This article follows the introduction of COVID-19 polymerase chain reaction (PCR) diagnostic tests in France. It shows how, at the intersection of science, medicine, politics, and policy-making, the test, trace, and isolate (TTI) strategy played out during the first months of the pandemic against a backcloth of multiple shortages. In so doing, the authors move beyond trite explanations (such as ‘French publ i c health’s backwardness’) to highlight how successive policy inflections affected the national response to the pandemic. The piece analyses the shifting French political discourse surrounding (scarce) COVID-19 tests while exploring ad-hoc regulations and guidelines as well as the intense ‘bricolage’ that they triggered in the field of clinical medicine. The authors contend that the limitations of the testing infrastructure in France during the first half of 2020 shaped the decision to resort to lockdown. The research article sheds light on two coexisting registers of professional uses of reverse transcription-polymerase chain reaction (RT-PCR) assays—a ‘public health use’ and a ‘clinical use’—and highlights the chang i ng political and social relevance of these two registers, with scarcity as a major determinant of these changes. One of the striking aspects of the introduction of COVID-19 tests in France therefore lies in the enduring gap between the dynamics of the epidemic and the dynamics of testing. In this respect, the French situation is neither extreme nor unique, which makes this case study a relevant basis for the international comparison of testing practices in different phases of the COVID-19 pandemic.
'Test, test, test!'
Scarcity, tinkering, and testing policy early in the COVID-19 epidemic in France
—
Abstract
Introduction
‘Test, test, test!’ has already become a defining byword of the COVID-19 pandemic, which, as we finalise this research article in May 2021, is far from over. Initially, this plea was merely one of the ‘opening remarks’ of Tedros Adhanom Ghebreyesus, director general of the World Health Organization (WHO), at a media briefing on 16 March 2020—‘a simple message for all countries’, as he put it (World Health Organization 2020c). However, the repeated, insistent recommendation quickly captured imaginations and prompted a massive stream of comments at a time when the reluctance and/or inability of so many countries around the world to follow the WHO’s advice were becoming all too obvious.
The rapid development of the COVID-19 molecular diagnostic test in the first weeks of the pandemic made it possible for authorities such as the WHO to call for testing to become one of the core tools for controlling the disease throughout the world. However, as the epidemic spread from one continent to another, shortages of all sorts of necessary items quickly became apparent. For instance, there was a crucial lack of rapid transmission-polymerase chain reaction (RT-PCR) diagnostic tests, personal protective equipment (PPE) for healthcare workers, and regular masks for the public. In spite of claims that the scale of the need for medical goods was unforeseeable, exceeded normal production capabilities, and disrupted the markets for medical goods, this scarcity of vital items soon came to epitomise governmental failure in France and other countries alike.[1] During the first months of the pandemic, national testing capacities and strategies became widely regarded as the yardstick for states’ actions; they were the quantitative variable underlying most of the (in)formal world rankings that journalists, experts, and laypeople alike started to elaborate in late February and early March 2020. Tests were what France lacked; South Korea, Germany, and some middle-income countries such as Vietnam and Uruguay, however, were seemingly effortlessly scaling up their testing capacities.
France, a country proud of its healthcare system and convinced of its ability to deal with a pandemic,[2] provides us with a relevant case study to examine perceived public health failure in the midst of a global crisis. A peculiarity of the French situation is that, at the time of the first COVID-19 diagnoses in Paris and Bordeaux in January 2020, the Ministry of Health was finalising the rollback of most of the pandemic preparedness work undertaken by previous governments in the aftermath of several H5N1 flu epidemics and the 2003 SARS outbreak. The French government was carrying on with the destruction of (admittedly out of date) FFP2 masks[3] just at as Chinese authorities began to warn the world about a possible new epidemic. Moreover, when COVID-19 began to spread out of China, French public hospitals were engaged in a nation-wide social movement against another kind of scarcity: a shortage of beds and personnel. Repeated industrial actions had taken place during the previous year, prompted by the most recent of a series of organisational reforms implemented by successive governments over the previous decade. The French health context is shaped by the conjunction of its showcased publicly funded universal healthcare system and the neo-liberal policies that have repeatedly constrained health budgets and long neglected public health.
As a group of historians, sociologists, and anthropologists of medicine and science, our aim is to make sense of this French configuration in relation to the unfolding of COVID-19 testing. During the weeks that followed the 17 March lockdown, heated debates over testing policy raged, with a strong focus on perceived shortages throughout the country. Our contention is that the severe limitations of testing infrastructure in France in the first half of 2020 shaped the government’s choice of lockdown strategy. On this basis, we broaden the perspective and explore—mostly with regards to public healthcare institutions—the root causes and features of this dramatic configuration.
Carrying out an investigation under lockdown (until mid-May 2020) was a peculiar experience for we researchers. By limiting our mobility and access to potential field sites and interviewees, the sanitary situation in France strongly constrained our methodological choices. Deprived of the possibilities of ethnography and professional meetings, we worked from our respective homes and almost compulsively collected whatever data we could. As a result, we had to rely on two corpuses made of various snapshots which, when aggregated, painted the picture we explore in this research article. First, we performed a thorough analysis of the national press and of governmental and regulatory literature. The press was an important resource because of the high quality of the work of selected investigative journalists. We complemented this survey of available written material with a set of 26 targeted phone, videoconference, and, in a few cases, face-to-face interviews, conducted between March and June 2020. Our interviewees included public health experts, clinicians in hospitals and private practices, medical biology specialists, and industry personnel. In the media and in our interviews, we gathered key actors’ personal and official views on the unfolding of the pandemic in France. In so doing, we sought to analyse the shifting French political discourse surrounding (scarce) COVID-19 tests while exploring ad-hoc regulations and guidelines as well as the intense ‘bricolage’ they triggered in clinical medicine.
Our initial hypothesis was that the main event that shaped the shifts in French testing strategy was the scarcity of tests (i.e., the failure to account for tests’ various sociotechnical dimensions: reagents, machines, personnel, etc.). Our analysis shows that, although specific shortages certainly had major effects, they do not account for all of our observations. First and foremost, our investigation sheds light on the manifold social appropriations of diagnostic assays. It led us to differentiate between two registers of professional uses (that is, two sets of expectations and appropriations). The first, what we term the ‘public health use’ of COVID-19 tests, refers to the newly developed COVID-19 tests that rapidly emerged as essential but deeply imperfect public health tools. The initial ‘T’ of a three-pronged strategy—‘testing’—was the first necessary epidemiologically informed intervention, and was widely described as the only way to control the spread of the virus. Yet, biological assays also bear clinical significance for the person tested and the health professionals s/he might come into contact with, especially if the test is positive. It is important to stress that not all those who were diagnosed as ‘COVID-19 patients’ in France during the first months of the epidemic were duly tested. At that time, PCR assays were in extremely short supply. Still, diagnostic tests played (and still play) a key role in orienting the medical trajectory of those who display symptoms associated with COVID-19 (‘asymptomatic positives’ more rarely seek medical advice). We label this the ‘clinical use’ of COVID-19 tests.
In the face of this distinction, it is tempting to describe the social appropriation of COVID-19 tests as drawing a continuum between these two different categories of use. Yet, as we shall show, these use categories are not competing; if one prevailed over the other during certain phases of the pandemic in France, it was mainly due to three different factors: first, the series of enduring and often severe shortages in assays (PCR reagents), machines, and workforce; second, the institutional peculiarities of the French health system, which has for over a century been defined by the structural weakness of public health interventions and lack of investment (Picard 2003; Schneider 2003; Berlivet 2008); and third, a pronounced hospital tropism fuelled by the almost knee-jerk preference of French ‘medical mandarins’ and policymakers alike for ‘curative medicine’.
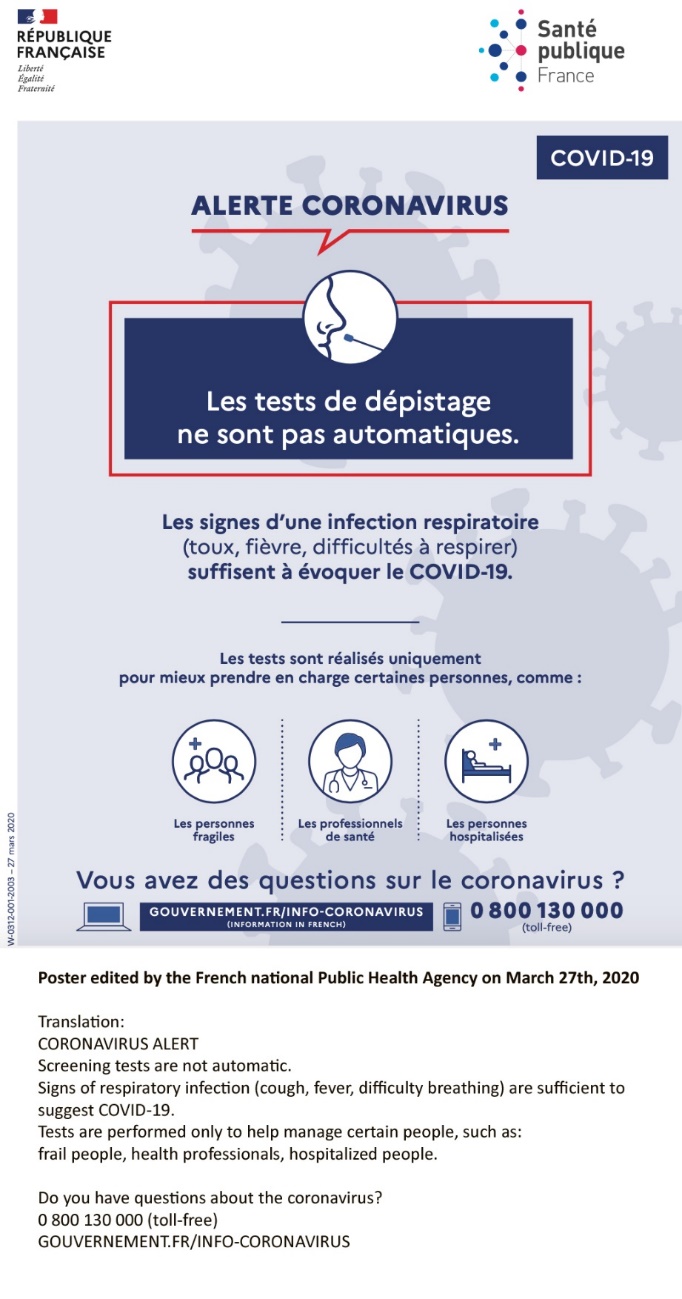 1. Poster edited by the French national Public Health Agency and published on 27 March 2020.
Translation: CORONAVIRUS ALERT / Screening tests are not automatic. / Signs of respiratory
infection (cough, fever, difficulty breathing) are sufficient to suggest COVID-19. / Tests
are performed only to help manage certain people, such as: frail people, health
professionals, hospitalized people. / Do you have questions about the coronavirus? / 0 800
130 000 (toll-free) / GOUVERNEMENT.FR/INFO-CORONAVIRUS.
1. Poster edited by the French national Public Health Agency and published on 27 March 2020.
Translation: CORONAVIRUS ALERT / Screening tests are not automatic. / Signs of respiratory
infection (cough, fever, difficulty breathing) are sufficient to suggest COVID-19. / Tests
are performed only to help manage certain people, such as: frail people, health
professionals, hospitalized people. / Do you have questions about the coronavirus? / 0 800
130 000 (toll-free) / GOUVERNEMENT.FR/INFO-CORONAVIRUS.
One can delineate three distinct phases of the COVID-19 crisis in France from late January to early June 2020. First, in January and early February, the number of tests required by health authorities was very low and clinicians were still struggling to comprehend the new disease, so tests were mostly used as a public health tool. The sanitary authorities were attuned to the danger of imported cases, and the limited testing capacity was used to prevent the development of clusters of COVID-19 in France. Then, during the second stage of the outbreak, which lasted roughly from early March to mid-April, the sanitary authorities were suddenly confronted with a massive surge in the number of COVID-19 cases and a rapid extension of the epidemic. When a strict lockdown started on 17 March, a radical shift occurred: France moved from a public health stance and systematic (not always efficient) efforts to trace COVID-19 contacts to the opposite pole. Not only were the contacts of infected people no longer tested, but the sanitary authorities went so far as to reject the systematic testing of people with typical COVID-19 symptoms.[4] The shortage of tests was obvious, even with the new, limited goal of limiting testing to people with severe symptoms. Yet the authorities were reluctant to include new actors, such as private laboratories, in the official testing scheme. Locally, hospitals were often able to overcome practical difficulties through creative improvisation and tinkering. By contrast, no testing whatsoever was offered in nursing/care homes, with devastating consequences. During the third period, which spanned from mid-April until mid-May, the number of COVID-19 cases gradually declined and, with it, the pressure on intensive care wards in heavily affected regions. In the context of the post-lockdown stage of the epidemic (then planned for 11 May 2020) and several public controversies, the French authorities launched an effort to significantly increase the country’s testing capacity while timidly acknowledging some potential mistakes. The government progressively introduced serological tests, and organised systematic tracing of COVID-19 cases and their contacts. Following a bumpy path, techniques and structures finally came into being in late May and early June. The declared aim of the new public health arrangements was to mend the test, trace, and isolate (TTI) strategy; uncover hidden loci of COVID-19; limit transmission; and, in the best case, handle a possible second wave of the disease without resorting to lockdown. These goals were barely achieved. The main explanation of this relative failure is not to be found in France’s testing capacity per se, but rather in organisational issues which affected the two less technical dimensions of the strategy (contact-tracing and self-isolation of both ‘positives’ and ‘contacts’).
This trajectory immediately points to a key feature of such biological assays: as crucial as they may be (if deemed reliable) in assessing individual status with regards to a specific disease, they are part of broader, more complex socio-technical networks. This is of course common to all technical objects. Yet this seemingly trivial assertion actually carries crucial implications for the case in point. The versatility of diagnostic tests, which in turn depends on the ability of social actors to include them in various socio-technical networks, explains the plurality of uses evidenced at different times during the health crisis (Juttel 2009; Street 2014; Hay Burgess, Wasserman, and Dahl 2006; Brown 1995). In this respect, the French situation is—in all probability—not unique, and we hope our detailed analysis allows for comparisons of the practical ways in which diversity of uses has operated in, first of all, East Asian countries, where the implementation of TTI appeared more decisive in reducing the transmission of SARS-Cov2. More specifically, we believe that our analysis, focused as it is on effects of scarcity on the conditions of test usage at macro and micro levels, will contribute to better understandings of the dynamics at work in complex organisational settings of complex systems under stress. Scarcity works both as an indicator of tensions/limitations/lacks and as a set of constraints that leads actors to develop alternative strategies.
Everything is under control: Surveillance of an imported disease
Initially all went well, or so it seemed at the time. The French health authorities first learned of the arrival of the ‘novel coronavirus’ (which would be named ‘SARS-CoV-2’ on 11 February) on national territory on 24 January 2020. A French national of Chinese origin who had flown back from Wuhan two days earlier and a couple of Chinese tourists originally from that same city were diagnosed with COVID-19 in Paris and Bordeaux (Bernard Stoecklin et al. 2020).
The full testing procedure of the biological samples (RNA extraction, real-time reverse transmission-polymerase chain reaction [RT-PCR] testing, virus isolation and titration) was undertaken at the National Reference Centre for Respiratory Infection Viruses, based at the Pasteur Institute in Paris (Lescure et al. 2020). The procedure used the sequence disclosed by the GISAID database, a collective tool created in 2006 during the H5N1 threat, in accordance with an assay protocol published by a group of virologists at the Berliner Charité Universitätsmedizin the previous week (more specifically, on 16 January), with the WHO’s endorsement (Corman et al. 2020). Between late January and mid-February, biologists at the Pasteur Institute added their own personal touch to the protocol by developing a real-time RT-PCR assay specifically for the RdRp gene (four targets). Their motivation seems simple: ‘They published their technique, but we also wanted to develop our own technique in parallel,’ commented Sylvie Behillil, deputy director of the National Reference Centre (CNR) for respiratory infection viruses at the Pasteur Institute on 30 January 2020 (Magenou 2020). The Pasteur protocol, which was endorsed and published by the WHO (World Health Organization 2020b), used the gene disclosed by the Berliner Charité as a confirmatory test for its own method.
The need for RT-PCR tests grew only slowly in the following weeks as few new cases were registered, and the sanitary control of the flights organised to repatriate French nationals from China seemed to have proven effective. It was only when infection clusters finally emerged in two small towns in the French Alps that the number of diagnostic tests needed by epidemiologists (who had been on alert since 10 January) to trace the dissemination of the virus in the community became more substantial. During this initial stage, tests were the first public health tools deployed and were a key element in the efforts to trace secondary transmissions in the community. However, because the authorities assumed that the disease could not be transmitted by symptom-free individuals, there was no call for widespread testing.
The structure of pandemic control in France involves a complex network of public institutions whose roles and jurisdictions have gone through repeated transformation over the past two decades. After the SARS epidemic (and the urging of the WHO, which since the 2000s had been pushing governments to develop preparedness strategies, the French government began pandemic planning in earnest. It took place under the guidance of an inter-ministerial committee established and initially chaired by Didier Houssin[5] (the Health Director-General from 2005 to 2011), but ran in conjunction with the General Secretariat for Defence and Security and involved almost every ministry, local authority, and professional branch. The first plan against pandemic flu, adopted in 2004, provided the backbone for the nation’s epidemic preparedness plan until the end of the decade. In 2009, however, the political scandal that followed the H1N1 episode, which targeted the ‘overreaction’ of the government and the health administration, led to a dramatic revision of its structure. The government of the time had massively invested in vaccines and personal protective equipment and, as H1N1’s transmission rate dropped rapidly, did not use them, leading to what was labelled a ‘waste of public money’.
The revised 2011 plan was therefore less proactive than its predecessor, leaving out public health measures that targeted the entire population (Secrétariat Général de la Défense et de la Sécurité Nationale 2011). The first phase of action focused on the surveillance of travellers, identifying cases based on clinical symptoms, and advising domestic isolation. The second phase aimed at limiting the circulation of people within the country and also relied on clinical diagnoses eventually confirmed in hospital virology laboratories. Contact tracing was mentioned but was not accompanied by a clear definition of how it should be organised. Beside the provision of antivirals and clinical interventions, the main public health measures envisioned were selective vaccination campaigns for the population at risk and the closure of day-care centres and schools. Testing was neither a priority nor a necessity within a framework based on the epidemiological features of the flu.
Two very different but complementary institutions were in charge of the critical work of disease control. First, the Direction des maladies infectieuses (DMI) [infectious diseases division] of Santé Publique France (SPF), the French public health agency established in 2016 and based on the model of Public Health England. The DMI is responsible for epidemiological surveillance and intervention all over the country, and can rely on a network of regional correspondents. Second, the Cellules de veille, d’alerte et de gestion sanitaires (CVAGS) [surveillance and crisis management units], which were established in each of the Agences régionales de santé [health regional agencies] (ARS),[6] carried out local investigations with the support, if not supervision, of SPF epidemiologists (Ilef 2011). The latter were central in the putative implementation of response plans known as ORSAN REB (Organisation de la réponse du système de santé en situations sanitaires exceptionnelles—risques epidémiologiques et biologiques), which were adopted in the context of mounting security issues after 2015 by the Ministry of Health. One of ORSAN’s key goals was to open communication channels between the different health actors: health managers, infectious and tropical disease services, emergency physicians, intensive care specialists, and paediatricians.
From a public health perspective, the role of these organisations was, however, limited. ARS, on the one hand, have, since their creation in 2009, been deeply engaged in the management and reorganisation of hospitals, aiming to increase productivity, reduce the number of beds, and reinforce ambulatory care. In many instances, preparation has been limited to the writing of local plans and the conduct of exercises dealing with the consequences of a terrorist attack. SPF, on the other hand, is a heterogeneous agency with little operational experience and resources; its main tasks have to do with epidemiological surveillance and health education campaigns. Compared to its US, British, and many European counterparts, the French surveillance and intervention apparatus is infamously undersized and underfunded while the whole national public health community remains both very small and politically subaltern (Berlivet 2008).
The weakness of operational capabilities and logistics within this public health landscape may be illustrated by the issue of mask provision for health personnel and the general population. A key aspect of preparedness lay in the constitution of a national health stockpile of masks, drugs, vaccines, and so on, in order that France might not depend on foreign suppliers like China. However, while the stock grew steadily until 2010, once it had exceeded one billion euros in value (including 250 million euros’ worth of masks alone), efforts started to wane. Criticism of the alleged overreaction of the government and public health administration to the 2010 H1N1 flu epidemic were taken up by successive governments to justify a sharp reduction in emergency funds. This, in turn, translated into a gradual depletion of public emergency supply stocks. The destruction and non-replacement of surgical masks and PPE, in particular, would later come back to haunt French politicians on both sides of the political spectrum.
In this early, pre-epidemic stage, French authorities nonetheless displayed a high level of confidence in their ability to cope with a possible health crisis. Drawing on their successful control of sporadic MERS infections, both the Minister of Health and various senior physicians made a number of speeches in which they underlined the high level of preparedness of the country in spite of the tensions in the hospital environment (to which we will later return). Everything suggested that France would face up to the situation thanks to past investments in epidemic preparedness, themselves prompted by a long series of past alerts: the 1997 and 2005 H5N1 influenza outbreaks, SARS in 2003, H1N1 in 2009, MERS in 2012, and Ebola in 2014.
In this initial configuration, diagnostic technologies were an element in a limited cluster management operation that went from interviewing COVID-19 patients about their activities during past days—to identify who they had been in contact with and assess their risk exposure—to ‘tracing’ these contacts, especially those at higher risk of exposure, and then to trying to talk them into ‘self-isolating’ for 14 days or, when they had severe symptoms, checking into a specialised reference hospital (ESR). The list of these 38 referral hospitals, spread across France’s territory, was established in 2012 (in the midst of the Middle East respiratory syndrome [MERS] outbreak) by the Ministry of Health. The role of these hospitals was subsequently extended to COVID-19.
‘When we have finished all the validation steps, we will be able to distribute this test to the various hospital laboratories that will be in charge of the patients and the samples taken from these patients,’[7] explained Vincent Enouf, deputy director of the CNR for Respiratory Infection Viruses at the Pasteur Institute, on 24 January (Frouville 2020). On 20 February, the Ministry of Health, under the responsibility of Olivier Véran, published a methodological guide on how to prepare for a possible COVID-19 epidemic (Ministère des solidarités et de la santé 2020b). The national strategy focused on the management of ‘suspect patients’:
The final classification of patients as ‘possible cases’ of COVID-19 was based on the ability to render a virology result with the highest possible reliability. The National Reference Centre (CNR) for respiratory viruses now has a specific test (RT-PCR) for the diagnosis of COVID-19 infection. This diagnostic technique is in the final stages of deployment within health institutions authorised for COVID-19 at the national level (Ministère des solidarités et de la santé 2020b, 22).
At this stage, not all of the 38 referral hospitals earmarked to treat COVID-19 had installed a test platform. When needed, they were asked to send their samples to the CNR laboratories in Paris and Lyon.
By the end of February, health services and many more public institutions were on alert, and although cluster control efforts by SPF epidemiologists and various ARS had not gone entirely smoothly,[8] it seemed that any consistent spread of the disease in the population had been avoided. Appearances were deceptive, though, for at the same time as the Minister of Health was praising the work of the ‘surveillance and intervention [epidemiological] apparatus’ during an interview on national radio (Véran 2020),[9] two disease outbreaks were already spiralling out of control.[10] The role played by RT-PCR tests in the COVID-19 epidemic was about to change dramatically, from a public health use to a clinical use.
The crisis at home: The trouble with testing
The critical days of late February and early March and the unexpected discovery of the extent of the asymptomatic spread of COVID-19 radically changed the perception of this disease as a foreign phenomenon that could be tackled with the targeted testing of people travelling from the affected regions (that is, China and, of far more concern, Northern Italy). This is well illustrated by the situation in Strasbourg, a city with the largest university hospital in the Grand-Est region and located close to Mulhouse, where massive contamination took place during a week-long religious event.
Strasbourg’s university hospital (CHU), a COVID-19 referral hospital with its own virology laboratory, developed a local testing protocol in collaboration with the Pasteur Institute during the second week of February (interview with a local infectiologist, 3 June). The virology lab completed its first reverse transmission-polymerase chain reaction (RT-PCR) diagnosis of COVID-19 on 25 February on a patient who had just returned from Lombardy in Italy. On 2 and 3 March, the number of calls to the infectious disease department via the emergency call centre escalated. According to our informants, the decision was made to set up a site to sample nasopharyngeal swabs for PCR testing, which started operating the next day. The situation nevertheless immediately got out of hand due to dozens of requests. By 6 March, two dozen patients had been admitted and the service for infectious diseases was already filled with COVID-19-affected patients. The newly created crisis unit decided to postpone all non-urgent and non-COVID activities, especially surgery, in order to make room for COVID-19-affected patients and allow for the creation of dedicated services, which by the end of March amounted to 12 units of 15 beds.
The testing operations seem to have been constrained for two different reasons. The most immediate was the infrastructure of the virology lab, which at that time had only one PCR machine with a maximum capacity of 100 tests per day. The second and less direct issue originated in the flow of admissions. By 6 March, the consensus in the crisis cell was already that it was necessary to keep all patients evaluated as ‘non-severe’ cases out of the hospital. Intermediate cases were kept for 24 hours so that pulmonary scans could be performed and respiratory needs evaluated. Under this combined pressure, a) the testing of patients at risk because of existing conditions (e.g., diabetes and cardiovascular diseases) who did not show acute COVID-19 symptoms was stopped and, b) the operations of the sampling centre were reorganised with an appointment system to collect a maximum of 150 swabs per day and avoid overwhelming the laboratory, which also had to handle samples from neighbouring hospitals, especially from the Mulhouse outbreak.
Testing in Strasbourg thus quickly lost its public health function. Contact tracing was stopped altogether, although the families of positive cases were still tested—but only when family members started to show symptoms. The activities of the virology laboratory were clearly focused on the clinical and hospital-oriented uses of the test, namely the diagnosis and confirmation of COVID-19 infections in patients with acute respiratory distress syndrome and, later, the reduction of iatrogenic risk to non-COVID patients.
A similar massive flow of COVID-19 patients to hospitals occurred in two other French regions: Hauts-de-France and Ile-de-France. During the last days of February, public health authorities started to reconsider the epidemiological situation, proclaiming that the circulation of the virus had reached epidemic proportions (Pascariello et al. 2020). Epidemiological phase 2 was declared on 28 February and phase 3, in which large-scale community transmission was acknowledged, was declared two weeks later on 14 March. As panic escalated within the Direction générale de la Santé [General Directorate for Health], the Haut Conseil de la santé publique [Higher Council for Public Health], and the Ministry of Health, the strategic meaning of testing was reconsidered along the same lines as in the hospitals facing a ‘tsunami’ (a word that by then was commonly used by medical professionals).
On 11 March, the Haut Conseil de la santé publique adopted national testing guidelines, which clearly stated that the testing of contacts and patients with mild symptoms had become unnecessary and was therefore no longer being considered. Accordingly, RT-PCR tests would be accessible only to hospital personnel and patients at high risk of severe symptoms—namely those over 70 or suffering from renal failure, cirrhosis, cardiovascular disorders, diabetes, severe obesity, lung diseases with breathing limitations, immunodeficiency, and pregnant women (Haut Conseil de la santé publique 2020). Triage and the prioritisation of patients either admitted to hospital or considered for admission became the norm, while cluster management lost its strategic meaning. As Jérôme Salomon, the directeur général de la Santé, explained in his daily press conference on the first day of lockdown, ‘When facing active, large-scale circulation of the virus, testing is no longer useful’ (Direction générale de la Santé 2020).
This claim contrasted with the recommendations of the World Health Organization (WHO) and was far from consensual. Many observers in the media challenged it, arguing that testing was perhaps difficult or impossible because of logistic problems, but was definitely not useless, as the example of Germany suggested. Interviewed on 18 March by a national public TV channel, Jean-François Delfraissy, the head of the government’s COVID-19 scientific advisory council, actually admitted that the strict prioritisation was grounded in scarcity:
Yes, the testing problem is a real problem. The aim of containment is to avoid or diminish contact. If they were available in very large quantities, the tests would in fact make it possible to test suspicious individuals and then isolate them from contact. This is therefore a major issue. If we did not choose this strategy in France, as was done in Korea, it is because we did not have the capacity, initially, to test a very large number of people. […] But, I want to be very clear: we are constantly working on the matter. We have a first stage, which is confinement, and we will have to get out of this confinement and under what conditions? We will have to use tests—and we will have them, by that stage—in a very broad, massive way, and eventually we will have a drug, a molecule, and we will be able to apply a ‘test and treat’ strategy (Delfraissy 2020).
With the arrival of the epidemic wave and lockdown measures, the new testing strategy, limited as it was to symptomatic and vulnerable people, came under fire from health and biology professionals working in private biology, veterinary, and public research laboratories outside the referral hospitals.
For instance, on 19 March, Laurent Lagrost, a senior researcher at the National Health Research Institute (INSERM), and Didier Payen, a physician at the Lariboisière Hospital in Paris, called for a massive screening programme, arguing for the mobilisation of university research laboratories equipped with PCR machines to complement the use of approved commercial kits. The geneticist and CNRS researcher Philippe Froguel blamed the ARS, which he considered an inefficient technical bureaucracy since they had rejected his and other researchers’ offers of service: ‘We lost perhaps fifteen days. We could have ordered reagents and that would have allowed us to do about 600 tests per day, when France does between 2,000 and 4,000 per day’ (Cherel and Cellule Investigation de Radio France 2020).
The situation at Pitié-Salpêtrière, one of the two reference hospitals in Paris, illustrates the ways in which some clinicians similarly tried to address what they called the uses of testing for ‘prevention’. As head of the department of infectious and tropical diseases, Eric Caumes had closely followed events in China. Up to the end of February, he was critical of what he considered an exaggerated reaction to the situation.
Renaud Piarroux, another specialist of infectious diseases at Pitié-Salpêtrière, is a microbiologist with extensive experience in global health. He has led missions in West Africa, and investigated and organised the response to the cholera outbreak after the 2010 earthquake in Haiti. Piarroux not only argued for more tests and discussed supply issues, but also pleaded for an integrated strategy of territorial surveillance, patient involvement, and testing. By April, he had won the support of the City of Paris and of Assistance publique–Hôpitaux de Paris (AP-HP), its consortium of university hospitals, to establish mobile units whose role mimicked the kind of epidemiological surveillance and community involvement activities his team had prioritised in Haiti. On national public radio, he declared:
The idea is to accompany the patient, to make an alliance with him. By finding out about his living conditions and sending teams to his home to see how to manage containment, to do screening around the patient and with his family to see how to limit the spread as much as possible. This is in the interests of the patient, who does not want to send his relatives to hospital. The day we manage to do this on the vast majority of patients, we will have a major impact on the epidemic. We have to isolate very quickly, look around the patient if there are no other infected people, and above all help them’ (Piarroux and Flahault 2020).
The controversy over the screening strategy in établissements hospitaliers pour personnes âgées dépendantes (EHPAD) [public and private nursing homes for the aged] reveals the deep contradictions underlying France’s lockdown strategy. On 30 March, the government’s COVID-19 scientific advisory council issued an opinion on the management of the epidemic in EHPADs, suggesting that their inmates were a ‘priority for the use of diagnostic and biological tests’—but was cautious—’depending on the availability of diagnostic tests, which should be directed as a priority to these institutions’. The question was all the more acute as France’s intensive care units were saturated and the issue of triaging admissions was overtly discussed. On 5 April, Galla Bridier, deputy mayor of Paris, ‘in charge of seniors and autonomy’ declared, ‘The SAMU [Service d’aide medicale d’urgence—a public emergency transportation service] can no longer take to hospital residents of EHPADs who are sick with coronavirus’ (Gairaud 2020).
In practice, testing of the elderly and EHPAD personnel was not organised centrally. When it took place, it was on the basis of local initiatives and alliances. For instance, on 25 March, Philippe Juvin, head of the emergency department at Georges Pompidou Hospital and mayor of La Garenne-Colombes, called for massive screening in retirement homes ‘to avoid deaths on a massive scale’. On 31 March, he organised the screening of all staff and residents of the town’s EHPAD, for which a private biology laboratory was mobilised (Bureau 2020). The Departmental Council of the Hauts-de-Seine, associated with two large private biology laboratories, echoed his initiative and on 16 April announced mass screening in 106 EHPADs and 42 state-run residences for senior citizens.
The scarcity of tests partly stemmed from the local impact of worldwide demand for swabs, PCR machines, kits, and reagents. France has limited industrial infrastructure for producing such goods and was therefore very sensitive to the mounting difficulty testing laboratories faced when importing these materials. However, in addition (and in contrast to Germany, whose biotech industry started to produce SARS-CoV-2 testing kits in January to meet both the Asian markets’ and the country’s demands), the multinational company bioMérieux, a powerful French industrial champion in medical diagnostics, favoured the more lucrative US market.
The company began developing several test technologies for coronavirus SARS-CoV-2 in January 2020 on the premises of two research and development and production sites in France (Grenoble in Auvergne-Rhône-Alpes and Verniolle in Occitanie) and one at Biofire in the United States (Salt Lake City, UT), a company it had acquired in 2014. Given that 90% of bioMérieux’s sales take place abroad, the hierarchy of the international and French markets was clear. The firm announced the release of two different tests in March. The Argene® SARS-CoV-2 R-GENE® test received a waiver from the French Agence nationale de sécurité du médicament (ANSM) on 19 March. The Centre national de référence des virus des infections respiratoires (CNR) validated it on 27 March and on 1 April, the French social security fund authorised its reimbursement. This kit, the only SARS-CoV-2 test produced in France (Reuters and Henri-Pierre André 2020), was not available before lockdown and reached the market only several weeks later. In contrast, the Biofire SARS-CoV-2 test, developed with the support of the US Department of Defense, received a marketing waiver from the US Food and Drug Administration (FDA) on 23 March. bioMérieux later announced that the tests produced in the US would first cover the needs of the US Department of Defense, then the US market, and finally the global market (bioMérieux 2020). The French CNR validated the Biofire test on 5 May.
National production thus faced two difficulties. First, the size of the US (and the international) market for the French company precluded massive investments in France before the pandemic. Second, as the crisis struck home, the lockdown measures and the erratic policy of the French health authorities resulted in an absence of incentives that could have made the domestic market more attractive.[11]
Scaling up to revive ‘preventive’ testing
One of the most influential collectives pushing for the rapid growth of testing capacity during lockdown was the Syndicat des jeunes biologistes médicaux (SJBM), a union of young medical biologists. This professional union is responsible for running private as well as public laboratories that conduct a wide range of biological analyses and tests in relation to medical practice. It was established in 2008 by a small group of medical interns, tenured hospital physicians, and private practitioners owning city labs. By 2014, the Ministry of Health recognised the SJBM as ‘representative’ of the profession.
The SJBM’s public campaigning against what they perceived as a state bureaucracy inhibiting civil society’s ability to mobilise and innovate started with lockdown. According to them, not only would it have been preferable to embrace the test, trace, and isolate (TTI) strategy, but there was also not a single good epidemiological motive for limiting testing, even under lockdown conditions. As the SBJM president, L. Barrand, explained to us:
We believe not that the DGS [Direction générale de la Santé] restrictions on testing aims and practice are the result of an evaluation of the sanitary situation to identify people at risk, but that targeting and limited testing are the consequences of the limited testing capabilities we have identified […] In France, our public health strategy adjusts to our logistical means, and not the reverse. Where South Korea does massive testing and targeted isolation, France does the opposite: massive quarantine and targeted testing’ (personal interview, 11 April).
The SJBM argued that the limited testing apparatuses available in France at the time was not the main cause of scarcity. Even if medical biologists all agreed that their number would have to increase, the key issue, in the SJBM’s view, was the shortage of both reagents and protective equipment for personnel. The scarcity of reagents (RNA extraction media and amplification kits in particular) was the consequence of market anarchy. On 11 April, Barrand told us:
Every single laboratory is now operating on its own. We all try to secure materials from our usual suppliers. For weeks, this has become increasingly difficult. The entire supply chain is facing a booming demand worldwide, while many factories have ceased or limited production. Delivery, when it happens, has become unpredictable.
For the organisation, however, the absence of state engagement and the lack of coordination of orders severely aggravated the problem. Barrand added:
There is no reserve stock and we depend on those made by the private suppliers. The governments of several European countries, beginning with Germany, set up national stocks they now make available to their laboratories. This did not happen in France. Testing platforms are therefore regularly facing shortages for days and have to outsource testing. We have the cars but we don’t have the gas to drive.
The SJBM campaign took a decisive turn late in March, when the union decided to file a case against the health administration to overcome what they considered the worst of the bureaucratic hurdles. In several regions, Agences régionales de santé (ARS) officials were indeed denying laboratories outside the referral hospitals the right to collect samples from suspect cases and to perform reverse transmission-polymerase chain reaction (RT-PCR) tests. Given the mounting pressure of what was becoming the ‘test scandal’, the Direction générale de la Santé (DGS) quickly confirmed that all certified laboratories—that is, all laboratories ‘working with the proper equipment, following the authorised protocol, employing samplers and led by a physician biologist’, private or public—were entitled to test for COVID-19. Following this action, the union received a request for information from a new Senate investigation committee established to scrutinise the government’s actions against COVID-19. The SJBM’s reply, sent on 2 April, not only presented its diagnosis of the situation but also offered an integrated plan for creating an enlarged testing network, scaling up testing practices during lockdown, and resurrecting the TTI strategy.
Another problem was the lack of personal protective equipment (PPE). The SJBM memo pointed to the extreme difficulties encountered by medical biologists in accessing masks, which often forced them to postpone or even stop sampling activities altogether. Biologists were usually not included on the limited list of medical personnel to whom pharmacists could deliver masks from public stocks. Even after the Ministry of Health finally amended the list, the number of masks available (18 per week, including six FFP2 masks) did not allow for regular sampling.
Beside obvious measures targeting the problems of scarcity, such as new pricing, government orders and stocks, and incentives to increase the national production of reagents, the SJBM’s response plan focused on scaling up the number of laboratories testing outside of hospitals. Building on their network of private ambulatory (city-based) laboratories, they aimed at doubling the number of official testing sites from 200 to 400 within a few weeks so as to be able to test patients with moderate symptoms and to facilitate coordination with general practitioners. They argued that drive-in centres and sampling at home should replace patients’ visits to hospital laboratory premises.
At this point, it is important to stress that the private laboratory biologists who claimed to be entitled to perform COVID-19 RT-PCR assays did not necessarily nurture any grudge against public hospitals. Quite the contrary: over the previous decades, a growing proportion of French private laboratories, especially larger ones, established close collaborations with such hospitals, which routinely farmed out part or all of their biological molecular assays to them. One of the driving forces behind the expansion of these informal public–private partnerships was the increasing number of molecular diagnostic assays approved for clinical use and market sales. The largest and best-equipped private biological laboratories were therefore part and parcel of a socio-technical network that included the provision and movement of sophisticated biological testing platforms established in an increasing number of teaching hospitals with the financial support of government agencies. In most of the 38 COVID-19 referral hospitals, therefore, medical and technical staff mastered the technical skills necessary to the implement a large-scale quasi-industrial diagnostic test scheme (involving sample circuits, testing apparatuses, computerised data transmission, quality control, certification of results, etc.). When, in mid-April, the Paris public hospital consortium Assistance publique–Hôpitaux de Paris (AP-HP) needed to set up a high throughput RT-PCR platform (using the 2 MGI SP960, BGI machine) for COVID-19 testing, it entrusted its organisation and operation to one of its own professors of pharmacy who had recently successfully set up a national high throughput DNA sequencing platform for healthcare purposes.
Understanding the uses of molecular diagnostic tests during the 20 years prior to the epidemic helps us to understand how RT-PCR assays were implemented once patients started to flock to the referral hospitals in March 2020. Three key words aptly characterise the approach to molecular diagnostics advocated by the elite expert clinicians who introduced those techniques and which framed the professional and clinical regulation of molecular diagnostics in the country (Bourgain et al. 2020; Turrini and Bourgain 2020): parsimony, timing, and articulation with other types of medical data. Importantly, the early and growing interest of these clinicians in molecular testing came together with a sense of caution concerning its use. The complexity that such tests could bring to clinical work called for moderation.
The ‘doctrine’ (part-formal, part-informal guidelines) for the use of diagnostic assays elaborated by leading French infectiologists in the middle of the COVID-19 epidemic displayed the same features. Even when maximum testing capacity had not been reached, as in some major teaching hospitals, guidance was given not to test asymptomatic or even mildly symptomatic hospitalised patients, as this would bring more confusion than clarity. Results, most likely to be negative, would be clinically meaningless. In practice, two complementary variables proved decisive in framing local uses of diagnostic tests in hospital settings during the epidemic: the local testing infrastructure and the severity of the epidemic in the area. In Paris and surrounding areas covered by AP-HP, disparities between hospitals were significant.
At the height of the ‘epidemic wave’, Hôpital Saint-Louis, which, although not a referral hospital, is a major university hospital equipped with a large all-purpose microbiology lab, was able to test all symptomatic patients admitted to the emergency unit. An infectiologist from this hospital told us on 9 April: ‘When it came to PCR tests, we never had any constraints. They [in the lab] worked a lot. They were able to perform numerous tests every day. The local testing capacity was large, with no financial limits. The stress on reagents has not been a hindrance.’ The situation was vastly different at the Hôpital Bichat-Claude-Bernard, a referral hospital in Paris, where patients with COVID-19 symptoms were not systematically tested but rather were selected on the basis of the severity of their symptoms, as in Strasbourg. At the Hospices Civils de Lyon, a teaching hospital, a waiting ward was set up for patients whose state of health justified admission but whose status with respect to COVID-19 was still unclear. Whereas, until the end of May, the local doctrine was to only allow patients with clear COVID-19 symptoms access to RT-PCR tests, a clinician volunteering at this waiting ward explained to us on 3 April that, ‘in practice, almost all patients [got] tested: the spectrum of COVID symptoms is so wide that it is rare that a patient does not fit in’. In Lyon, the epidemic wave was less severe and the hospital, as a member of the National Reference Centre (CNR) for respiratory infection viruses alongside the Pasteur Institute, had high PCR testing capacity.
When PCR tests were actually performed for diagnostic reasons, their clinical significance was often open to interpretation. PCR results were indeed articulated alongside other data (i.e., included in triangulation work, allowing their significance to be weighed according to clinical situations). Any time a patient displayed severe clinical manifestations, especially acute respiratory distress syndrome, the results of their PCR tests had little impact on their medical trajectory. A positive result would merely pinpoint the presence of the virus and further justify the patient’s admission. On the other hand, a negative PCR test did not preclude a COVID-19 diagnosis. As soon as clinical signs consistent with such a diagnosis were observed, a chest computed tomography (CT) scan was performed to check for specific lesions. When imaging came back with clear and unquestionable positive results, the probative value of molecular assays dropped sharply, to the point that inconclusive PCR tests could be repeated several times. In fact, the combination of compatible symptoms and imaging routinely led to a COVID-19 diagnosis, regardless of PCR results. A clinical biologist confessed to us how much he enjoyed ‘witnessing the way in which fellow clinicians undermine[d] the importance of PCR tests, the way they look at their usefulness. With COVID, PCR is losing its divinity among fellow clinicians’.
Ultimately, local combinations of testing capacities and levels of epidemic severity played a role in the rise of a different rationale for the use of tests in hospitals, one linked no longer to clinical diagnosis but to the control of the nosocomial contamination risk. Hospital clinicians argued for the need to identify all PCR-positive patients (including those who were asymptomatic or mildly symptomatic) admitted to hospital for clinical reasons unrelated to COVID-19. While the ability to limit the risk of sending ‘COVID+’ patients to hospital wards that had ‘non-COVID’ patients and thus to control iatrogenic contamination became a serious issue, knowledge of the PCR status of staff members was equally important. For example, as of 30 March 2020, following the detection of a case of COVID-19 in a non-COVID ward at Hôpital Saint-Louis in Paris, all patients and staff were tested without any consideration for their clinical status. Under such circumstances, the meaning of a positive test shifted; it was now a reason to move a patient to a COVID ward or to isolate a staff member. Use of the test consequently expanded to maximise the chances of identifying all PCR-positive staff or patients. Even in the absence of compatible imaging, health professionals with mild symptoms could be tested repeatedly, sometimes up to four times. By early April, biological tests were being used extensively for tracking nosocomial infections spread by asymptomatic health professionals in many hospitals across France’s most affected regions.
‘Test, trace, and isolate’ out of lockdown
France started to ease lockdown measures on 11 May 2020. Individuals who did not belong to the newly labelled ‘essential workforce’ no longer needed an exemption to exit their home, and the government started easing restrictions on workplaces, shops, and schools. The health authorities presented the ‘test, trace, and isolate’ (TTI) strategy as a precondition for easing lockdown, as well as the only alternative to it.
To prepare for this moment, it had been necessary to solve multiple issues regarding the implementation of the strategy and to clarify the logistics of tracing and isolating, the role of information technologies, and the role of reverse transmission-polymerase chain reaction (RT-PCR) tests in relation to the TTI approach. In the midst of these discussions, which mobilised the whole palette of health authorities mentioned above, the head of the government’s COVID-19 scientific council insisted on the need to take into account the scarcity of personnel rather than materials. On 30 April, he explained to a Senate investigation committee that effective TTI required the intervention of professionals rather than the sole mobilisation of information technologies:
Korea has brigades of tracers, including 20,000 persons, in order to trace the contact cases. Behind the apps, you have people. For the moment, we don’t have that in France and, if such brigades are not organised, the apps will not work. What is needed is a corps of roughly 30,000 tracers (Commission des affaires sociales du Sénat 2020).
On 13 May, the government launched the Système d’informations de DEPistage (SI-DEP), a national information system for COVID-19 screening, as the basis for its ‘contact tracing’ strategy (Ministère des Solidarités et de la Santé 2020a). This system tapped two sources of information about new cases. The first one, officially available from 3 June onwards, was a case-tracking smartphone app, StopCovid, which utilised Bluetooth technology.[12] The app was designed to advise every individual who spends more than 10 minutes close to an infected person to get tested, provided that the person has entered the unique code of her/his positive PCR test into the app. Second, tens of thousands of private practitioners throughout the country were expected to feed SI-DEP through their pre-existing professional accounts on the national social security platform, Amelipro. The contact-tracing strategy depended on the involvement of private practitioners in three key steps: firstly, physicians (mostly GPs) had to fill in the online form for every new COVID-19 case (via the boxes ‘confirmed positive RT-PCR result’ or ‘probable symptoms + CT-scan’) and start documenting their immediate contacts during consultations. Medical biology specialists then had to arrange for the sampling and testing of those cases in their private laboratories. Pharmacists then dealt with the follow-up of mask delivery to indexed patients and their contacts.
As Delfraissy alluded, epidemiological investigations of further cases linked to each patient necessitate significant human resources, as governments and NGOs involved in dealing with Ebola outbreaks on the African continent discovered (Wallace-Wells 2020). In France, these interventions were organised on the basis of phone calls made by employees (administrative officers, HR staff, etc.) of local social security agencies, who attended short ad-hoc training sessions in early May 2020 (Pineau and Hecketsweiler 2020). In addition to tracing cases, these professionals also checked isolation settings and the potential needs of patients and provided social support. When their investigations pointed at a cluster, the local ARS took over, performing a field investigation led by trained public health specialists, followed (if necessary) by quarantine.
From mid-May, the number of positive tests uncovered and documented through the contact-tracing platform in general practice remained low: the proportion of positive COVID-19 RT-PCR tests decreased from 20% in mid-April (already beyond the peak of COVID-19 incidence in France) to 2–3% in late May. This percentage was even lower in some regions. For example, during the week from 15 to 21 May, out of the 9,800 tests performed in the Bourgogne-Franche-Comté region, only 122 (1.25%) were positive (Delaporte 2020). In June 2020, the low number of tests performed to combat COVID-19 clusters led the government to use its newly acquired testing capacity to experiment with massive testing around detected clusters and in regions with higher incidence (Hecketsweiler and de Royer 2020).[13]
In this new testing landscape, where PCR testing was ubiquitously proposed as a national testing solution, everything seemed again under control. Capacity reached 300,000 tests per week in early July and confidence in this relative abundance was such that, by the end of month, the Ministry of Health—facing the protests of people who needed PCR tests in order to reduce risks while organising their family lives—eased the mandatory medical prescription and the prioritisation of access for patients with symptoms.
The limited implementation of TTI after lockdown became a matter of public debates by the end of September 2020, when the health administration mentioned renewed constraints on mobility and local curfews due to the clear signs of a second wave. The limited use of the app and the small number of contacts reported, as well as the frequent refusal of identified contacts to self-isolate, were at the forefront of public discourses, turning the problem into a matter of compliance. While discussing guidelines for a renewed tracing and isolation policy, the COVID scientific council on 3 September struck another chord. It pointed to the lack of governmental incentives in several important domains: support for contact cases, the design of an adapted strategy for risk reduction, and the easing of the social and personal consequences of isolation. The absence of compensation for lost revenues for asymptomatic persons stands as a good example (Conseil scientifique Covid 2020). It became clear that testing was not TTI and that the strategy required another type of intervention, one less technical and more social than those deployed earlier to scale up access.
Conclusion: Of abundance and scarcity
In this research article, we have detailed how, in France during the first months of the pandemic, the test, trace, and inform (TTI) strategy played out at the intersection of science, medicine, politics, and policymaking against a backcloth of multiple shortages. In so doing, we have been able to move beyond vague explanations, such as the often-mentioned ‘French public health’s backwardness’, to highlight how successive policy inflections impacted the national response to the pandemic. For example, the overwhelming of French public health agencies around mid-March 2020 undoubtedly illustrates the difficulties in building expertise and operational capabilities. The roots of this situation can be traced back to various decisions made by French governments since the 1930s as well as to organisational failures related to a series of administrative reforms implemented in the 2010s.
In addition, our study has stressed the need to broaden our understanding of scarcity and its impacts on policy responses to health crises. It is crucial to weigh the extent and nature of shortages experienced locally, as it is critical to take into account the ways in which these shortages have configured the spectrum of uses of diagnostic tests. This includes a focus on those health professionals and administrators faced by scarcities resulting from governmental failures and the ways in which they resort to ‘creative tinkering’ and elaborated ‘palliative’ strategies that help them regain some agency, at least temporarily.
We have argued that, throughout the period covered in this article (January–September 2020), a striking dialectic has existed between the shortages (of, for example, machines, reagents, and sampling personnel) limiting access to SARS-CoV-2 reverse transmission-polymerase chain reaction (RT-PCR) tests in France and the political decision-making processes concerning their use. On the one hand, scarcity largely explains the government’s early claims that pursuing a massive testing strategy (including contacts and asymptomatic cases) was useless in the prevailing epidemiological situation. On the other hand, this proclamation justified the prioritisation of hospital patients with severe symptoms in order to ease the clinical handling of patients in overstretched hospitals. Additionally, since the use of tests was then adjusted to suit local capabilities and capacities, this policy failed to implement a coordinated, national, and public effort to increase testing capacity at the peak of the epidemic. As a result, the policy created a vicious cycle and prolonged the scarcity. The dialectic of scarcity and policy is also the reason for the major role that health professionals —hospital practitioners as well as private medical biologists—have played in the creation of an enlarged testing network and in the scaling-up of capabilities.
Just like any other socio-technical object, virological tests are susceptible to multiple appropriations. We have described here two registers of the professional use of RT-PCR assays. We have defined ‘public health use’ as the first step of TTI, necessary to build epidemiologically informed interventions and to follow and control the spread of the virus. We have also defined a ‘clinical register of use’ as the process by which RT-PCR test results participate in orienting the medical trajectory of people who display symptoms associated with COVID-19. These uses are neither exclusive of each other nor peculiar to one actor or another. Our study shows that the relative political and social importance of these two registers of use kept evolving over time, from one phase of the pandemic to the next, with scarcity as a major determinant of the evolutionary changes’ characteristics.
France accordingly provides us with a fascinating case study of the ability of medical professionals to deal with shortages of key technical objects and to negotiate confusing guidelines during a major and multi-dimensional crisis. The French lockdown situation reveals forms of ‘bricolage’ taking place even in the wealthy Global North, ranging from the search for alternative resources and suppliers to local innovations in the maintenance of technical platforms and the governance of testing prioritised cases. In the end, such bricolage was endorsed by the health authorities as a demonstration of creativity rather than disparaged as a sign of weakness (see, for instance, the Assistance publique–Hôpitaux de Paris [AP-HP] director’s hearing by the National Assembly COVID-19 Commission: Hirsch et al. 2020).
The abundance of testing capacities that characterised the post-lockdown period in France proved almost as destabilising to social actors as scarcity. Indeed, the quick increase in test production capacities from early June 2020 onwards partly undermined the ‘registers of use’, which had been framed in a context of scarcity. Performing PCR tests without any further assessment of potential clinical symptoms and, from late July onward, without prioritising test requests effectively destabilised both the clinical and public health uses. By the beginning of July 2020, the view that one had a ‘right’ to know one’s status with regards to COVID-19 had taken root in the population. Indiscriminate testing and growing delays in the processing of samples and communication of test results (over a week, in many cases) began to limit the diagnostic value of the results as well as their utility for implementing a renewed TTI strategy, whose feasibility was already been undermined by the limited resources invested in it—namely the lack of tracing personnel, financial incentives, and support for those self-isolating.
One of the striking aspects of the introduction of COVID-19 tests in France therefore lies in the preserved gap between the dynamics of the epidemic and the dynamics of testing. In this respect, the French situation is neither extreme nor unique, at least in the European context. We hope that a detailed analysis of the practical ways in which the diversity of uses has operated in other countries will help us reflect upon the relationship between the testing practices, the various policies adopted in response to the pandemic, and the circulation of SARS-CoV2. Such a comparative exercise would be especially interesting in respect to the various Asian countries in which the implementation of TTI seems to have played a decisive role in reducing the transmission of COVID-19.
Acknowledgements
We thank our interlocutors for their generosity in terms of time and collaboration. We also thank MAT’s editors and the anonymous reviewers for their meticulous work and relevant advice, and Liz Librecht and Fred Johnson for their linguistic editing. Special thanks to Alexis Rayapoullé for his constructive participation in our reflections. Our gratitude is all the greater due to their help through these difficult pandemic times.
About the authors
Claire Beaudevin is a medical anthropologist and a researcher at the Centre National de la Recherche Scientifique (CNRS) in Paris, based at Cermes3 (Research Centre for Medicine, Sciences, Health and Society). Her work analyses the past and present entanglements of genetics, genomics, and global health. She conducts fieldwork in the Arabian Peninsula (Oman), where she studies the development of genetics and genomics within the clinic and in public health and research contexts. In France, she also investigates (alongside Catherine Bourgain and Ashveen Peerbaye) the development of routine cancer genomics in state-funded hospitals.
Luc Berlivet is a historian and sociologist of science and a researcher at the Centre National de la Recherche Scientifique (CNRS), based at Cermes3 (Research Centre for Medicine, Sciences, Health and Society). His work explores the historical changes in the uses of statistics in medicine, public health, and population sciences since the late 19th century. He has published extensively on the history and sociology of epidemiology, health education, eugenics, and human genetics.
Soraya Boudia is a historian and sociologist of science at Cermes3 (Research Centre for Medicine, Sciences, Health and Society) and a professor at Université de Paris. Her work explores the role of scientific knowledge in politics and policy, with a particular focus on the different ways of governing transnational health and environmental risks. Her current projects concern the politics of hazards in the nuclear industry and the green economy (i.e., recycling facilities).
Catherine Bourgain is a statistical geneticist and a sociologist of science at the Institut National de la Santé et de la Recherche Médicale (INSERM). She is the current director of Cermes3 (Research Centre for Medicine, Sciences, Health and Society). Her work explores the ways in which genomic technologies enter the clinic, the reconfiguration of actors and networks, the organisation of care, and the diagnostic work that these entail in areas such as cancer and cardiovascular diseases. She is also interested in models and ways of producing knowledge in the field of genomics at large.
Maurice Cassier is a sociologist and senior researcher at the Centre National de la Recherche Scientifique (CNRS), based at Cermes3 (Research Centre for Medicine, Sciences, Health and Society). His work explores innovation and appropriation regimes in health industries since the 19th century between the extension of exclusive property rights and common and public goods. Since 2002 he has directed a research programme on intellectual property and the local production of health technologies in the Global South.
Jean-Paul Gaudillière is a historian of science and senior researcher at the Institut National de la Santé et de la Recherche Médicale (INSERM), based at Cermes3 (Research Centre for Medicine, Sciences, Health and Society). His work explores the history of the life sciences and medicine during the 20th century, with recent research focusing on the history of pharmaceutical innovation and the uses of drugs with regards to the dynamics of health globalisation after World War II. From 2014 to 2019 he coordinated the European Research Council (ERC) project From International to Global: Knowledge, Diseases, and the Post-War Government of Health.
Ilana Löwy is a senior researcher emerita at Institut National de la Santé et de la Recherche Médicale (INSERM), Paris, based at Cermes3 (Research Centre for Medicine, Sciences, Health and Society). Trained as a biologist, she then retrained as a historian of science and medicine. Her main research interests are the relationships between laboratory sciences, clinical medicine, and public health and the intersection between gender studies and biomedicine in areas such as female cancers; contraception and the medicalisation of pregnancy; birth defects and prenatal diagnosis; and, more recently, Zika epidemics in Brazil.
Footnotes
-
In a bout of self-criticism, the chief medical officer for England and Wales, Chris Whitty, confessed on 10 June 2020 that he regretted not having sped up testing earlier: ‘Many of the problems that we had come because we were unable to work out exactly where we were’ (Reuters Staff 2020). As far as we know, no such regret has yet been expressed by any French senior medical officer (Hecketsweiler and de Royer 2020).↩︎
-
See, for example, The Lancet’s special issue France: Nation and World (and especially two papers: Delfraissy, Yazdanpanah, and Levy (2016); and Hollande (2016)).↩︎
-
Equivalent to the US norm N95 and the Chinese KN95.↩︎
-
As clearly displayed on Figure 1 and the cover image of this article, a government poster dated 27 March 2020.↩︎
-
Didier Houssin later chaired the emergency committee established by the WHO to investigate the outbreak of new coronavirus pneumonia in China (see World Health Organization 2020a).↩︎
-
The Agences régionales de santé (ARS) are executive agencies. Established in 2010, they aim to ‘rationalise’ the implementation of health services at the regional level. Their coordinating role at the local level attracted a lot of criticism during the COVID-19 pandemic in France.↩︎
-
All French-language quotations were translated into English by the authors.↩︎
-
The ‘field epidemiologist’ on the staff of the Auvergne-Rhône-Alpes ARS who was in charge of investigating the second French cluster (in the Alpine town of La Balme de Sillingy) in mid-February 2020 later revealed in an interview that she had to ‘go into self-isolation’ in the middle of her investigation as the mayor of the town was diagnosed with coronavirus and they had shaken hands the previous day (Malye 2020).↩︎
-
The praise occurs between 3:07 and 3:50.↩︎
-
The first outbreak started in the Alsatian region of Mulhouse following a week-long prayer meeting attended by over 2,000 followers of an Evangelical denomination called the Mission du Plein Évangile—Église Porte Ouverte Chrétienne [Open Door Christian Church] from 17 to 21 February. The second cluster materialised in and around Creil, a city in the Ile-de-France region (by far the most populated region of the country), home to large military intelligence facilities.↩︎
-
Public debates about bioMérieux’s activities erupted in late March. On 26 March, MP Sébastien Nadot (previously a member of the presidential party) requested its requisitioning by the state under the emergency health law. The government did not consider this plea, even though it had ordered the requisitioning of mask production facilities a few weeks earlier.↩︎
-
StopCovid’s use of Bluetooth remains highly controversial due to its capacity to breach user and patient confidentiality. The app was renamed TousAntiCovid in October 2020.↩︎
-
The Ile-de-France ARS thus launched a campaign for systematic testing in 32 municipalities with the aim of better understanding the virus’ circulation and the dynamics of cluster formation. All inhabitants were targeted and serological tests were included (Le Parisien/AFP 2020).↩︎
References
Berlivet, Luc. 2008. ‘Between Expertise and Biomedicine: Public Health Research in France after the Second World War’. Medical History 52 (4): 471–492. https://doi.org/10.1017/s0025727300002982.
Bernard Stoecklin, Sibylle, Patrick Rolland, Yassoungo Silue, Alexandra Mailles, Christine Campese, Anne Simondon, Matthieu Mechain, et al. 2020. ‘First Cases of Coronavirus Disease 2019 (COVID-19) in France: Surveillance, Investigations and Control Measures, January 2020’. Eurosurveillance 25 (6): 2000094. https://doi.org/10.2807/1560-7917.ES.2020.25.6.2000094.
bioMérieux. 2020. ‘BioMérieux reçoit l’autorisation d’utilisation en urgence de la FDA pour le test Biofire Covid-19’. bioMérieux. Press Release. 24 March. https://www.biomerieux.com/fr/biomerieux-recoit-lautorisation-dutilisation-en-urgence-de-la-fda-pour-le-test-biofirer-covid-19.
Bourgain, Catherine, Lionel Pourtau, Chafika Mazouni, Martine Bungener, and Julia Bonastre. 2020. ‘Imperfect Biomarkers for Adjuvant Chemotherapy in Early Stage Breast Cancer with Good Prognosis’. Social Science & Medicine 246: 112735. https://doi.org/10.1016/j.socscimed.2019.112735.
Brown, Phil. 1995. ‘Naming and Framing: The Social Construction of Diagnosis and Illness’. Journal of Health and Social Behavior 35 (extra issue): 34–52. https://doi.org/10.2307/2626956.
Bureau, Olivier. 2020. ‘Coronavirus : des Ehpad se lancent dans le dépistage systématique’. Le Parisien. Web. 31 March. https://www.leparisien.fr/societe/sante/coronavirus-des-ehpad-se-lancent-dans-le-depistage-systematique-31-03-2020-8291694.php.
Cherel, Laetitia, and Cellule Investigation de Radio France. 2020. ‘Dépistage du coronavirus : le coup de gueule d’un généticien’. Web. 25 March. https://www.franceinter.fr/societe/depistage-du-coronavirus-le-coup-de-gueule-d-un-geneticien.
Commission des affaires sociales du Sénat. 2020. Audition de MM. Jean-François Delfraissy, président et Arnaud Fontanet, membres du Comité scientifique Covid-19. Sénat. 30 April. http://www.senat.fr/compte-rendu-commissions/20200427/soc.html#toc4.
Conseil scientifique Covid. 2020. Avis n°9, Stratégie et modalités d’isolement. 3 September.
https://solidarites-sante.gouv.fr/IMG/pdf/avis_conseil_scientifique_3_septembre_2020.pdf.
Corman, Victor M., Olfert Landt, Marco Kaiser, Richard Molenkamp, Adam Meijer, Daniel Kw Chu, Tobias Bleicker, et al. 2020. ‘Detection of 2019 Novel Coronavirus (2019-nCoV) by Real-Time RT-PCR’. Euro surveillance 25 (3): 2000045. https://doi.org/10.2807/1560-7917.ES.2020.25.3.2000045.
Delaporte, Lucie. 2020. ‘Retard des tests Covid-19 : l’ombre des conflits d’intérêts’. Mediapart. Web. 22 May. https://www.mediapart.fr/journal/france/210520/retard-des-tests-covid-19-l-ombre-des-conflits-d-interets.
Delfraissy, Jean-François. 2020. ‘Coronavirus : entretien avec le Pr Jean-François Delfraissy’. Lapix, Anne-Sophie (interviewer). France 2 Evening News Program. TV interview. 18 March. https://www.francetvinfo.fr/sante/maladie/coronavirus/coronavirus-entretien-avec-le-pr-jean-francois-delfraissy_3873703.html.
Delfraissy, Jean-François, Yazdan Yazdanpanah, and Yves Levy. 2016. ‘REACTing: The French Response to Infectious Disease Crises’. The Lancet 387 (10034): 2183–2185. https://doi.org/10.1016/S0140-6736(16)30059-9.
Direction générale de la Santé. 2020. ‘Point de situation, 17 mars 2020’. Web. 17 March. https://solidarites-sante.gouv.fr/soins-et-maladies/maladies/maladies-infectieuses/coronavirus/etat-des-lieux-et-actualites/article/points-de-situation-coronavirus-covid-19.
Frouville, Margaux de. 2020. ‘Coronavirus : comment sont analysés les cas suspects en France ?’. BFMTV. Web. 24 January. https://www.bfmtv.com/sante/coronavirus-comment-sont-analyses-les-cas-suspects-en-france_AN-202001240084.html.
Gairaud, Marie-Anne. 2020. ‘Coronavirus : 8000 diagnostics lancés cette semaine dans tous les Ehpad de Paris’. Le Parisien. Web. 5 April. https://www.leparisien.fr/paris-75/coronavirus-8-000-diagnostics-lances-cette-semaine-dans-tous-les-ehpad-de-paris-05-04-2020-8294502.php.
Haut Conseil de la santé publique. 2020. ‘Avis sur les indications prioritaires du diagnostic par RT PCR - Lettre au Directeur général de la Santé’. Web. 10 March. https://solidarites-sante.gouv.fr/IMG/pdf/new_hcsp-sars-cov-2_patients_fragiles_v3.pdf.
Hay Burgess, Deborah C., Jeffrey Wasserman, and Carol A. Dahl. 2006. ‘Global Health Diagnostics’. Nature 444 (1): 1–2. https://doi.org/https://doi.org/10.1038/nature05440.
Hecketsweiler, Chloé, and Solenn de Royer. 2020. ‘Coronavirus : face à la commission d’enquête, Jérôme Salomon ne lâche rien’. Le Monde. Web. 17 June. https://www.lemonde.fr/politique/article/2020/06/17/coronavirus-face-a-la-commission-d-enquete-jerome-salomon-ne-lache-rien_6043099_823448.html.
Hollande, François. 2016. ‘Towards a Global Agenda on Health Security’. The Lancet 387 (10034): 2173–2174. https://doi.org/10.1016/S0140-6736(16)30393-2.
Ilef, Danièle (ed.). 2011. La veille et l’alerte sanitaires en France. Saint-Maurice: Institut de veille sanitaire.
Juttel, Annemarie. 2009. ‘Sociology of Diagnosis: A Preliminary Review’. Sociology of Health and Illness 31 (2): 278–99. https://doi.org/10.1111/j.1467-9566.2008.01152.x.
Le Parisien/AFP. 2020. ‘Covid-19 : une campagne de tests à grande échelle débute dans 32 communes d’Ile-de-France’. Le Parisien. Web. 29 June. https://www.leparisien.fr/societe/covid-19-une-campagne-de-tests-a-grande-echelle-debute-dans-32-communes-d-ile-de-france-29-06-2020-8344329.php.
Lescure, Francois-Xavier, Lila Bouadma, Duc Nguyen, Marion Parisey, Paul-Henri Wicky, Sylvie Behillil, Alexandre Gaymard, et al. 2020. ‘Clinical and Virological Data of the First Cases of COVID-19 in Europe: a Case Series’. The Lancet Infectious Diseases 20 (6): 697–706. https://doi.org/10.1016/S1473-3099(20)30200-0.
Magenou, Fabien. 2020. ‘Coronavirus 2019-nCoV : comment la France a développé son propre test pour détecter le virus’. FranceInfo. Web. 30 January. https://www.francetvinfo.fr/sante/maladie/coronavirus/coronavirus-comment-la-france-a-developpe-son-propre-test-pour-detecter-le-virus_3803333.html.
Malye, François. 2020. ‘Coronavirus : l’exemple des deux premiers “clusters” français’. Le Point. Web. 17 April. https://www.lepoint.fr/sante/coronavirus-l-exemple-des-deux-premiers-clusters-francais-17-04-2020-2371839_40.php.
Ministère des Solidarités et de la Santé. 2020a. ‘Décret n° 2020-551 du 12 mai 2020 relatif aux systèmes d’information mentionnés à l’article 11 de la loi n° 2020-546 du 11 mai 2020 prorogeant l’état d’urgence sanitaire et complétant ses dispositions’. Journal Officiel 0117. 13 May. https://www.legifrance.gouv.fr/eli/jo/2020/5/13/0117.
Ministère des solidarités et de la santé. 2020b. Préparation au risque épidémique Covid-19. Établissements de santé, Médecine de ville, Établissements médico-sociaux. Guide méthodologique. Paris: Ministère des solidarités et de la santé.
Pascariello, Pascale, Antton Rouget, Alexander Abdelilah, Guillaume Krempp, and Robert (We Report) Schmidt. 2020. ‘“Le virus se propage”, “il faut dépister” : ces alertes de médecins qui ont été ignorées’. Mediapart. Web. 14 May. https://www.mediapart.fr/journal/france/140520/le-virus-se-propage-il-faut-depister-ces-alertes-de-medecins-qui-ont-ete-ignorees.
Piarroux, Renaud, and Antoine Flahault. 2020. ‘Renaud Piarroux et Antoine Flahault : “Il y a encore beaucoup de virus en circulation”’. Salamé, Léa (interviewer). France Inter - L’invité de 8h20 : Le Grand Entretien. Radio broadcast. 15 April. https://www.franceinter.fr/emissions/l-invite-de-8h20-le-grand-entretien/l-invite-de-8h20-le-grand-entretien-15-avril-2020.
Picard, Jean-François. 2003. ‘Aux origines de l’Inserm : André Chevallier et l’Institut national d’hygiène’. Sciences Sociales et Santé 21 (1): 5–26. https://doi.org/https://doi.org/10.3406/sosan.2003.1574.
Pineau, Elisabeth, and Chloé Hecketsweiler. 2020. ‘Coronavirus : après dix jours de “contact tracing”, les enquêteurs de l’Assurance-maladie ne voient pas arriver de rebond’. Le Monde. Web. 23 May. https://www.lemonde.fr/societe/article/2020/05/23/coronavirus-apres-10-jours-de-contact-tracing-les-enqueteurs-de-l-assurance-maladie-ne-voient-pas-arriver-de-rebond_6040507_3224.html.
Reuters and Henri-Pierre André. 2020. ‘BioMérieux va fabriquer en Ariège son premier test de diagnostic du Covid-19’. L’Usine nouvelle. Web. 11 March. https://www.usinenouvelle.com/article/biomerieux-va-fabriquer-en-ariege-son-premier-test-de-diagnostic-du-covid-19.N938961.
Reuters Staff. 2020. ‘UK Lockdown a Week Earlier Could Have Halved COVID-19 Death Toll, Scientist Says’. Web. June 10. https://fr.reuters.com/article/topNews/idUKKBN23H2GB.
Schneider, William H. 2003. ‘War, Philanthropy, and the National Institute of Hygiene in France’. Minerva 41 (1): 1–23. https://doi.org/https://doi.org/10.1023/A:1022257805553.
Secrétariat Général de la Défense et de la Sécurité Nationale. 2011. Plan national de prévention et de lutte ‘Pandémie grippale’. Document d’aide à la préparation et à la décision. Paris: SGDSN.
Street, Alice. 2014. Biomedicine in an Unstable Place: Infrastructure and Personhood in a Papua New Guinean Hospital. Durham, NC: Duke University Press.
Turrini, Mauro, and Catherine Bourgain. 2020. ‘Genomic Susceptibility in Practice: The Regulatory Trajectory of Non-Rare Thrombophilia (NRT) Genetic Tests in the Clinical Management of Venous Thrombo-Embolism (VTE)’. Social Science & Medicine: 112903. https://doi.org/10.1016/j.socscimed.2020.112903.
Véran, Olivier. 2020. ‘Coronavirus : Olivier Véran ne veut pas annuler Lyon-Juventus et la Fashion Week’. Ventura, Alba (interviewer). L’invité RTL. Radio broadcast. 25 February. https://www.rtl.fr/actu/politique/coronavirus-olivier-veran-ne-veut-pas-annuler-lyon-juventus-et-la-fashion-week-7800153008.
World Health Organization. 2020a. ‘International Health Regulations Emergency Committee on Novel Coronavirus in China — 23 January 2020’. Minutes. 23 January. https://www.who.int/docs/default-source/coronaviruse/transcripts/ihr-emergency-committee-for-pneumonia-due-to-the-novel-coronavirus-2019-ncov-press-briefing-transcript-23012020.pdf?sfvrsn=c1fd337e_2.
World Health Organization. 2020b. ‘Protocol: Real-time RT-PCR Assays for the Detection of SARS-CoV-2 — Institut Pasteur’. Web. https://www.who.int/docs/default-source/coronaviruse/real-time-rt-pcr-assays-for-the-detection-of-sars-cov-2-institut-pasteur-paris.pdf.
World Health Organization. 2020c. ‘WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19 — 16 March 2020’. Web. 16 March. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---16-march-2020.