In this article, I address an issue that emerged during my ethnographic fieldwork in Brazil in 2018, which received little attention during the Zika virus outbreak that took place in the country during 2015–17. My fieldwork revealed that, interestingly, despite the epidemic and its associated risk of birth defects, some couples who were attending a fertility clinic (most of whom came from a middle- or upper-class background, with access to private health care) chose to take the risk of a pregnancy instead of delaying their plans. I argue that this case study of assisted reproductive technology (ART) is a ‘grey zone’ whose investigation aids understanding of how the Zika epidemic was managed in Brazil. By looking at the potentiality of pregnancies and prospective babies for (infertile) couples, we can analyse how fertility clinics influenced the ability of couples to engage in ART during the epidemic and explore which kinds of reproductive services were offered to patients during this time. More broadly, this case study permits the examination of how the specific case of ART sheds light on the issue of risk/reward in wider reproductive decision-making during the epidemic. In many ways, I conclude, one can say that the Zika virus epidemic came to challenge both the timing of reproduction and the choice to become pregnant.
Assisted Reproductive Technologies
A Grey Zone in the Zika Epidemic in Brazil?
—
Abstract
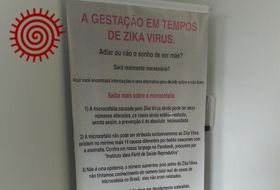 Poster in a private fertility clinic in São Paulo, Brazil, 2018. The poster begins: 'Pregnancy in times of Zika virus. To postpone or not the dream of being a mother? Is it really necessary?’. Image by the author.
Poster in a private fertility clinic in São Paulo, Brazil, 2018. The poster begins: 'Pregnancy in times of Zika virus. To postpone or not the dream of being a mother? Is it really necessary?’. Image by the author.
‘Use repellent and do not get pregnant!’
No serious health policy can consider sexual abstinence and avoiding
pregnancy as reasonable recommendations for reproductive health or the
control of an epidemic with multiple forms of transmission – this
epidemic in particular, [because of] vector and sexual
transmission.
(Diniz 2016, 140–41 [my translation]).
While management of the Zika health emergency of 2015–2017 in Brazil emphasised mosquito bite prevention tools for pregnant women in order to prevent in utero transmission, sexual and reproductive issues were given secondary status.[1] The fact of sexual transmission of the Zika virus, for instance, has never been brought to public attention and almost no information about this mode of transmission has been circulated in Brazil by its Ministry of Health. Sexual and reproductive risk factors have been minimised despite the many recommendations regarding sexual transmission that have been issued by the World Health Organization (WHO, 2016a). In the United States, conversely, the Centres for Disease Control and Prevention (CDC) recommended having protected sex (or abstaining) during pregnancy (CDC 2021a). One can see these policy decisions to minimise sexual and reproductive risk factors as inappropriate, or even deleterious to Brazilian public health since the presence of the virus in bodily fluids, and its persistence for several months, have been widely documented.[2]
In September 2017, nine months after the start of the media coverage of the Zika virus epidemic, epidemiologists examining the city of São Paulo raised an alert about a possible reduction in its birth rate (Diaz-Quijano, Alexander, and Dias Porto Chiavegatto Filho 2017). It was later found that there had been an overall decrease of 7.8% in the national birth rate in 2016. This decrease reached 10.8% in the cities that in 2015 had had the highest rates of microcephaly—a birth defect associated with Zika virus infection during pregnancy (Diaz-Quijano, Pelissari, and Dias Porto Chiavegatto Filho 2018). Even though it is very difficult to obtain reliable numbers (Bahamondes et al. 2016), social scientists suggest it is likely that during the epidemic many women postponed pregnancy or had an abortion as soon as they learned of their pregnancy and the risk of getting infected by the Zika virus (Marteleto, Weitzman, and Zanatta Coutinho 2017b; Guedes de Mello and Rondon 2020). Consequently, social researchers and activists have focused mostly on equal access to sexual and reproductive rights such as contraception and abortion. The promotion of such rights could have been what Diniz (2016) terms above a ‘serious health policy’ (see also Diniz, Medeiros, and Madeiro 2017). The Zika virus epidemic has de facto put reproductive rights back on the agenda, since it sheds light on the stratified nature of reproduction in Brazil. As Correa and Löwy (2020, page) point out in their examination of unequal access to health services in Brazil, ‘one of the areas strongly affected by structural inequalities is reproductive health’; it is mostly women of middle and upper socioeconomic status who have access to pregnancy planning tools, reliable contraception, and illegal, safe abortion. As always, a large proportion of Brazilian women are left to their own fate.
However, the urge to study, report, and act on this social and health crisis has in some ways left grey areas of un-investigated issues that are important for the understanding of reproduction and the biopolitics of the epidemic at a broader systemic level. One of these is the ‘potentiality’ of viable pregnancies (and therefore, the ‘potentiality’ of babies born) in 2016 and 2017. In other words, the choice made by couples and women who intended to get pregnant and chose to postpone their plans—or instead took the risk of pregnancy during the Zika epidemic.
Methodology
Initially considering the research topic of ‘potentiality’ of pregnancies likely to result in a healthy live birth, I intended to look first at practices of prenatal diagnosis of mother-to-foetus infection. Because of the time that had elapsed between the beginning of the Zika virus epidemic (the end of 2015) and my arrival in Brazil (mid-2017), however, I had to shift the focus of my research and decided instead to interview reproductive health professionals and women who were of childbearing age at the time of the epidemic outbreak. I began my fieldwork in the city of São Paulo, in the southeast of Brazil, in order to investigate the impact of the Zika virus epidemic on reproductive practices in a less-affected geographical area. The main discourse I heard from health professionals was that the epidemic was located in the northeast, and that everybody in the south of the country had already forgotten about it (Prado 2018). Following that common belief, I went to Recife, the capital of the northeastern state of Pernambuco, to interview women who had given birth to children with congenital Zika syndrome,[3] and to speak to reproductive and child health professionals. As I was asking about prenatal monitoring during the Zika virus epidemic, I happened to hear about the only medical field where Zika virus testing was compulsory: medically assisted procreation. I decided to pursue this new topic, one that was on the fringes of the epidemic’s main social issues but one that could offer a different and complementary perspective on reproductive decision making.
I sought to investigate how fertility clinics influenced the ability of women and couples to engage in assisted reproductive technology (ART) during the spread of the Zika virus epidemic in Brazil, exploring the kinds of reproductive services that were offered at the time (Borges et al. 2017). More broadly, I aimed to identify how the specific case of ART articulates the issue of risk/reward in reproductive decision-making during the Zika virus epidemic.
It is worth noting that although fertility treatments are theoretically provided through Brazil’s public national health service [Sistema Único de Saúde], in practice access to such publicly-funded treatment is very—and increasingly—limited (Correa and Löwy 2020). Only privileged women and couples can access and pay for ART, and most of the clinics are in the richest, southern states: 66% as opposed to just 1% in the much poorer north (Ibid.).
During my second period of fieldwork in 2018 in São Paulo and Recife, I conducted interviews with obstetrician-gynaecologists and biologists from private fertility clinics, as well as with women who had had pregnancy plans during and after the Zika virus epidemic. I also had the opportunity to observe an assisted reproductive procedure in the laboratory of a private fertility clinic. What I present next are the first results of my ongoing research.
A grey zone in the politics of reproduction
The risk of vertical (mother-to-child) and sexually transmitted infection of the Zika virus was evidenced by early 2016, shortly after the epidemic had started in 2015 (see Oliveira Melo et al. 2016 and Mlakar et al. 2016 on vertical transmission; Musso et al. 2015, Atkinson et al. 2016, and D’Ortenzio et al. 2016 on sexual transmission). In May 2016, three months after the international emergency had been declared by the WHO (2016b), the Brazilian Health Regulatory Agency [Agência Nacional de Vigilância Sanitária – Anvisa] announced a change in the regulation of blood donation and assisted reproduction procedures (Anvisa 2016). With the risk of virus persistence in gametes (sexual transmission) and the teratogenic effects of the Zika virus (vertical transmission), patients involved in fertility treatments were to be tested for Zika before the insemination or embryo transfer took place in order to avoid any infection during the fertilization process (Araújo Filho et al. 2019), as well as be tested for infection at the beginning of the potential pregnancy. The terms of this new regulation are binding:
According to the document published by Anvisa, CGTBs [cell and germ tissue banks] can only collect gametes or germ tissue for use in assisted reproduction procedures after obtaining non-reactive or negative test results for ZIKV [Zika virus] infection no more than five days prior to gamete collection; individuals whose laboratory tests yield positive or inconclusive results will be temporarily suspended from treatment and tested again 30 days later (de Carvalho et al. 2016).
Among all maternal health policies, assisted reproduction technologies (regardless of who funds them) are the only ones that are subject to strict regulation regarding the risk of Zika virus infection. Indeed, ART is the only field where the risk of sexual transmission—and not just the potential of vector and vertical transmission during pregnancy—is implied and considered. Since both men and women must be tested when their sperm or eggs are collected, which is before the fertilization takes place, the risk of sexual transmission can no longer be ignored by sexual health professionals, despite its absence from Brazilian public health recommendations.
Anvisa’s new regulation has not been unanimously welcomed, and controversies remain among specialists in human reproduction (doctors, gynaecologists, and virologists) when it comes to deciding what to do if one of the patients tests positive for the Zika virus. According to Valéria, a renowned virologist whom I interviewed, it is not known, for instance, whether sperm washing (a treatment used for semen from male patients who are HIV positive that is designed to remove disease-carrying material), may be a suitable and reliable means of eliminating the Zika virus from the gamete. The same uncertainty about the persistence of infection applies to the oocyte, and no possibilities exist to test either the oocyte or the embryo in vitro, without the risk of damaging them both. In other words, no further test and no reliable treatment is available to a couple who test positive for Zika virus infection during an ongoing fertility procedure.
In theory, within a strict interpretation of the Anvisa regulation, if a Zika infection is confirmed then the gamete materials must not be collected, and the process must then be delayed for at least one month. This potential delay in the fertility treatment (which is rarely enforced in practice) is always presented by professionals within the field of reproduction as a waste of time and money for their patients, who lose the investment they have made in a fertile cycle and the embryo; implicitly, the clinical professionals are referring to the same consequences for the clinics themselves.
In practice, then, fertility clinics (and I recall that the vast majority of them are private), form their own understanding of the regulation: some offer egg or sperm freezing in order to preserve the gamete while waiting for a safer winter season—even though, as Valéria reminded me, ‘freezing is the best way to keep the virus alive’. Others offer to freeze the embryo and wait for embryo transfer, while others give in to the pressure of patients ‘in a hurry’, as one clinician said, and proceed with the embryo transfer against recommendations.
When I asked a gynaecologist in São Paulo about the implications of the Zika virus in the practices of their fertility clinic, I was told:
Zika is a big issue. Especially because the compulsory test for Zika is very expensive and it’s an additional cost for our patients. And because women sometimes don’t have time to wait … and wait for what? Nobody knew when the epidemic was going to end, and nobody knows if it will return. Besides, none of our patients [of higher socioeconomic backgrounds] has been infected by Zika, it happened in poor areas of the northeast region.
In other words, Zika cannot be legally ignored by the fertility clinics because of the national regulation: testing the couples for Zika is compulsory. Nevertheless, according to professionals’ discourses, the risk is largely minimised in their own practices of collecting and freezing eggs and sperm and creating embryos.
Another gynaecologist specialising in reproduction in São Paulo, Dr Pedro, remembers the panic that occurred between the end of 2015 and the beginning of 2016:
There was a significant lack of information coming from the federal council of medicine. At the beginning of 2016, nobody knew what the consequences would be. So people decided to wait for the winter to get pregnant. The outbreaks of the three arboviruses (dengue, chikungunya, and Zika) that happened that year were definitely very distressing. You must understand that the patients that arrive here at the clinic are already exhausted [esgotados] after more than a year trying to get pregnant naturally: they have frustrations, physical and mental pain. When they arrive here, they want the process to begin right away, they expect us to make it happen fast. So, the delay imposed by the Zika epidemic increased the stress. It’s a matter of exchanging a risk [of infection and thereafter of birth defects] for another risk [of not having babies at all]. It all depends on the context and the perception of the risk; on the age too. If the woman has little time left [of fertility], she will take the risk of Zika infection.
It seems that ART clinics and gynaecologists are approaching the Zika epidemic as a matter of cost/benefit in order to justify the risk of investing in a potential pregnancy. In their discourses, they often refer to scientific uncertainties but also to financial costs, implicit social class bias (believing that the mainly upper-class patients of private clinics wouldn’t be at risk), and the consideration of their patients’ mental health (emotional ‘exhaustion’). From the reproductive professionals’ point of view, the patients themselves also weigh up the cost/benefit of delaying their plans of pregnancy when they are reminded of the risk of remaining childless.
Having or not having (healthy) babies
Dr Pedro also works in a public hospital—the only one in Brazil (to my knowledge) that offers all stages of fertility treatment free of charge. He highlighted that the waiting conditions are not equal for every patient:
In the public hospital where I work, I have a case of a young woman who tried for eight years to get pregnant. When she arrived at the hospital, she had to go through all the tests in the public health service, so she has been in the queue for two more years. Those kinds of cases are more serious because they take years to be taken care of by our service. Those patients will never postpone the treatment when they have the chance to access it.
I did not have the chance to visit this public service nor to meet women who were being treated within the public health system. I can only assume that the issue of delaying pregnancy plans follows a heavier and more painful path for people that have been waiting for many years within the public service queue—often people of middle and lower socioeconomic status.
Dr Pedro concluded by saying that Zika represents a spectre of fear within the ART field in São Paulo and that he never saw anyone testing positive for the infection. It is worth noting that I was told the exact same thing by a private clinic director from Rio de Janeiro, where the prevalence of the virus was much higher.
In a private clinic in Recife, Dr Amanda also confirmed that she had encountered no cases of Zika among the pregnant patients that she has treated. She explained that her patients are ‘enlightened’ [esclarecidas]: a common expression in Brazil used when speaking about people of high socioeconomic status. Describing the women as esclarecidas assumes that they have enough cultural and economic capital to prevent themselves from the risk of infection. Dr Amanda explained how ‘the women who arrived at the consultation for a fertility treatment were already prepared: avoiding mosquito exposure, using repellent, wearing long clothes, staying indoors with air conditioning … all because of the panic and the media. Sometimes it was exaggerated too, some women wanted to put on repellent every hour’. Dr Amanda had faced a decrease in the number of patients between 2015 and 2016:
Only the couples who couldn’t wait, women of 39–40 years old, or patients with a very specific issue, continued the treatment. Younger couples who were trying for two or three years decided to postpone or freeze their embryos. I saw one case of serology positive to Zika in a woman who was being treated. She froze her embryo and repeated the test for Zika twice, and it came back negative both times … We didn’t know if it was a false positive result the first time. So, she didn’t know what to do and chose not to transfer the embryo at that time. When she eventually came to the transfer, she had a miscarriage. The test for Zika is our responsibility, we are not allowed to begin the process of fertilization [either insemination or embryo transfer] if there is no test. But then, prevention during pregnancy is the woman’s responsibility.
By disconnecting the process of biological reproduction from the process of parenthood that develops during pregnancy, gynaecologists in reproductive medicine deny their responsibility for what could happen after the fertilization process; or, at least, they often show little concern about the evolution of the pregnancy.
After the beginning of the winter of 2016, the flow of patients returned to normal. When asked in September 2018 what she recommended now to her patients, Dr Amanda replied:
When a woman of 38 years old says that she’s afraid of Zika, I tell her that she has statistically more chance of having a baby with Down syndrome. ‘You want to wait? OK, but then your chances of having a baby with Down syndrome will increase.’
Once again, reproduction specialists tend to highlight the cost/benefit of delaying pregnancy—and the still higher cost of waiting to get pregnant. Dr Amanda used a comparison between statistics of various congenital malformations (taking the well-known case of Down syndrome risk as an example) to convince her patient that she has no ‘rational’ concern about the Zika epidemic.
The Zika epidemic has been a major problem for fertility clinics, economically speaking, because many couples decided not to start fertility treatment. Consequently, the rate of IVF and embryo transfer decreased by almost 30% in the first semester of 2016, according to several ART professionals, sometimes threatening closure of the clinics with low rotation rates (of patients and ongoing procedures). In an article questioning the necessity of Zika testing in ART, de Souza et al. (2016) note that: ‘The public health care system and private health insurance companies do not process refunds for these tests, and they significantly increase the cost of treatment to patients. Interestingly, the cost of testing is equivalent to approximately 1.2 days [costing the equivalent of US$200] of treatment with controlled hyperstimulation drugs’.[4] The new Anvisa regulation therefore also had consequences for the patients’ financial investment: the additional costs of the Zika tests for the couple (rarely reimbursed by health insurance) at every attempt of a fertilization procedure.
The biological fertility clock
One of my last interviews in Brazil was with Andréia, a laboratory biologist in charge of the technical procedures of in vitro fertilization (IVF)—freezing and so on—and co-owner of a fertility clinic in Recife. Unlike her gynaecologist colleagues, she was talkative and eager to give me all the details about her job and her perception of the patients. In the very first minutes of our meeting she explained:
Couples where the woman is over 36 years old couldn’t wait because of the biological clock. So, they did the fertilization procedure but didn’t tell anyone, not even their family, for fear of being judged.
When I asked her who had told them they couldn’t wait, she replied:
It's often in their own minds. We didn’t say they should not do the treatment but … the women are so anxious!
According to Marteleto et al. (2017, 10) in their research on women’s reproductive behaviour during the Zika epidemic in Brazil:
Age was a key factor that explained a short period of postponement or no postponement during the ZIKV [Zika virus] epidemic for several high-SES [socioeconomic status] women. Notably, these discussions about age were not as frequent among low-SES women, who tended to have children at a much younger age.
As Marteleto highlights: ‘Socioeconomic status shapes women’s ability to obtain and afford reproductive services’ (ibid., 5–6). One can assert that there is a ‘reproductive privilege’ in delaying pregnancy and preserving oneself from Zika virus infection (the ‘privilege’ being here understood as the chance to access effective contraception, negotiate contraceptive use with the partner, and access effective repellent).
The key factor associating age with (in)fertility issues explains the reproductive choices and practices among the group that attends fertility clinics. This fact exemplifies the systemic stratified nature of reproduction in Brazil. It has, however, a major downside, which is the difficulty for those women of living different temporalities at the same time: the temporality of the epidemic, the temporality of the ticking biological clock (and female fertility in particular), and the temporality of the IVF cycles and ART (egg freezing, embryo freezing, and transfer).[5] Consequently, the impossible choice between taking the risk of delaying and having no future pregnancy on the one hand, and taking the risk of Zika infection and transmission to the foetus, on the other.
Although some women and couples took the ‘risk’ of getting pregnant during the Zika pandemic—a long-wanted pregnancy coming at very considerable emotional and financial cost—the anxieties do not stop there.
Felícia, a 36-year-old mother of twins born in 2016 through IVF, is one of these mothers who was told by her gynaecologist that she couldn’t wait because of her and her husband’s fertility issues. She shared the story of her pregnancy with me:
The medical indication was not to wait. If I could have waited, I would have postponed the IVF procedure, because of Zika. Fifteen days before the embryo transfer, I had to do all the necessary blood tests in order to avoid the risk of infection [by] TORCHS, etc.[6] My husband and I did the Zika test twice, one 15 days before, and the second a few days before the embryo transfer, it cost around 2000 reals (around US$500). During pregnancy, I wasn’t tested again for Zika. I used repellent every day, I moved to an apartment on the eighth floor, turned the air-conditioning on, and put a mosquito net at every window. I had Zika in my mind all the time … at work [as an infectious disease specialist in a private hospital] all we talked about was new articles about Zika, so I knew well about the risks!
One day I killed a mosquito with my shoe, and it was full of blood. I didn’t know if it was my mother’s or mine. It’s the only time I ever saw a mosquito in my building. When I saw its little legs [showing me a picture of the crushed mosquito on her phone], I freaked out! I immediately called my doctor to ask for a test. My insurance covered the blood test but not the urine test. It was negative. But I thought about Zika until the last moment of my pregnancy, I thought a lot about the little head[s] of the newborns.
I heard about women that ran away to Argentina, Miami, or the south of Brazil [to escape the epidemic]. If I were living in the northeast of Brazil, maybe I would have done the same thing.
It is clear that memories of the epidemic are marked by the visible consequences of the Zika virus: birth defects, such as microcephaly, are at the forefront of the collective imaginary. That imaginary has haunted all women who intended to get pregnant during the Zika epidemic. Some researchers have observed that women, regardless of age, social class, ethnic or religious background, had to face fear and to implement individual strategies to manage risk on their own initiative and according to the information they could rely on (Diniz 2016; Marteleto et al. 2017).
Conclusion
As the Zika epidemic was growing, many researchers from the Global South and the Global North turned their attention to the management of the crisis and the consequences of the health emergency. Specifically, the women who gave birth to babies with microcephaly, often underprivileged women from the northeast region of Brazil, were put on the agenda of scholars in biomedicine and social sciences (see Reis-Castro 2019; Lira and Prado 2020). It has since been a huge concern for social workers, healthcare professionals, and social scientists—with good reason, as many of these mothers have been abandoned by their partners and continue to struggle to access specific health and childcare for their severely disabled children (Williamson 2020; Lustosa 2019; Lima and Fleischer 2020).
Technologies of reproduction (in a broad sense, including contraception, family planning, abortion, and ART), maternal and healthcare politics, and gender issues are obviously at the core of the debate about the Zika epidemic. However, in my understanding, the case study of ART is a grey zone of investigation, and one on the fringes of the main social consequences of the Zika epidemic. In this article, I have argued that this case is useful to understand how the Zika epidemic was managed in Brazil by looking at the potentiality of pregnancies and prospective babies for (infertile) couples—that is, the biopolitics of reproduction as a whole, and not only at the risk of child disability. More broadly, it calls into question the substantive issue of ‘stratified reproduction’ (Ginsburg and Rapp 1995; Inhorn 2015) and the expression of the intrinsic inequalities of access to reproductive rights and technologies in the context of an epidemic. As many studies on reproductive ageing state, the idea of a ‘natural’ biological clock in the field of ART is closely linked to the construction of gender-based female infertility (Vialle 2014; Löwy 2009) along with the idea of a ‘choice’ of being a biological older mother (Baldwin et al. 2014). In many ways, the Zika epidemic came to challenge both the timing of reproductive ageing and the choice of getting pregnant.
A last word as this text is finalised during the COVID-19 pandemic. It may be too soon to analyse properly the consequences of the current pandemic but one thing is certain: when it comes to healthcare, lessons were not learned after the Zika epidemic. This novel pandemic sheds light once again on the global inequalities of access to healthcare, reliant on national private or public health systems (but also on access to water, soap, and of course, to a home). It has also called into question the policy of testing—including who must be tested and for what purpose.
Particularly in terms of the biopolitics of reproduction, health recommendations regarding the COVID-19 outbreak in Brazil are repeating the Zika virus epidemic history: ‘Do not get pregnant’ [Não engravidem!] advised the Ministry of Health (Anis 2021)—in a way relieving, again, its accountability for reproductive health. In France, where I am located, access to sexual and reproductive healthcare has been constrained for several months, during which it was considered ‘non-essential’: beginning with abortion services (Condomines 2020), ART (Cabut 2020), and prenatal care—including the prohibition of partners from attending consultations and sometimes even childbirth (Le Journal des Femmes 2020). It may be worthwhile for anthropologists to look at the way in which health emergency policies act and how they reveal the structure of biopolitics in times of health crisis and epidemic.
Acknowledgements
I would like to give special thanks to Ilana Löwy and Luísa Reis Castro for their insightful comments on earlier versions of this article. I also thank sincerely MAT’s editors and the anonymous reviewers for their careful reading and valuable advice. My post-doctoral research on the social uses of biomedical technologies and reproductive practices during the Zika epidemic, in addition to the two periods of fieldwork in Brazil, have been supported by funding from the Institute for Research and Innovation in Society (IFRIS, France) and hosting by the Centre for Population and Development (CEPED, Université Paris Descartes, IRD).
About the author
Helena Prado is an anthropologist, whose work aims to understand and analyse bodily practices and representations. Her PhD thesis ‘The Other Face’ (2016) at the Ecole des Hautes Etudes en Sciences Sociales (France), explored the dynamics of cultural identifications and representations of the body of Japanese-Brazilians in São Paulo (Brazil). She received two postdoctoral fellowships (Institute for Research and Innovation in Society, Paris, 2017–18; Excel Project, Institute for Social Sciences, Lisbon, 2019–20) that gave her the opportunity to engage in the study of biopolitics and the use of biotechnologies, particularly concerning representations of the female body and reproductive and sexual life in the field of health. She is currently a lecturer at the Institute of Ethnology, University of Strasbourg, France, based in the Lab for interdisciplinary cultural studies–LinCS.
Footnotes
A measure announced at the beginning of 2016 for the distribution of mosquito repellents to women from very low socioeconomic backgrounds (who benefit from the State's Bolsa família programme) did not take effect until March 2017, once the epidemic had passed. This was more than a year after the announcement of the measure, and almost at the end of the summer—the riskiest period for vector-borne diseases (Prado 2018, 82). The failure of this measure combined with the high cost of efficient repellent (around US$20 per bottle), not to mention shortages of repellent in the main cities, gives an idea of the consequences of promoting mosquito bite prevention as the main health prevention recommendation.↩︎
The presence of the virus has mostly been detected in semen, where it has been reported to remain for nine months after infection. It has also been detected in urine, blood, vaginal secretions, saliva, and breast milk—even though there is as yet no evidence of potential infection after primary viremia, i.e. after the initial spread of the virus in the blood from the first site of infection. In other words, if the primary infection happens before the woman gets pregnant, no evidence has shown that the mother could transmit the disease in utero later on (see e.g., Mead et al. 2018).↩︎
Congenital Zika syndrome is identified as a ‘distinct pattern of birth defects and disabilities’ (CDC 2021b).↩︎
See discussions on the financial costs of Zika testing in Carvalho et al. (2016) and de Souza et al. (2016).↩︎
I especially thank Ilana Löwy for pointing out so clearly the issue of ‘various temporalities’ when reading a previous version of this article.↩︎
Congenital infections caused by toxoplasmosis, rubella, cytomegalovirus, herpes and other agents, commonly referred to by the acronym TORCHS.↩︎
References
Agência Nacional de Vigilância Sanitária – Anvisa. 2016. ‘Critérios técnicos para o gerenciamento do risco sanitário de células, tecidos germinativos e embriões humanos para uso terapêutico frente aos casos de infecção por vírus Zika no Brasil’. Nota Técnica n.º008/2016/GSTCO/GGMED/DIARE/ANVISA.
ANIS Instituto de Bioética. 2021. ‘Incapaz de cuidar da vida, governo só diz: “Não engravidem!”’.https://www.facebook.com/AnisBioetica/posts/5399040643502157.
Araújo Filho, Edilberto, Cássio Leão Fácio, Ligiane Alves Machado-Paula, Mariana Angelozzi de Oliveira, Ciro Dresch Martinhago, Leonardo Previato Araújo, and Lígia Fernanda P. Araújo. 2019. ‘Case Report of Zika Virus during Controlled Ovarian Hyperstimulation: Results from Follicular Fluid, Cumulus Cells and Oocytes’. JBRA Assisted Reproduction 23 (2): 172–74. https://doi.org/ 10.5935/1518-0557.20180081.
Atkinson, Barry, Pasco Hearn, Babak Afrough, Sarah Lumley, Daniel Carter, Emma J. Aarons, Andrew J. Simpson, Timothy J. Brooks, and Roger Hewson. 2016. ‘Detection of Zika Virus in Semen’. Emerging Infectious Diseases 22 (5): 940. https://doi.org/10.3201/eid2205.160107.
Bahamondes, Luis, Moazzam Ali, Ilza Monteiro, and Arlete Fernandes. 2016. ‘Contraceptive Sales in the Setting of the Zika Virus Epidemic’. Human Reproduction 32 (1): 88–93. https://doi.org/10.1093/humrep/dew310.
Baldwin, Kylie, Lorraine Culley, Nicky Hudson, and Helene Mitchell. 2014. ‘Reproductive Technology and the Life Course: Current Debates and Research in Social Egg Freezing’. Human Fertility 17 (3): 170–79.
https://doi.org/10.3109/14647273.2014.939723.
Borges, Edson Jr., Daniela Paes de Almeida Ferreira Braga, Bianca Ferrarini Zanetti, Amanda Souza Setti, Rodrigo Rosa Provenza, and Assumpto Iaconelli Jr. 2017. ‘Zika Virus Outbreak – Should Assisted Reproduction Patients Avoid Pregnancy?’ JBRA Assisted Reproduction 21 (3): 208–11. https://doi.org/10.5935/1518-0557.20170040.
Cabut, Sandrine. 2020. ‘Coronavirus : les demandes d’IVG à la baisse, les activités de PMA à l’arrêt’. Le Monde, March 31, 2020.
CDC. 2021a. ‘Pregnant Women and Zika’.
https://www.cdc.gov/pregnancy/zika/protect-yourself.html.
CDC. 2021b. ‘Congenital Zika Syndrome & Other Birth Defects’.
https://www.cdc.gov/pregnancy/zika/testing-follow-up/zika-syndrome-birth-defects.html.
Condomines, Anaïs. 2020. ‘La pratique des IVG va-t-elle être perturbée pendant la crise sanitaire ?’. Libération, March 20, 2020.
Correa, Marilena, and Löwy, Ilana. 2020. ‘Reproductive technology and social justice: a view from Brazil’. Reproductive BioMedicine Online 41 (6): 1151–53. https://doi.org/10.1016/j.rbmo.2020.11.003.
de Carvalho, Bruno R., Paulo F. Taitson, Karina S. A. G. Brandão, Rui Alberto Ferriani, Hitomi M. Nakagawa, Adelino A. Silva, and Joaquim R. C. Lopes. 2016. ‘Reproductive Planning in Times of Zika: Getting Pregnant or Delaying Plans? The Opinion of the Brazilian Society of Assisted Reproduction Committee – a Basis for a Bioethical Discussion’. JBRA Assisted Reproduction 20 (3): 159–64. https://doi.org/10.5935/1518-0557.20160034.
de Souza, Maria do Carmo B., Veronica Raupp, Fernanda Sobrinho, Mariana Menezes, Tatiana R. Panaino, Maria A. Tamm, Ana C. A. Mancebo, Ana L. R. Costa et al. 2016. ‘Zika Virus and Assisted Reproductive Technology: To Test or Not to Test, That Is the Question. Is it an Unnecessary Cost? The First Two Months of Mandatory Testing in an Outbreak Area in Rio de Janeiro, Brazil’. JBRA Assisted Reproduction 20 (4): 195–99. https://doi.org/10.5935/1518-0557.20160038.
Diaz-Quijano, Fredi Alexander, and Alexandre Dias Porto Chiavegatto Filho. 2017. ‘Reduction of the Birth Rate in São Paulo: A Probable Effect of the Panic Caused by the Zika-associated Microcephaly Epidemic’. Annals of Epidemiology 27 (9): 616–17. https://doi.org/10.1016/j.annepidem.2017.08.009.
Diaz-Quijano, Fredi Alexander, Daniele Maria Pelissari, and Alexandre Dias Porto Chiavegatto Filho. 2018. ‘Zika-Associated Microcephaly Epidemic and Birth Rate Reduction in Brazilian Cities’. American Journal of Public Health 108 (4): 514–16. https://doi.org/10.2105/AJPH.2017.304260.
Diniz, Débora. 2016. Zika: Do Sertão Nordestino à Ameaça Global. Rio de Janeiro: Civilização Brasileira.
Diniz Debora, Marcelo Medeiros, and Alberto Madeiro. 2017. ‘Brazilian Women Avoiding Pregnancy During Zika Epidemic’. BMJ Sexual & Reproductive Health 43 (1): 80. https://doi.org/10.1136/jfprhc-2016-101678.
D’Ortenzio, Eric, Sophie Matheron, Xavier de Lamballerie, Bruno Hubert, Géraldine Piorkowski, Marianne Maquart, Diane Descamps, Florence Damond, Yazdan Yazdanpanah, and Isabelle Leparc-Goffart. 2016. ‘Evidence of Sexual Transmission of Zika Virus’. New England Journal of Medicine 374: 2195–98. https://doi.org/10.1056/NEJMc1604449.
Ginsburg, Faye D., and Rayna Rapp, eds. 1995. Conceiving the New World Order: The Global Politics of Reproduction. Berkeley, CA: University of California Press.
Guedes de Mello, Anahí, and Gabriela Rondon. 2020. ‘Feminism, Disability, and Reproductive Autonomy: Abortion in Times of Zika in Brazil’. Somatosphere (blog), February 17, 2020. http://somatosphere.net/2020/abortion-zika.html.
Inhorn, Marcia C., and Pasquale Patrizio. 2015. ‘Infertility Around the Globe: New Thinking on Gender, Reproductive Technologies and Global Movements in the 21st Century’. Human Reproduction Update 21 (4): 411–26. https://doi.org/10.1093/humupd/dmv016.
Le Journal des Femmes. 2020. ‘Grossesse et covid : suivi, échographies, chômage partiel’. Le Journal des Femmes, November 16, 2020.
Lima, Flávia, and Soraya Fleischer. 2020. ‘Nourishment Dilemmas: The Complex Science of Caring for Children with CZVS’. Somatosphere (blog), February 24, 2020. http://somatosphere.net/2020/care-children-czvs.html.
Lira, Luciana Campelo and Helena Prado. 2020. ‘“Nossos filhos não são cobaias”: objetificação dos sujeitos de pesquisa e saturação do campo durante a epidemia de Zika’. Ilha Revista de Antropologia 22 (2): 96–131. https://doi.org/10.5007/2175-8034.2020v22n2p96.
Löwy, Ilana. 2009. ‘L’âge limite de la maternité : corps, biomédecine, et politique’. Mouvements 59 (3): 102–12. https://doi.org/10.3917/mouv.059.0102.
Lustosa C. Alves, Raquel. 2019. ‘In the Search of a School for Nancy: Stories of Disability, Inclusion and Care’. Somatosphere (blog), December 9, 2019. http://somatosphere.net/2019/school-for-nancy-zika.html/.
Marteleto, Letícia J., Abigail Weitzman, Raquel Zanatta Coutinho, and Sandra Valongueiro Alves. 2017a. ‘Women’s Reproductive Intentions and Behaviors During the Zika Epidemic in Brazil’. Population and Development Review 43 (2): 199–227. https://doi.org/10.1111/padr.12074.
Marteleto, Letícia J., Abigail Weitzman, and Raquel Zanatta Coutinho. 2017b. ‘Women's Reproductive Intentions and Behaviors Amidst the Zika Epidemic in Brazil’. Paper presented at the IUSSP XXVIII International Population Conference, Cape Town, 3 November 2017.
Mead, Paul S., Nisha K. Duggal, Sarah A. Hook, Mark Delorey, Marc Fischer, Dana Olzenak McGuire, Heidi Becksted et al. 2018. ‘Zika Virus Shedding in Semen of Symptomatic Infected Men’. New England Journal of Medicine 378 (15): 1377–85. https://doi.org/10.1056/NEJMoa1711038.
Mlakar, Jernej, Misa Korva, Nataša Tul, Mara Popović, Mateja Poljšak-Prijatelj, Jerica Mraz, Marko Kolenc et al. 2016. ‘Zika Virus Associated with Microcephaly’. New England Journal of Medicine 374 (10): 951–58.
https://doi.org/10.1056/NEJMoa1600651.
Musso, Didier, Claudine Roche, Emilie Robin, Tuxuan Nhan, Anita Teissier, and Van-Mai Cao-Lormeau. 2015. ‘Potential sexual transmission of Zika virus’. Emerging Infectious Diseases 21 (2) : 359–61. https://doi.org/10.3201/eid2102.141363.
Oliveira Melo, A. S., G. Malinger, R. Ximenes, P. O. Szejnfeld, S. Alves Sampaio, and A. M. Bispo de Filippis. 2016. ‘Zika Virus Intrauterine Infection Causes Fetal Brain Abnormality and Microcephaly: Tip of the Iceberg?’. Ultrasound in Obstetrics & Gynecology 47 (1): 6–7. https://doi.org/10.1002/uog.15831.
Prado, Helena. 2018. ‘Ce que l’épidémie du virus Zika dévoile des droits reproductifs et sexuels au Brésil’. Cahiers Des Amériques Latines: Dossier Naissances et Politiques Publiques 88–89: 79–96. https://doi.org/10.4000/cal.8855.
Reis-Castro, Luísa. 2019. ‘Histórias of Zika’. Somatosphere (blog), December 2, 2019. http://somatosphere.net/2019/historias-of-zika.html/.
Vialle, Manon. 2014. ‘L’«horloge biologique» des femmes : un modèle naturaliste en question. Les normes et pratiques françaises face à la croissance de l’infertilité liée à l’âge’. Enfances, Familles, Générations 21: 1–23. https://doi.org/10.7202/1025957ar.
Williamson, Eliza. 2020. ‘Against Forgetting: Telling Stories After Zika’. Somatosphere (blog), January 6, 2020. http://somatosphere.net/2020/telling-stories-zika.html/.
World Health Organization. 2016a. ‘Prevention of sexual transmission of Zika virus: interim guidance update’. https://apps.who.int/iris/handle/10665/204421.
World Health Organization. 2016b. ‘WHO Statement on the First Meeting of the International Health Regulations (2005) (IHR 2005) Emergency Committee on Zika Virus and Observed Increase in Neurological Disorders and Neonatal Malformations’. 1 February 2016. https://www.who.int/news/item/01-02-2016-who-statement-on-the-first-meeting-of-the-international-health-regulations-(2005)-(ihr-2005)-emergency-committee-on-zika-virus-and-observed-increase-in-neurological-disorders-and-neonatal-malformations