarians, also promoted hygiene education and encouraged miners, especially those who displayed symptoms of hookworm infection, to get tested. Infected miners were invited to receive anti-helminthic treatment. According to Calmette’s description, such miners spent a day in the miners’ infirmary [dispensaire d’hygiène sociale], where they were put into a clean bed; made to feel spoiled; given a dose of an anti-helminthic drug; and, at end of the day, received a nice meal. When they expelled the worms, they and other people present in the infirmary were invited to look at the parasites. The sight of fat worms bloated with ingested blood, Calmette explained, usually strongly impressed the miners. It boosted their willingness to follow hygiene rules and to spread these rules among their comrades (Calmette and Breton 1905, 137). It seems that both the rigid German method, which focused on the elimination of parasites, and the flexible French method, which focused on the elimination of handicap cases, were effective, especially when coupled—in both countries—with general hygiene improvements in the mines. In the 1910s, ‘miners’ anaemia’ became rare in France and Germany. And, one may add, in both countries, trade unions (of social-democratic inspiration in Germany and anarchist inspiration in the north of France) played a central role in the collective negotiations on the best way to balance the individual rights of asymptomatic carriers of parasites with those of mine owners.
Asymptomatic HIV infection: Public health and stigma
If typhoid was associated with to urban poverty and dirt and hookworm with rural ‘backwardness’, AIDS, which was initially presented as a disease of male homosexuals and drug addicts, can be said to have been strongly associated with deviant behaviour. Moreover, unlike typhoid, hookworm, and COVID-19, the control of AIDS is not linked to the introduction of hygienic measures. Another important difference between AIDS and the other three diseases is the absence of ‘truly asymptomatic’ carriers of pathogens. Long-term carriers of typhoid bacilli, such as Mary Mallon, or people who carry a small load of hookworm, can remain healthy for their entire lives while still being able to infect others. By contrast, if untreated, HIV-infected individuals nearly always develop full-fledged AIDS. The stigma associated with AIDS was a direct continuation of the stigmatisation of other sexually transmitted diseases.
Specific categories of people, above all female sex workers and ‘promiscuous women’, were for a long time accused of the propagation of venereal diseases (Corbin 1978; Brandt 1987). Proof of infection was not necessary for such an accusation to be made; suspicion of ‘immorality’ was sufficient. In the 19th and early 20th centuries, women seen as displaying loose sexual behaviour could be detained for ‘vagrancy’, a practice that culminated with the detention of women suspected of spreading syphilis in ‘rapid treatment centres’ in the US during the Second World War. In these centres, women who tested positive for syphilis (on an unreliable test) were forced to undergo treatment with arsenicals, a therapy that was neither rapid nor risk-free (Parascandola 2009). The widespread detention and isolation of US women suspected of being carriers of venereal diseases did not prevent, however, the dramatic increase in the prevalence of these pathologies during the Second World War (Brandt 1986).
The development of penicillin put an end to the quarantine of putative syphilis spreaders. However, widespread fear of hidden propagators of venereal diseases reappeared in the 1980s with the AIDS pandemic. The story of ‘patient zero’, a homosexual Canadian flight attendant named Gaetan Dugas, illustrates the concentrated fears of and apprehensions surrounding hidden disease spreaders. Randy Shilts bestselling 1987 book, And the Band Played On, described Dugas, the presumed ‘patient 0’ who started the AIDS epidemic in California, as a sinister individual who had hidden the symptoms of his disease and deliberately infected a great number of sexual contacts. Dugas was explicitly presented as the late 20th-century version of Typhoid Mary. This is an apt comparison. Both ‘Typhoid Mary’ and ‘Typhoid Marvin’, as Dugas was dubbed by one journalist, were mythical creatures produced by the media. As historian Richard McKay has shown, much of what was said about Dugas was fabricated (2017). Dugas was not listed in epidemiological records as ‘patient zero’—that is, as the person supposedly at the origin of the Californian outbreak—but as ‘patient O’, for ‘outside the state’. The zero was a transcription error; Dugas was not seen as responsible for bringing AIDS to California and he did not deliberately hide the fact that he had AIDS. At first, he was not aware of it and, later on, he was in denial and refused to accept that he had the deadly disease.
Dugas was diagnosed with a cancer, Kaposi’s sarcoma, in 1980, before this cancer was associated with AIDS (or, rather, with GRID—‘gay-related immunodeficiency’, as the mysterious disease that appeared among homosexual men and intravenous drug users in 1981 was then called). He saw himself as a cancer patient who had undergone chemotherapy and thus as an individual affected by a non-transmissible pathology. In 1982, doctors started to link Kaposi’s sarcoma with GRID, but the link was not universally accepted. Dugas elected to deny that he had GRID, the equivalent of a death sentence, and maintained the hope that he would one day be cured. Throughout 1982, he continued to work as a flight attendant and had numerous sexual contacts. When, in 1983, his health deteriorated and he was obliged to stop working, Dugas returned to Canada—first to Vancouver and then to his family home in Quebec City, where he died in 1984 (McKay 2014; 2017). After his death, authors such as Shilts (but also Mirko Grmek, the author of the first history of AIDS) took Dugas’s story out of the context of the very limited understanding of AIDS in the early 1980s and linked it to the mythical suspicion of vengeful transmission of disease by infected people, a story that frequently accompanied narratives of past epidemics (Grmek 1993, 19).
Gaetan Dugas died before the development, in 1985, of a blood test that detected anti-HIV antibodies in the blood. The introduction of this test did not eliminate the stigma linked with this pathology, but it did radically change the understanding of the natural history of AIDS. It made visible the existence of a long gap, which can last several years, between HIV infection and the appearance of the clinical disease AIDS. During the invisible infection period, infected people, usually unaware of their HIV-positive status, can infect others. Testing for HIV was rapidly introduced so as to make blood and blood products safe. In addition, selected categories of people, such as hospitalised patients and some healthcare workers, were systematically tested for HIV to reduce the risk of contamination in hospitals. In the US, there was also pressure to broaden HIV testing to, for example, people seeking residency in the US as well as international travellers (Brandt 1990): selected US states, such as Illinois and Louisiana, even introduced mandatory prenuptial screening for HIV in the late 1980s. This regulation was strongly criticised by some public health experts, who pointed to the high probability of false positives in populations with a very low prevalence of HIV infection (Cleary et al. 1987; Brandt 1988). Moreover, many countries introduced mandatory screening for AIDS for migrants and international travellers, a policy again criticised by some experts as repressive and inefficient (Gostin et al. 1990).
In North America and Europe, a few conservative politicians and public health experts proposed going much further by, for example, promoting mandatory universal HIV testing. One US columnist even proposed to tattoo the buttocks and forearms of all seropositive individuals as a warning to those who might want have sex or share needles with such individuals (see Brandt 1986, 236). Opponents of mandatory testing argued that, in the absence of an efficient treatment, the only ethically acceptable position was to propose voluntary screening programmes for people who wanted to know what their status was and a voluntary sexual-contact-notification programme for HIV-positive people (Brandt 1990). The situation would change dramatically with the development of an effective therapy for AIDS, especially if such a therapy was more successful when initiated during the early stages of a given HIV infection. This indeed happened in the mid-1990s, when the development of antiretroviral drugs (ARVs) led to the large extension of testing for HIV.
The proposal to introduce mandatory testing for HIV—either for the general population or, more often, specific ‘risk groups’ such as men who have sex with men or sex workers—was not implemented in Europe or North America. One of the main obstacles in the way of mandatory testing regimes for ‘risk groups’ was the question of who the members of these groups actually were: for example, numerous men who define themselves as heterosexuals occasionally have sex with men. In contrast, Cuba introduced such testing in 1986. HIV-positive individuals were isolated in sanatoriums, mainly to prevent them from having sex or exchanging needles with non-infected people. Moreover, if an HIV-positive woman was pregnant, she was required to have an abortion. Living conditions in sanatoria for HIV-infected people were good—in fact, better than those of the average Cuban—and interned people had access to state-of-the-art medical care. On the other hand, they were cut off from the external world, had limited rights to receive visits, and what visits were allowed were closely supervised to prevent sexual relations occurring between visitors and inmates. In the early 1990s, some inmates of these sanatoria expressed their despair at being left to wait for death in an institution. The situation of HIV-positive people in Cuba dramatically changed, however, with the development of anti-retroviral treatments. The government ended the obligatory internment of HIV-positive people and provided them with free treatment. The new policy was coupled with the widespread provision of education about AIDS, the free distribution of condoms, the multiplication of clinics that provided testing for HIV, and a strong incitation—according to some, even, a pressuring incitation—for people at risk to be tested (Anderson 2009). As a result, Cuba has had a very low number of deaths from AIDS. Fewer than 2,500 people died from AIDS in Cuba in the first 30 years of the epidemic, as compared with over 78,000 thousand AIDS deaths in New York, a city with a population roughly of Cuba’s size. Cuba’s experience with AIDS was seen by some as exemplary, by others as reprehensible, and by others still as somewhere between those two extremes (Scheper-Hughes 1993; McNeil 2012).
The three examples—of asymptomatic carriers of typhoid bacilli, hookworms, and HIV (during AIDS’s long pre-symptomatic phase)—illustrate, each in its own way, the situated dilemmas of finding the right balance between individual and collective rights and the decisive input of social, cultural, economic, and political considerations in negotiating such a balance. Dilemmas linked to the detection of asymptomatic carriers of SARS-CoV2 during the current COVID-19 pandemic have not been different, but the very nature of the pandemic foregrounds the role of situated socio-cultural variables.
COVID-19: Asymptomatic carriers and uncertainty
The debate about asymptomatic carriers of COVID-19 began at the very beginning of the pandemic. On 20 January 2020, the Chinese authorities confirmed human-to-human transmission of the new coronavirus. An article published in The Lancet on 24 January mentioned the possibility of symptom-free carriers of this virus (Chan et al. 2020). The same day, a group of Japanese researchers led by Hiroshi Nishiura published an article in The Journal of Clinical Research (Nishiura, Jung, et al. 2020) grounded in an analysis of Chinese-language publications on the new ‘atypical pneumonia’. They stated that, in many cases, Wuhan doctors were unable to trace the source of infection of the new coronavirus, a possible indication of a widespread ‘silent’ transmission of this pathogen (ibid.). On 29 January 2020, a report on the spread of this virus in Wuhan, published in The New England Journal of Medicine (NEJM), confirmed that, indeed, in a significant number of cases it was not possible to trace the origin of the infection (Chan et al. 2020; Li, Guan, et al. 2020). On 27 January, a UK information site, Science Media, interrogated a panel of leading UK specialists about risks of an ‘invisible’ spread of the new virus (Woolhouse et al. 2020). The panellists discussed more specifically an article published in Chinese on the 26 January, which reported the case of a symptom-free individual who travelled from Wuhan to Hangzhou for a conference. Several participants at that conference developed an ‘atypical pneumonia’ and tested PCR-positive for the new coronavirus. The participant from Wuhan, who was also PCR-positive, remained symptom-free during his stay in Hangzhou, but became ill two days after his return to Wuhan (Joseph 2020). The UK panellists explained that they did not have yet sufficient data to ascertain whether the new coronavirus could be spread by symptom-free people, but they agreed that if that were the case then it was a very worrisome development indeed—it would mean that it would be extremely difficult to control the new coronavirus’s worldwide propagation (Woolhouse et al. 2020).
On 13 February 2020, Nishuira and his colleagues, who were studying COVID-19 infections among Japanese citizens repatriated from Wuhan, reported that nearly half of the infected—and infecting—individuals were asymptomatic. The presence of numerous ‘invisible’ cases of a highly contagious virus, they stated, greatly complicated attempts to control the new disease (Nishiura, Kobayashi, et al. 2020). Japanese public health authorities immediately acted on this information. They banned travel from abroad, imposed severe quarantine on the small number of Japanese people allowed to return to the country, and barred all public gatherings. They also strongly recommended the generalisation of the use of face masks and a drastic reduction of interpersonal contact. This rapid action was later seen as one of the main reasons for the efficient containment of COVID-19 in Japan (Mesmer and Pons 2020). Western countries were much slower to enact similar measures.
Two weeks earlier, on 30 January, a group of German researchers described in a letter to the NEJM a cluster of coronavirus infections in Munich. A Chinese businesswoman from Shanghai had visited Germany from 19–22 January, and on 20 and 21 January met with a colleague from Munich. Her German contact developed a sore throat and fever on 24 January; three days later, he felt much better and returned to work. The Chinese woman did not report any health problems while in Germany, but became sick after returning to China. On 26 January, she tested positive for the new coronavirus; her employers transmitted this information to her professional contacts in China and Germany. The German colleague she had met tested positive for the new coronavirus, as did three of his co-workers. The four PCR-positive people were admitted to an infectious disease unit in a Munich hospital for isolation and monitoring. All developed mild cases of the disease, although the first patient continued to shed high quantities of the virus in sputum after his recovery. In their letter to the NEJM, the Munich researchers explicitly warned their colleagues about the dangers of COVID-19 asymptomatic transmission (Rothe et al. 2020).
At first, the Munich study was seen as a straightforward confirmation of earlier observations made by Chinese researchers. The director of the US National Institute of Allergy and Infectious Diseases (NIAID), Anthony Fauci, declared, ‘There’s no doubt after reading the New England Journal of Medicine paper that asymptomatic transmission is occurring. This study lays the question to rest’ (quoted in Kupferschmidt 2020). But the credibility of this claim was rapidly destabilised by an emerging professional dispute. A group of researchers at the Robert Koch Institute in Berlin was also in the process of publishing a report on the first coronavirus cases in Germany, but the Munich group was quicker and only their text was published. The Berlin group then wrote a letter to the NEJM protesting that the Munich group’s conclusions were inaccurate; the Munich group’s text claimed the Chinese businesswoman at the origin of the German outbreak displayed symptoms of coronavirus infection only after her return to China. However, the Berlin group claimed they had spoken to her on the phone and found that she had felt unwell during her stay in Germany, but had attributed this to jetlag. The Munich researchers did a sloppy job by failing to interview their index case. One may argue that the Chinese businesswoman still could have been described as ‘asymptomatic’ because, when she met her German colleague, she did not believe that she was sick and did not display typical signs of coronavirus infection. The story might have remained a minor squabble among competing professionals, but that was not the case. On 3 February, the journal Science published an article with the ominous title, ‘Study Claiming New Coronavirus Can Be Transmitted by People without Symptoms was Flawed’, quoting experts who severely criticised the study of the Munich group (Kupferschmidt 2020).
In June 2020, a New York Times investigation team presented the controversy as a crucial turning point. The conflict, the New York Times argued, deflected attention from the possibility of apparently healthy people disseminating the virus and consequently enabled the invisible spread of COVID-19 in Europe and the USA in February and early March (Apuzzo, Gebrekidan, and Kilpatrick 2020). Such a view may be an overstatement. The controversy surrounding the NEJM publication might have contributed to a delay in recognising the spread of the coronavirus by symptom-free people, but it was probably not the only cause for such a delay. The Munich group’s ‘proof’ that the virus could be transmitted by an apparently healthy individual may have been seen as insufficient evidence that this could occur frequently. It is, after all, possible to believe that the interpretation provided by the authors of the letter to the NEJM was correct while still holding the comforting view that the Munich case was an atypical event. In February and March 2020, the World Health Organization (WHO), the European Centre for Disease Prevention and Control (ECDC), and the health ministries of several European countries maintained that COVID-19 was diffused only by symptomatic individuals. For instance, in late January, the French health ministry widely distributed an information poster about the new coronavirus that boldly affirmed, ‘An individual is infectious only when symptomatic. No symptoms = No risk of contagion’ (reproduced in Maad 2020; translation by the author). The conviction that only symptomatic individuals could spread the new coronavirus was reassuring because it implied that the new coronavirus was a ‘Chinese problem’ that could be contained without having to take drastic and unpopular steps. An additional important element that might have contributed to the reluctance of health authorities in Europe and North America to recognise the danger of the spread of COVID-19 by symptom-free carriers was the then-current scarcity of face masks and, especially, diagnostic tests. Large-scale testing is vital to halting the diffusion of a pathology by symptom-free individuals, but many countries had limited supplies of diagnostic tests for SARS-Cov2 and were unwilling or unable to hike up their testing capacity (Beaudevin et al. this issue).
In March 2020, Italy, France, Spain, the UK, and the US suddenly discovered the alarming scale of the silent spread of COVID-19, especially in regions such as eastern France and northern Italy. Several later studies have shown that symptom-free individuals played an important role in the spread of COVID-19 (Ye et al. 2020; Qiu 2020). Some of these symptom-free COVID-19 carriers were probably ‘truly asymptomatic’—the young woman from Anyang infected in Wuhan in early January 2020, for example—while others were probably ‘pre-symptomatic’ or ‘weakly symptomatic’, like the Chinese businesswoman who visited Munich in late January. Sometimes, the boundary between these categories remained blurred, the more so because CT scans of people classified as ‘truly asymptomatic’ occasionally revealed lung anomalies, as was the case with the symptom-free child in the Shenzhen family cluster (Chan et al. 2020; Long et al. 2020). One widely publicised case involved members of a choir in Seattle who, in March, were massively infected by COVID-19 during a rehearsal. Their infection was initially presented as a result of asymptomatic transmission, because all choir members stated that they were perfectly well when they participated in that ‘super-spreading’ event (Read 2020). A later investigation found, however, that one choir member had indeed had slight flu-like symptoms. On the other hand, there is no formal proof that they were at the origin of this cluster of COVID-19 infections (Hamner et al. 2020).
In spring 2020, studies of the kinetics of SARS-CoV2 by infected persons confirmed not only that secretion of the virus precedes the appearance of disease symptoms but, worse, that such secretion peaks just before or just after the appearance of symptoms (He et al. 2020; Ganyani et al. 2020). By summer 2020, many specialists agreed that, on average, between 40 and 50% of infected (or, to be more precise, PCR-positive) individuals were symptom-free (Oran and Topol 2020a), although in December 2020 it was still not clear how many of those were truly asymptomatic throughout the course of their infection and how many were paucisymptomatic (i.e., subclinical), presymptomatic (i.e., would go on to develop symptoms later), or post-infection (i.e., with viral RNA fragments still detectable from an earlier infection) (Pollock and Lancaster 2020). At that time, however, experts were not sure whether ‘truly asymptomatic’ carriers played an important role in spreading COVID-19 (Lai et al. 2020; Li, Pei, et al. 2020). On 8 June 2020, Dr Maria Van Kerkhove, head of the WHO’s emerging diseases and zoonosis unit, stated at a news briefing in Geneva that the spread of the coronavirus by asymptomatic people appeared to be ‘very rare’ (WHO 2020). Following strong protests by numerous epidemiologists, the WHO experts declared that Van Kerkhove’s statement had been a misunderstanding and that the precise risk of transmission of SARS-CoV2 by asymptomatic individuals remained unknown (Mandavilly 2020; Oran and Topol 2020b; Meyerowitz et al. 2020). In early January 2021, scientists concluded on the basis of a meta-analysis of the available data and modelling that transmission by asymptomatic people—or, to be more precise, by people who did not display any of the clinical symptoms of COVID-19 when they infected others—were responsible for 59% of COVID-19 infections, meaning that, therefore, ‘measures such as wearing masks, hand hygiene, social distancing, and strategic testing of people who are not ill will be foundational to slowing the spread of COVID-19’ (Johansson et al. 2021, 1). Japanese researchers and public health authorities had arrived at the same conclusion almost a year earlier, in early February 2020 (Nishiura, Kobayashi, et al. 2020); they also took immediately efficient steps to contain the asymptomatic spread of COVID-19 by testing, tracing, and isolating contacts (TTI), an approach which is much easier to implement when the number of cases and contacts is low.
Ending notes: Pathogen carriers, unmasked and masked
Diagnostic tests can reduce the uncertainty pandemics cause, but cannot eliminate it entirely (Street and Kelly 2020; Comfort 2020). The meaning of a positive test result is impossible to dissociate from the wider socio-technical, legal, cultural, and political networks in which it is embedded. Tests can be thus be described as belonging to the domain of ‘trans-science’—that is, of questions which can be asked of science and yet which cannot be answered by science alone (Eyal 2019).
Testing for COVID-19 is important for confirming diagnosis but more important still for public health reasons. A minority of scientists (led by Professors Jay Bhattacharya of Stanford University, Sunetra Gupta of the University of Oxford, and Martin Kulldorff of Harvard University) in early October 2020 wrote up the ‘Great Barrington Declaration’, which advocated for a ‘handicap-oriented’ approach that did not involve the search for invisible carriers of the coronavirus. These scientists proposed focusing exclusively on the protection of vulnerable individuals, such as older people and those with health problems that increased their vulnerability to the virus, and suggested refraining from measures that limit the freedom of movement and association of low-risk individuals on the grounds that such measures hamper the development of immunity against COVID-19 in wider populations (Kulldorff et al. 2020). Their proposal met with the strong opposition of the majority of recognised experts, who pointed out the practical impossibility of identifying and protecting all vulnerable people (up to 30% of the population in some countries); the high human cost of this approach; the uncertainty as to whether/when a sufficient level of protective immunity would be achieved in a given population (for example, antibody studies indicated that the majority of the population of Manaus, Brazil came into contact with SAS-CoV2, but the mortality from COVID-19 in this city remained high [Buss et al. 2021]); and the risk that a high level of COVID-19 circulation would enable the rise of dangerous mutations (Alwar et al. 2020). It is not surprising that the control of SARS-Cov2 remained grounded in ‘pathogen-centred’ approaches.
Two models for managing COVID-19 risk through the control of the circulation of the virus co-existed in 2020: eradication and containment. Each model entails very different technological, social, and political choices. Countries that adopt the eradication model wish to eliminate SARS-CoV2 from their territory. To achieve this goal, they need to diagnose—that is, unmask—all the pre-symptomatic/ asymptomatic carriers of SARS-CoV2 present on the national territory, then ensure that they will not contaminate others by isolating them until they test negative for the virus. An eradication campaign implies zero tolerance of carriers of pathogens, be they mosquitoes or humans. As one of the main promoters of the disease eradication model in the 1950s, Fred Soper, put it, ‘Any is too many’ (Stepan 2011). Countries like China, South Korea, and New Zealand have sought to eradicate COVID-19 and are willing to take drastic steps to achieve this goal. When, in May 2020—two months after the city was declared COVID-free—a few cases of COVID-19 were detected in Wuhan, the city authorities decided to screen all its inhabitants (approximately ten million people) for SARS-CoV2 using the ‘classical’ PCR test (Davidson 2020). In June, New Zealand started an intensive search for every single contact of the two visitors who brought back SARS-Cov2 to the coronavirus-free island (Graham-Harrison 2020).
The often-praised South Korean model for eradicating COVID-19 assumes that asymptomatic virus carriers are as dangerous as symptomatic people. It relies on intensive testing, aggressive contact tracing (including the use of security camera footage, credit card records, and GPS data from cell phones), and rigorous isolation of infected people and their contacts (Thibaud 2020). Individuals who test positive for SARS-CoV-19, whether symptomatic or not, are isolated in special centres, while all their contacts are obliged to self-isolate at home for two weeks under strict electronic surveillance. Those who transgress the isolation rules face heavy fines and can be sent to prison. This aggressive and intrusive version of TTI—testing, tracing, and isolating—has been effective. In late February 2020, South Korea had several thousand cases of COVID-19; experts estimate that, at that time, several Western countries had a similar number of COVID-19 infections. But, while health authorities in countries like France, Spain, Italy, or the UK were unaware of the extent of the silent spread of the new coronavirus, widespread testing allowed South Korean health authorities to collect accurate data on COVID-19 propagation and then act swiftly to stop it (Fisher and Sang-Hun 2020; Fisher and Taub 2020; Thibaut 2020).
Countries that aim to contain COVID-19 have a more modest goal. They seek to test all symptomatic people, their close contacts, and selected ‘at-risk’ groups, but recognise that it is not technically possible to ‘unmask’ all the symptom-free carriers of SARS-CoV2. The eradication strategy is similar everywhere, but the definition of how many asymptomatic SARS-CoV2 carriers are ‘tolerable’ and how searches for such carriers are organised depend on situated variables, such as the availability and sensitivity of diagnostic tests; the priority given to the prevention of viral spread by specific groups of people, such as caretakers in nursing homes, students in university lodgings, or healthcare and services workers; and the capacity to ensure the isolation of PCR-positive people. It also relies on an additional element: the generalisation of the use of face masks. Estimates of the precise level of protection provided by face masks still vary, but, in summer 2020, experts agreed that the wide-scale adoption of masks helped to halt the spread of COVID-19, mainly by preventing infected people, especially those who believed they were healthy, from contaminating others (Stutt et al. 2020). Some countries, mostly but not exclusively in Asia, have energetically promoted the use of face masks by the general public. In South Asia, wearing a face mask during an outbreak of a respiratory disease is seen as a symbol of a shared condition and a mutual obligation to protect the wider community. A mask is a sign that anybody can be contaminated and can contaminate others, and a refusal to wear one is perceived as a selfish act and a transgression of a social norm (Baehr 2005). In Japan, where from February 2020 onwards the sanitary authorities have assumed that SARS-CoV2 is highly contagious, spreads through aerosols, and is often transmitted by asymptomatic carriers, the effort to control this virus has not aimed to detect all infected people (i.e., Japan did not rely on intensive COVID-19 testing) but has relied instead on a prohibition of ‘super-spreading’ events, the reduction of interpersonal contact among members of the public, and an immediate generalisation of the wearing of masks (Normille 2020; Economist Staff 2020).
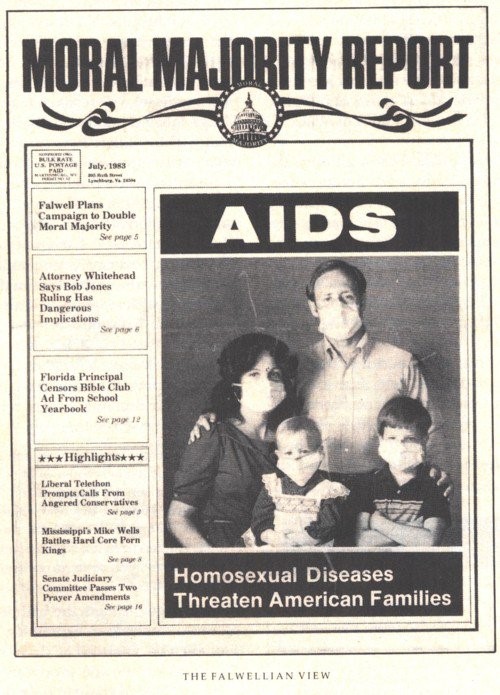
Face masks are less well accepted in other countries, such as the US, where some individuals believe that the obligation to wear a face mask in public is a violation of their rights and categorically reject the argument that their rejection of face masks puts others in danger (Gutierres 2020). A reluctance to recognise one’s potential responsibility in the dissemination of dangerous pathogens resonates with a long tradition of stigmatising ‘pestilence spreaders’, itself revived in the late 20th century in the context of the AIDS epidemic. In the early 1980s, at the height of the AIDS panic, public opinion turned against the presumed propagators of the new plague. The cover of the July 1983 issue of Jerry Falwell’s Moral Majority Report featured a photo of a typical American, white, middle-class family—a father, a mother, and two young children—with their faces covered by surgical masks. Beneath them ran the headline, ‘Homosexual Diseases Threaten American Families’ (Hoppe 2017, 41). ‘Homosexual diseases’ stands for homosexuals—that is, polluted deviants that threaten ‘normal’, clean, heterosexual Americans. In 2021, a photograph of a family wearing face masks is a perfectly banal sight, and it is not certain whether this image, originally meant to produce a visual shock and promote fear, would be recognised as being 38 years old. On the other hand, people seen as propagators of dangerous diseases continue to be stigmatised, a phenomenon recently observed during the COVID-19 pandemic: for example, people shunned nurses and care workers or ostracized individuals who recovered from COVID-19 (see, e.g., Bagcchi 2020).
Epidemics are frightening, and so are invisible—or ‘masked’—carriers of pathogens. Their ‘unmasking’ by a diagnostic test is often presented as an essential step towards eliminating a threat. Such a view may promote the stigmatisation and ostracism of pathogen carriers and hamper efforts meant to persuade actual or potential spreaders of disease to adopt behaviour which minimises the risk to others. It does not have to be so. Efforts to contain epidemics can be grounded in solidarity in the face of a common danger, while asymptomatic disease carriers can become important agents of the expansion of such solidarity. The ‘secret’ of success of COVID-19 containment measures in democratic countries such as Japan and South Korea, observers proposed, is twofold: firstly, trust in experts’ advice, and secondly, solidarity (Fisher and Taub 2020; Thibault 2020). The South Korean approach, grounded in the national effort to supress SARS-CoV2, and the Japanese approach, grounded in a tolerance of low levels of circulation of the virus coupled with a non-repressive hindering of its diffusion, were both efficient. The spread of COVID-19 is an amorphous target: it is affected by changes in the virus itself; the ‘COVID fatigue’ of populations; and the speed of vaccine distribution and vaccine efficiency, especially in terms of blocking the transmission of COVID-19 and its ability to slow the spread of coronavirus mutants. Now, in the summer of 2021, neither the South Korean or Japanese approaches to the control of COVID-19 seem quite as exemplary, but the data for 2020 should not be ignored. The mortality rate per million for 2020 was 17 for South Korea and 26 for Japan; on the other hand, it was 1,123 for the UK, 1,070 the US, and 910 for France (Johns Hopkins University & Medicine 2020).
Calmette and his colleagues mobilised miners from hookworm-affected communities to promote hygiene and healthy habits among their comrades. AIDS activists who advocated for testing, safe sex, and the safe use of injectable drugs were often HIV-positive. One can imagine Mary Mallon might also have followed a similar path. During her second quarantine on the North Brother Island, she worked as a laboratory assistant and was reported to be very proud of this job (Leavitt 1997). If, instead of being transformed into an icon of pestilence, Mallon had been given the opportunity to participate in the promotion of sanitary measures—that is, had she lived in a society that trusted and supported poor, migrant, working-class women—she could have become a symbol of responsible behaviour and care for others.
About the author
Ilana Löwy is a senior researcher emerita at the Institut national de la santé et de la recherche médicale (INSERM), Paris. Trained as a biologist, she then retrained as a historian of science and medicine. Her research mainly concerns the past and present relationships between laboratory sciences, clinical medicine, and public health. She has studied the history of microbiology, tropical medicine, oncology, and reproductive medicine. Her interest in diagnosis is grounded in studies of female malignant tumours (see her books, Preventive Strikes: Women, Precancer and Prophylactic Surgery [Johns Hopkins University Press, 2009] and A Woman's Disease: A History of Cervical Cancer [Oxford University Press, 2011]), research on prenatal diagnosis (see Imperfect Pregnancies: A History of Birth Defects and Prenatal Diagnosis [Johns Hopkins University Press, 2017] and Tangled Diagnoses, Women, Prenatal Testing and Risk [Chicago University Press, 2018]); and an ongoing investigation of Zika epidemics in Brazil.
Footnotes
-
It may, however, have also been also accompanied by educational efforts: posters, leaflets, press campaigns, and interventions in schools.↩︎
References
Alwan, Nisreen A., Rochelle Ann Burgess, Simon Ashworth, Rupert Beale, Nahid Bhadelia, Debby Bogaert, Jennifer Dowd, et al. 2020. ‘Scientific Consensus on the COVID-19 Pandemic: We Need to Act Now’. The Lancet 396 (10260): E71–E72. https://doi.org/10.1016/S0140-6736(20)32153-X.
Anderson Roy, Christophe Fraser, Azra Ghani, Christl Donnelly, Steven Riley, Neil M. Ferguson, Gabriel Leung, et al. 2004. ‘Epidemiology, Transmission Dynamics and Control of SARS: the 2002–2003 Epidemic’. Philosophical Transactions of the Royal Society B 359 (1447): 1091–1105. https://doi.org/10.1098/rstb.2004.1490.
Anderson, Warwick. 1995. ‘Excremental Colonialism: Public Health and the Poetics of Pollution’. Critical Inquiry 21 (3): 640–669. https://www.jstor.org/stable/1343940.
Anderson, Tim. 2009. ‘HIV/AIDS in Cuba: Lessons and Challenges’. Revista Panamericana de Salud Pública 26 (1): 78–86. https://doi.org/10.1590/s1020-49892009000700012.
Apuzzo, Matt, Selam Gebrekidan, and David Kirkpatrick. 2020. ‘How the World Missed Covid-19’s Silent Spread’. The New York Times. Web. June 27. https://www.nytimes.com/2020/06/27/world/europe/coronavirus-spread-asymptomatic.html.
Baehr, Peter. 2005. ‘Social Extremity, Communities of Fate and the Sociology of SARS’. Archives of European Sociology 46: 179–221. https://doi.org/10.1017/S000397560500007X.
Bagcchi, Sanjeet. 2020. ‘Stigma during the COVID-19 Pandemic’. The Lancet Infectious Diseases 20 (7): 782. https://doi.org/10.1016/S1473-3099(20)30498-9.
Bai, Yan, Lingsheng Yao, Tao Wei, Fei Tian, Dong-Yan Jin, Lijuan Chen, and Meiyun Wang. 2020. ‘Presumed Asymptomatic Carrier Transmission of COVID-19’. JAMA 323 (14): 1406–1407. https://doi.org/10.1001/jama.2020.2565.
Beaudevin, Claire, Luc Berlivet, Soraya Boudia, Catherine Bourgain, Maurice Cassier, Jean-Paul Gaudillière, and Ilana Löwy. 2021. ‘“Test, Test, Test!” Scarcity, Tinkering, and Testing Policy early in the COVID-19 Epidemic in France’. Medicine Anthropology Theory 8 (2): 1–31. https://doi.org/10.17157/mat.8.2.5116.
Bourdain, Anthony. 2005. Typhoid Mary. New York City, NY: Bloomsbury.
Brandt, Allan. 1990. ‘Sexually Transmitted Disease: Shadow on the Land, Revisited’. Annals of Internal Medicine 112 (7): 481–483. https://doi.org/10.7326/0003-4819-112-7-481.
Brandt, Allan. 1986. ‘AIDS: From Social History to Social Policy’. Law, Medicine and Health Care 14 (5–6): 231–242. https://doi.org/10.1111/j.1748-720X.1986.tb00990.x.
Brandt, Allan. 1987. No Magic Bullet: A Social History of Venereal Infections in the United States Since 1880. New York City, NY: Oxford University Press.
Brandt, Allan. 1988. ‘The Syphilis Epidemic and Its Relation to AIDS’. Science 239 (4838): 375–380. https://doi.org/10.1126/science.3276007.
Brown, Phil. 1995. ‘Naming and Framing: The Social Construction of Diagnosis and Illness’. Journal of Health and Social Behavior: S34–S52. https://doi.org/10.2307/2626956.
Buss, Lewis, Carlos Prete Jr., Claudia Abrahim, Alfredo Mendrone, and Tassila Salomon. 2021. ‘Three-Quarters Attack Rate of SARS-CoV-2 in the Brazilian Amazon During a Largely Unmitigated Epidemic’. Science 371 (6526): 288–292. https://doi.org/10.1126/science.abe9728.
Calmette, Albert and Michel Breton. 1905. L'Ankylostomiase maladie sociale (anémie des mineurs): biologie, clinique, traitement, prophylaxie. Paris: Masson et Cia.
Chan, Jasper Fuk-Woo, Shuofeng Yuan, Kin-Hang Kok, Kelvin Kai-Wang, Hin Chu, Jin Wang, Fanfan Xing, et al. 2020. ‘Familial Cluster of Pneumonia Associated With the 2019 Novel Coronavirus Indicating Person-to-Person Transmission: A Study of a Family Cluster’. The Lancet 395 (10223): 514–523. https://doi.org/10.1016/S0140-6736(20)30154-9.
Cleary, Paul, Michael Barry, Kenneth Mayer, Allan Brandt, Larry Gostin, and Harvey Fineberg. 1987. ‘Compulsory Premarital Screening for the Human Immunodeficiency Virus’. JAMA 258 (13): 1757–1762. https://doi.org/10.1001/jama.1987.03400130071036.
Comfort, Nathaniel, 2020. ‘Confronting the Next Stage of Coronavirus Means Accepting Uncertainty in Science’. Philadelphia Inquirer. Web. 24 June. https://www.inquirer.com/opinion/commentary/coronavirus-pandemic-end-endemic-disease-scientist-predictions-20200624.html.
Corbin, Alan. 1978. Les filles de noces. Misère sexuelle et prostitution au XIX siècle. Paris: Aubier.
Davidson, Helen. 2020. ‘10 Days of Battle: Wuhan Draws up Ambitious COVID-19 Testing Plan’. The Guardian. Web. 13 May. https://www.theguardian.com/world/2020/may/13/10-days-battle-wuhan-covid-19-testing-plan.
Economist Staff. 2020. ‘The Japanese Authorities Understood COVID-19 Better Than Most’. The Economist. Web. 12 December. https://www.economist.com/asia/2020/12/12/the-japanese-authorities-understood-covid-19-better-than-most.
Enserink, Martin. 2003. ‘SARS: A Pandemic Prevented’. Science 302 (5653): 2045. https://doi.org/10.1126/science.302.5653.2045.
Ettling, John. 1981. The Germ of Laziness: Rockefeller Philanthropy and Public Health in the New South. Cambridge, MA: Harvard University Press.
Eyal, Gil. 2019. ‘Trans-Science as a Vocation’. Journal of Classical Sociology 19 (3): 254–274. https://doi.org/10.1177/1468795X19851377.
Fang, Fang. 2020. Wuhan Diary: Dispatches from a Quarantined City. New York City, NY: Harper Collins.
Fisher, Max, and Choe Sang-Hun. 2020. ‘How South Korea Flattened the Curve’. New York Times. Web. 24 March. https://www.nytimes.com/2020/03/23/world/asia/coronavirus-south-korea-flatten-curve.html.
Fisher, Max, and Amada Taub. 2020. ‘The Last Coronavirus Taboo.’ The Interpreter Newsletter. Newsletter. 14 May.
Fosdick, Raymond. 1989. The History of the Rockefeller Foundation. New Brunswick, NJ: Transaction Publishers.
Fuester, Ernst. 1905. ‘Les étapes de la lutte contre l’ankylostomiase en Allemagne’. Calmette, Albert, and Michel Breton, eds. L'ankylostomiase maladie sociale (anémie des mineurs): biologie, clinique, traitement, prophylaxie. Paris: Masson et Cia. 175–201.
Ganyani, Tapiwa, Cécile Kremer, Dongxuan Chen, Andrea Toneri, Christian Faes, Jacco Wallinga, and Niels Hens. 2020. ‘Estimating the Generation Interval for Coronavirus Disease (COVID-19) Based on Symptom Onset Data, March 2020’. Eurosurveillance 25 (17). https://doi.org/10.2807/1560-7917.ES.2020.25.17.2000257.
Gostin, Larry, Paul Cleary, Kenneth Mayer, Allan Brandt, and Eva Chittenden. 1990. ‘Screening Immigrants and International Travelers for the Human Immunodeficiency Virus’. New England Journal of Medicine 322 (24): 1743–1746. https://doi.org/10.1056/NEJM199006143222411.
Graham-Harrison, Emma. 2020. ‘COVID-19 Outbreaks in New Zealand and China Highlight Stark Choices’. The Guardian. Web. 17 June. https://www.theguardian.com/world/2020/jun/16/outbreaks-in-beijing-and-new-zealand-highlight-perils-of-relaxing-rules.
Grmek, Mirko. 1993. History of AIDS Emergence and Origins of Modern Pandemics. Princeton, NJ: Princeton University Press.
Gutierrez, Melody. 2020. ‘Anti-Vaccine Activists, Mask Opponents Target Public Health Officials—At Their Homes’. Los Angeles Times. Web. 18 June. https://www.latimes.com/california/story/2020-06-18/anti-mask-protesters-target-county-health-officers.
Hamlin, Christopher. 1990. A Science of Impurity: Water Analysis in Nineteenth Century Britain. Berkeley, CA: University of California Press.
Hamner, Lea, Polly Dubbel, Ian Capron, Andy Ross, Amber Jordan, Jacon Lee, Joanne Lynn, et al. 2020. ‘High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice—Skagit County, Washington, March 2020’. Morbidity and Mortality Weekly Report 69 (19): 606–610. https://dx.doi.org/10.15585/mmwr.mm6919e6.
Hardy, Anne. 2015. Salmonella Infections, Networks of Knowledge, and Public Health in Britain, 1880–1975. Oxford: Oxford University Press.
He, Xi, Eric Lau, Peng Wu, Xilong Deng, Jain Wang, Xinxin Hao, Yiu Chung Lau, et al. 2020. ‘Temporal Dynamics in Viral Shedding and Transmissibility of COVID-19’. Nature Medicine 26: 672–675. http://doi.org/10.1038/s41591-020-0869-5.
Heymann, David. 2004. ‘The International Response to the Outbreak of SARS in 2003’. Philosophical Transactions of Royal Society B 359 (1447): 1127–1129. https://doi.org/10.1098/rstb.2004.1484.
Hoppe, Trevor. 2017. Punishing Disease: HIV and the Criminalization of Sickness. Berkeley, CA: University of California Press.
Howard, Hector H. 1919. The Control of Hookworm Disease by the Intensive Method. New York City, NY: The Rockefeller Foundation-International Health Board.
Johansson, Michael, Talia Quandelacy, Sarah Kada, Pragati Venkata Prasad, Molly Steele, John Brooks, Rachel Slayton, et al. 2021. ‘SARS-CoV-2 Transmission from People Without COVID-19 Symptoms’. JAMA Open 4 (1): e2035057. https://doi.org/10.1001/jamanetworkopen.2020.35057.
Juttel, Annemarie, and Sarah Nettleton. 2011. ‘Towards a Sociology of Diagnosis: Reflections and Opportunities’. Social Science and Medicine 73 (6): 793–800. https://doi.org/10.1016/j.socscimed.2011.07.014.
Johns Hopkins University & Medicine. 2020. ‘Cumulative Data for 2020’. Coronavirus Resource Center. Web. https://coronavirus.jhu.edu/.
Joseph, Andrew. 2002. ‘New Coronavirus Can Cause Infections with No Symptoms and Sicken Otherwise Healthy People, Studies Show’. STAT News. Web. 24 January. https://www.statnews.com/2020/01/24/coronavirus-infections-no-symptoms-lancet-studies/.
Kulldorff, Martin, Sunetra Gupta, and Jay Bhattacharya. 2020. ‘The Great Barrington Declaration’. Web. 4 October. https://gbdeclaration.org/.
Kupferschmidt, Kai. 2020. ‘Study Claiming New Coronavirus Can Be Transmitted by People Without Symptoms Was Flawed’. Science. Web. 3 February. https://www.sciencemag.org/news/2020/02/paper-non-symptomatic-patient-transmitting-coronavirus-wrong.
Lai, Chih-Cheng, Yen-Hung Liu, Cheng-Yi Wang, Ya-Hui Wang, Shun-Chung Hsueh, Muh-Yen yen, Wen-Chien Ko, et al. 2020. ‘Asymptomatic Carrier State, Acute Respiratory Disease, and Pneumonia Due to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Facts and Myths’. Journal of Microbiology, Immunology and Infection 53 (3): 404–412. https://doi.org/10.1016/j.jmii.2020.02.012.
Latour, Bruno, 1988. The Pasteurisation of France. Cambridge, MA: Harvard University Press.
Lawrence, Christopher. 1985. ‘Incommunicable Knowledge: Science, Technology and the Clinical Art in Britain 1850–1914’. Journal of Contemporary History 20 (4): 503–520. https://doi.org/10.1177/002200948502000402.
Leavitt, Judith W. 1992. ‘“Typhoid Mary” Strikes Back. Bacteriological Theory and Practice in Early Twentieth-Century Public Health’. Isis 83 (4): 608–629. https://doi.org/10.1086/356292.
Leavitt, Judith W. 1997. Typhoid Mary: Captive to Public Health. Boston, MA: Beacon Press.
Li, Qun, Xuhua Guan, Peng Wu, Xiaoye Wang, Lei Zhou, Yeqing Tong, Ruiqui Ren, et al. 2020. ‘Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia’. New England Journal of Medicine 382 (13): 1199-1207. https://doi.org/10.1056/NEJMoa2001316.
Li, Ruiyun, Sen Pei, Bin Chen, Yimeng Song, Tao Zhang, Wan Yang, and Jeffrey Shaman. 2020. ‘Substantial Undocumented Infection Facilitates the Rapid Dissemination of Novel Coronavirus (SARS-CoV2)’. Science 368 (6490): 489–493. https://doi.org/10.1016/j.ijid.2020.03.020.
Long, Quan-Xin, Xiao-Jun Tang, Qiu-Lin Sh, Quin Li, Hai-Jun Deng, Jun Yuan, Je-Li Hu, et al. 2020. ‘Clinical and Immunological Assessment of Asymptomatic SARS-CoV-2 Infections’. Nature Medicine 26: 1200–1204. http://doi.org/10.1038/s41591-020-0965-6.
Loss, Adolf. 1905. The Anatomy and the Life History of Ankylostoma duodenale: A Monograph. London: Records of the School of Medicine.
Löwy, Ilana. 1994. ‘On Hybridizations, Networks and New Disciplines: The Pasteur Institute and the Development of Microbiology in France.’ Studies in the History and Philosophy of Science 25 (5): 655–688. http://doi.org/10.1016/0039-3681(94)90035-3.
Löwy, Ilana. 2015. ‘Les Microbes’. Raj, Kapil and Otto Sibum (eds). Histoire des Sciences et des Savoirs vol. 2: Modernité et globalisation. Paris: Seuil. 223–242.
Löwy, Ilana. 2020. ‘The Unknown Known: The SARS Past of COVID-19’. Medical Anthropology Quarterly. Web. 5 June. https://medanthroquarterly.org/rapid-response/2020/06/the-unknown-known-the-sars-past-of-covid-19/.
Maad, Asma, 2020. ‘Coronavirus : une affiche du ministère écarte trop vite le risque de contagion lors de l’incubation’. Le Monde. Web. 6 February. https://www.lemonde.fr/les-decodeurs/article/2020/02/06/coronavirus-une-affiche-du-ministere-ecarte-trop-vite-le-risque-de-contagion-lors-de-l-incubation_6028658_4355770.html.
MacDonald, Betty. 1948. The Plague and I. Philadelphia, PA: J. B. Lippincott & Co.
Mandavilli, Apporva. 2020. ‘In the W.H.O.’s Coronavirus Stumbles, Some Scientists See a Pattern’. New York Times. Web. 9 June. https://www.nytimes.com/2020/06/09/health/coronavirus-asymptomatic-world-health-organization.html.
McKay, Richard. 2014. ‘“Patient Zero”: The Absence of a Patient's View of the Early North American AIDS Epidemic’. Bulletin of the History of Medicine 88 (1): 161–194. https://doi.org/10.1353/bhm.2014.0005.
McKay, Richard. 2017. Patient Zero and the Making of the AIDS Epidemics. Chicago, IL: Chicago University Press.
McNeil, Donald. 2012. ‘A Regime’s Tight Grip on AIDS’. New York Times. Web. 7 May. https://www.nytimes.com/2012/05/08/health/a-regimes-tight-grip-lessons-from-cuba-in-aids-control.html.
Mendelsohn, Andrew. 1995. ‘“Typhoid Mary” Strikes Again: The Social and the Scientific in the Making of Modern Public Health’. Isis 86 (2): 268–277. http://doi.org/10.1086/357156.
Mendelsohn, Andrew. 1998. ‘From Eradication to Equilibrium: How Epidemics Became Complex after World War I’. Lawrence, Christopher, and George Weisz (eds). Greater than the Parts: Holism in Biomedicine, 1920–1950. Oxford: Oxford University Press. 303–332.
Mesmer, Philippe, and Philippe Pons. 2020. ‘Lutte contre le COVID-19 : les leçons sud-coréenne et japonaise’. Le Monde. Web. 29 October. https://www.lemonde.fr/idees/article/2020/10/19/lutte-contre-le-covid-19-les-lecons-sud-coreenne-et-japonaise_6056519_3232.html.
Meyerowitz, Eric, Aaron Richterman, Isaac Bogoch, Nicola Low, and Muge Cevik. 2020. ‘Towards an Accurate and Systematic Characterisation of Persistently Asymptomatic Infection with SARS-CoV-2’. The Lancet Infectious Diseases. Web. 7 December. https://doi.org/10.1016/S1473-3099(20)30837-9.
Nishiura, Hiroshi, Sung-mok Jung, Natalie Linton, Rio Kinoshita, Yichi Yand, Katsuma Hayashi, Tetsuro Kobayashi, et al. 2020. ‘Editorial: The Extent of Transmission of Novel Coronavirus in Wuhan, China, 2020’. Journal of Clinical Medicine 9 (2): 330. https://doi.org/10.3390/jcm9020330.
Nishiura, Hiroshi, Tetsuro Kobayashi, Takeshi Miyama, Ayako Suzuki, Sung-mok Jung, Katsuma Hyashi, Rio Kinoshita, et al. 2020. ‘Estimation of the Asymptomatic Ratio of Novel Coronavirus Infections (COVID-19)’. International Journal of Infectious Diseases 94: 154–155. https://doi.org/10.1016/j.ijid.2020.03.020.
Normille, Denis. 2020. ‘Japan Ends Its COVID-19 State of Emergency’. Science Magazine. Web. 26 May. https://www.sciencemag.org/news/2020/05/japan-ends-its-COVID-19-state-emergency
Oran, Daniel, and Eric Topol. 2020a. ‘Opinion: Lots of Us Are Infected by the Coronavirus—and Don’t Know It. Here’s What That Means’. Washington Post. Web. 11 June. https://www.washingtonpost.com/opinions/2020/06/11/how-find-out-whether-asymptomatic-covid-19-carriers-are-infectious/.
Oran, Daniel, and Eric Topol. 2020b. ‘Prevalence of Asymptomatic SARS-CoV-2 Infection. A Narrative Review’. Annals of Internal Medicine 173 (5): 362–367. https://doi.org/10.7326/M20-3012.
Parascandola, John. 2009. ‘Quarantining Women: Venereal Disease Rapid Treatment Centers in World War II America’. Bulletin of the History of Medicine 83 (3): 431–459. https://doi.org/10.1353/bhm.0.0267.
Pollock, Allyson, and James Lancaster. 2020. ‘Asymptomatic Transmission of Covid-19’. British Medical Journal 371: m4851. https://doi.org/10.1136/bmj.m4851.
Qiu, Jane. 2020. ‘Covert Coronavirus Infections Could Be Seeding New Outbreaks’. Nature News. Web. 20 March. https://www.nature.com/articles/d41586-020-00822-x.
Read, Richard. 2020. ‘A Choir Decided to Go Ahead with Rehearsal. Now Dozens of Members Have COVID-19 And Two Are Dead’. Los Angeles Times. Web. 29 March. https://www.latimes.com/world-nation/story/2020-03-29/coronavirus-choir-outbreak.
Rosenberg, Charles E. 2002. ‘The Tyranny of Diagnosis: Specific Entities and Individual Experience’. Milbank Quarterly 80 (2): 238–260. https://doi.org/10.1111/1468-0009.t01-1-00003.
Rothe, Camilla, Mirjam Schunk, Peter Sothmann, Gisela Bretzel, Guenter Froeschl, Claudia Wallrauch, Thorbjörn Zimmer, et al. 2020. ‘Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany’. New England Journal of Medicine 382: 970–971. https://doi.org/10.1056/NEJMc2001468.
Scheper-Hughes, Nancy. 1993. ‘AIDS, Public Health and Human Rights in Cuba’. The Lancet 342 (8877): 965–967. https://doi.org/10.1016/0140-6736(93)92006-f.
Steere-Williams, Jacob. 2020. ‘A “Menace” or a Martyr to the Public’s Health?’ Isis 111 (4): 818–821. https://doi.org/10.1086/712254.
Stepan, Nancy Leys. 2011. Eradication: Ridding the World of Diseases Forever? Ithaca, NY: Cornell University Press.
Stiles, Wardell. 1909. ‘The Treatment of Hookworm Disease’. Public Health Reports 24 (34): 1191–1193. https://doi.org/10.2307/4563571.
Street, Alice, and Ann Kelly. 2020. ‘Counting Coronavirus: Delivering Diagnostic Certainty in a Global Emergency’. Somatosphere. Web. 6 March. http://somatosphere.net/forumpost/counting-coronavirus-diagnostic-certainty-global-emergency/.
Sturdy, Steve, and Roger Cooter. 1998. ‘Science, Scientific Management, and the Transformation of Medicine in Britain c. 1870–1950’. History of Science 36 (4): 421–466. https://doi.org/10.1177/007327539803600402.
Stutt, Richard, Renata Retkute, Michael Bradley, Christopher Gilligan, and John Colvin. 2020. ‘A Modelling Framework to Assess the Likely Effectiveness of Facemasks in Combination With “Lock-Down” in Managing the COVID-19 Pandemic’. Proceedings of the Royal Society A 476 (2238). https://doi.org/10.1098/rspa.2020.0376.
Thibault, Harlod. 2020. ‘COVID-19 : comment une traque méthodique et intrusive a permis à la Corée du Sud de maîtriser le virus’. Le Monde. Web. 20 December. https://www.lemonde.fr/planete/article/2020/12/08/covid-19-comment-une-traque-methodique-et-intrusive-a-permis-a-la-coree-du-sud-de-maitriser-le-virus_6062564_3244.html.
Tomes, Nancy. 1998. The Gospel of Germs: Men, Women, and the Microbe in American Life. Cambridge, MA: Harvard University Press.
WHO. 2020. Covid-19: Virtual Press Conference. Transcript. 8 June. https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-08jun2020.pdf?sfvrsn=f6fd460a_0
Woolhouse, Mark, Bill Keevil, David Heymann, Jonathal Ball, Shiela Bird, Wendy Barclay, Michael Head, et al. 2020. ‘Expert Reaction to News Reports That the China Coronavirus May Spread Before Symptoms Show’. Science Media. Web. 27 January. https://www.sciencemediacentre.org/expert-reaction-to-news-reports-that-the-china-coronavirus-may-spread-before-symptoms-show/.
Worboys, Michael. 2000. Spreading Germs: Disease Theories and Medical Practice in Britain, 1865–1900. Cambridge: Cambridge University Press.
Ye, Feng, Shicai Xu, Zhihua Rong, Ronghua Xu, Xiaowei Liu, Pingfu Deng, Hail Liu, et al. 2020. ‘Delivery of Infection from Asymptomatic Carriers of COVID-19 in a Familial Cluster’. International Journal of Infectious Diseases 94: 133–138. http://doi.org/10.1016/j.ijid.2020.03.042.
You, Verna. 2020. ‘Hero Who Told the Truth: Chinese Rage Over Coronavirus Death of Whistleblower Doctor’. The Guardian. Web. 7 February. https://www.theguardian.com/global-development/2020/feb/07/coronavirus-chinese-rage-death-whistleblower-doctor-li-wenliang.