Vision is central to the apprenticeship of trainees undertaking ophthalmology residency training. As clinicians who diagnose and treat diseases of the eye, ophthalmologists build their professional identities around the mission of safeguarding their patients’ sight. At the same time, ophthalmologists rely on their own vision as they peer into the eye to detect subtle signs of disease. Based on an extended ethnography of an ophthalmology residency programme, as well as autoethnographic analysis of ophthalmology training, this article explores how novice trainees learn to view the eye by considering two fundamental examination techniques. The first is slit lamp biomicroscopy, where a table-mounted microscope is used to view ocular structures in fine detail. The second is binocular indirect ophthalmoscopy, where examiners view the retina using a head-mounted instrument in conjunction with handheld lenses. Rather than framing visual interpretation as a cognitive exercise in identifying pathology, I instead consider these techniques as embodied practices where trainees must discipline their movement, attention, and use of instrumentation to make the eye visible. This process of embodiment, in turn, unfolds within a broader terrain of affects as trainees marvel at what they behold, yearn to see more, and fear the limitations of their own vision while they learn to perform challenging examination manoeuvres. Situating the ophthalmic examination in its embodied and affective contexts illustrates the sensibilities that ophthalmology residents come to inhabit during their apprenticeship and which undergird the visual expertise of ophthalmologists.
Eyes in Sight
Embodiment, Affect, and Learning to See in Ophthalmology
—
Abstract
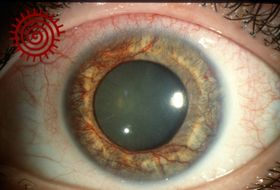 Abnormal proliferation of blood vessels on the surface of the iris, as seen during an eye examination. Image by James Gilman. In the Moran CORE collection, CC BY-NC-ND 4.0.
Abnormal proliferation of blood vessels on the surface of the iris, as seen during an eye examination. Image by James Gilman. In the Moran CORE collection, CC BY-NC-ND 4.0.
Introduction
Sight is a fundamental concern in ophthalmology, the branch of medicine that treats diseases of the eye and visual system. As clinicians whose professional lives are built around the measurement and preservation of vision, ophthalmologists think a great deal about what other people see. Yet for ophthalmologists, the clinical encounter is also dependent on their own vision. All parts of the patient’s eye must be inspected visually, whether through optical instruments that illuminate the organ’s intricate structures or via imaging technologies that capture the eye and enable its hidden depths to be seen. When ophthalmologists perform surgery, they peer through microscopes and other magnifying lenses at the delicate tissues they manipulate. In short, ophthalmologists engage with the vision of their patients against the backdrop of their own sensory disciplining.[1]
From early in my training as a physician-anthropologist, the figure of an ophthalmologist training her gaze onto a patient’s eyes sparked an insistent curiosity about the multiple ‘visions’ that are at stake in this profession. At one level, vision in ophthalmology is an object of clinical scrutiny that can be both measured and optimised. More implicitly, however, vision is imbued with moral status as a lived experience that can be enjoyed, depended upon, yearned for, and mourned as it slips away. What effect does it have on ophthalmologists to confront fragile and disordered embodiments of their patients’ vision while they work in a field where expertise is embodied through visual skill? How is vision represented in language and shared, whether in medical documentation or in conversations among doctors, patients, teachers, students, and colleagues? Thinking along the lines of Mol’s (2002) classic account of disease and its ontological multiplicity, how is vision enacted across different contexts in ophthalmology? As I later found, exploring the ‘visions’ of ophthalmology became fertile terrain for thinking about many themes: the historical and social constitution of the senses; the marshalling of technology and media to create new modes of viewing; the forms of power and authority generated through disciplined perspective; and the possibilities for intersubjective exchange that are created—or excluded—as ophthalmologists discuss vision with patients and share visual information with their peers.
As it happens, my plans for researching ophthalmology coalesced around the time I took leave from graduate studies to start medical school. Although most American medical students receive relatively little exposure to ophthalmology—creating an especially steep learning curve for beginner residents when entering this largely unfamiliar world—the early glimpses I had into the specialty created a durable fascination with the eye and the work of ophthalmologists. When I later paused my medical training to begin fieldwork on ophthalmology, I realised that the awe and wonder I had felt at first viewing the eye was an experience I shared with many of the trainees and practitioners who were taking part in my research.[2] As foretold by friends and advisors who withstood my earliest musings about ophthalmology, I now find myself, years after the completion of my dissertation, amid my own training in this specialty. The stories and experiences that were relayed to me by ophthalmologists during fieldwork continue to reverberate during my own professional formation as an ophthalmology resident.
This article considers early moments in ophthalmology training where medical students and residents begin peering into and making sense of the eye. Here I will focus on two emblematic ‘tools of the trade’ that are used by ophthalmologists to spot signs of ophthalmic disease: slit lamp biomicroscopy, where a table-mounted microscope is used to examine eye structures in fine detail, and binocular indirect ophthalmoscopy, where practitioners view the retina using a head-mounted device in combination with handheld lenses. Although this instrumentation may be familiar to readers from their own experiences as patients in ophthalmology or optometry clinics, using them adeptly is a significant challenge for junior trainees, who struggle to consistently identify the details that they are tasked with seeing. Rather than framing these diagnostic techniques as ‘competencies’ to be mastered by trainees—borrowing from the parlance of medical educators who seek to measure and optimise the transmission of clinical knowledge and skills—I instead consider how learning these ophthalmic examination techniques transforms the embodied subjectivities of burgeoning ophthalmologists (Frank et al. 2010).
One aim of this article is to extend existing accounts of embodiment, sensory calibration, and expertise in biomedicine to a field that has garnered little attention from scholars in medical anthropology and science studies.[3] Examining eye care professionals and their training creates opportunities to think afresh about these well-established theoretical concerns. A further goal of this project is to illustrate a style of partially autoethnographic analysis where clinician-anthropologists write at the interstices of their disciplines. Cultivating these accounts could, in turn, provide a useful body of literature with which to encourage clinicians in wide-ranging fields to reflect on their everyday experiences and emplacement as healthcare workers.
Embodying the eye
Vision holds a complicated status in Western intellectual traditions, being either glorified as the purest and most immediate way of knowing the world or maligned as a technology of surveillance and domination (Foucault 1980; Foster 1988; Jay 1993; Jutte 2005). Crary (1990) chronicles the rupture of classical philosophies of observation, wherein the observer was a passive and faithful recipient of sensation, and the rise of new critiques in the nineteenth century that framed vision as a function of the subject’s perspective and physiological attunement. This crisis of subjectivity, Crary argues, ‘coincided with the making of the observer into a subject of new knowledge and new techniques of power’ (idem, 79). Jay (1993) reviews a range of twentieth-century critiques that interrogate the ‘scopic regime’ of disembodied, totalising forms of vision. Heidegger (1977), for instance, denounces the idea of an abstracted, monocular viewer as a technique of violence and conquest, seeking instead a model of vision that is multiple and always aware of its context. In a similar vein, Haraway (1988) insists on recognising the situated nature of vision rather than acquiescing to a ‘conquering gaze from nowhere’ with the ‘power to see and not be seen, to represent while escaping representation’ (581).
These lines of critique become especially salient in the study of expert vision, where conceits of objectivity and authority have long been recognised as conditioning the transformation of sensation into fact.[4] One avenue for unsettling these presumptions has been to consider vision as a cultural practice that is contingent on the subjectivities of experts, on norms for designating certain visual media as truthful, and on the social signification of certain visual interpretations as accurate and trustworthy. To this end, scholars in anthropology and related fields have turned toward a variety of professional groups to characterise how visual expertise is constituted (Burri and Dumit 2008). Early work in science studies, for instance, describes how scientists use visualisation to create and analyse their objects of study (Knorr-Cetina and Amman 1990; Lynch 1990), while Goodwin (1994) and Jasanoff (1998) both provide influential accounts of the ways visual expertise is performed and marked. Subsequent work has investigated the crucial role of scientists’ sensory engagement with visual models and media (Lynch 1990; Masco 2004; Myers 2015; Vertesi 2015).
In the realm of biomedicine, radiology has been a natural venue for the extension of these inquiries into expert vision (Simon 1999; Dumit 2004; Joyce 2010; Burri 2013). Saunders (2008) provides an especially rich analysis that frames radiological interpretation not merely as an exercise in pattern recognition, but as a practice driven by the emotions of radiologists themselves. Curiosity and intrigue become part of the ‘fabric of detection’ in radiology as practitioners puzzle over images, either finding enjoyment as they successfully sleuth through a case or meeting consternation when they fail to decipher what lies hidden within images (idem, 143). Such work can be situated within broader histories of vision and subjectivity. In the German tradition of aesthetics, for instance, Kant ([1790] 2000) explores emotional states that are elicited by encounters with the beautiful and the sublime, while Schiller ([1795] 2004) makes more expansive claims about the ways such encounters influence our capacity for moral reasoning. In a much later context, members of the Frankfurt School examined the role of visual media in crafting new forms of political consciousness (Benjamin 1968; Adorno 1997).
In keeping with this literature, my approach to ophthalmology has remained attentive to the role of affect in everyday visual practice and in the transformation of trainees into visual experts. Here my use of ‘affect’ as an analytical category departs from Massumi’s (2002) notion of pre-cognitive intensity, which Leys (2011) critiques for its perpetuation of untenable mind–body dualisms (see also Martin 2013). More in keeping with Mazzarella’s (2009) framing of affect, I employ this concept as a shorthand for tacit emotional states and how they are constituted through social life.
Another useful analytic framework for understanding the situatedness of vision—and a longstanding concern in anthropology—is that of embodiment (Lock and Farquhar 2007). Addressing the sense of hearing, Boas (1889) suggests that individuals fail to detect differences between unfamiliar phonemes because what we hear is conditioned by the languages we speak. Mauss (2007) describes cultural variations in ‘techniques of the body’, meaning the ways individuals carry themselves, employ gesture, and perform physical acts. In the phenomenological tradition, Merleau-Ponty (2002) frames sensation and consciousness as states of experience that inherently derive from, and necessarily reside within, the lived body.[5] Bourdieu (1977) later shifted attention from experience to practice in his treatment of habitus, exploring how embodied dispositions are transmitted in social life. In a more contemporary formulation of habitus that returns to the concept’s Aristotelian origins, Mahmood (2005) considers religious pedagogy in a women’s Islamist movement and explores how emotional relationships to the divine (e.g., love of God, hope for closeness to God, fear of God’s wrath) are essential in the constitution of a pious subject.
Elsewhere, giving careful consideration to literature on embodiment and the senses, Prentice (2012) offers a rich ethnography of biomedical apprenticeship that examines anatomy education in medical school as well as the postgraduate training of surgery residents and fellows. Her analysis of each setting demonstrates tacit calibrations of ethics, affect, and embodied practice that are inseparable from—and often constitutive of—the transmission of knowledge and technical skills that medical educators openly expect trainees to acquire. Although vision plays a significant role in these training contexts, Prentice avoids privileging sight over other modes of perception such as hearing and haptics; her approach is a conscious intervention into the predominance of vision in Western intellectual traditions, intended to make space for studying the full range of sensory and bodily practices in medical education (see also Rice 2013; Hammer 2018). Along similar lines, Fountain (2014) uses the conceptual framework of rhetoric to explore relationships between material objects, discourse, and the senses in anatomy education.
The ophthalmic examination
The arrangement of an ophthalmology clinic visit will vary according to the ophthalmologist’s subspecialty and the issue being addressed, but most encounters will follow a typical sequence. It begins with a discussion about the patient’s symptoms—whether visual disturbances, pain in the eyes, or other complaints—before transitioning to measurement of the patient’s visual acuity using eye charts and the mapping of the patient’s visual field (most readily performed by instructing patients to count the examiner’s fingers when held at the edges of their peripheral vision). After this information is gathered, attention usually turns toward visual inspection of the eyes through the testing of pupillary reflexes, an assessment of eye movement and alignment, and an inspection of the appearance or position of the eyelids.
The encounter will then usually progress to more detailed examination of the eye using the slit lamp, which essentially comprises a moveable microscope and light source mounted together on a tabletop. The slit lamp provides the examiner with a magnified view of the eyelids and structures towards the front of the eye, such as the clear cornea, the pigmented iris, and the eye’s internal lens (where cataracts form). As a thin, slit-shaped light beam is used to examine these structures, the whole contraption is metonymically named the ‘slit lamp’. At one end of the device, there is a rest for the patient’s chin and forehead so that they can comfortably position their head during the examination. This has the added benefit of stabilising the patient’s head, thereby minimising movements that might disrupt the examination. At the other end of the slit lamp are two eyepieces through which the examiner will peer. The patient and examiner are facing each other with the slit lamp placed between them, while the examiner uses a joystick to move the microscope into the desired position.

Figure 1. Slit lamp biomicroscopy examination. Source: National Institutes of Health, 2006, free of copyright (https://www.flickr.com/photos/nihgov/27373487700/).
At teaching institutions, many slit lamps are equipped with an additional eyepiece that protrudes like a telescope from the examiner’s end of the device. This ‘teaching scope’ allows learners to passively watch the exam, albeit without being afforded the same depth perception enjoyed by the main examiner, who views the eye through two eyepieces.
The technique for using the slit lamp to conduct an examination varies by setting but typically unfolds along the lines of this scenario, which I observed during my fieldwork (while myself making use of the teaching scope):
The resident turns on the slit lamp’s light and adjusts the beam so that it illuminates a large patch of the patient’s right eye. By convention, she begins by examining the eyelashes and the surface of the eyelids. She asks the patient to look left and right while she inspects the surface of the eye. She then uses a finger to gently pull apart the upper and lower lids, which exposes more of the eye’s surface in addition to the inside surfaces of the lids.
Next, the resident narrows the beam of light into a thin slit. She casts the beam onto the cornea and moves the light source so the slit travels across its entire surface; the technique allows her to gauge the thickness of the cornea and even distinguish among its layers. She makes another slight change to the beam as she examines the iris as well as the chamber of clear fluid between the cornea and the iris. She aims the beam into the pupil to inspect the lens for signs of cataract, then pushes the microscope forward to bring the front surface of the vitreous—a clear jelly-like substance that fills the back chamber of the eye—into focus.
Finally, the resident turns towards the desk and takes a small, round lens in her hand, about 2.5 cm in diameter. She places the lens directly in front of the patient’s eye and returns to look again through the slit lamp’s eyepieces. As she pulls back on the slit lamp’s joystick, a small patch of the retina is brought into focus. ‘Look at my left ear, please’, she instructs the patient. As the patient shifts his gaze, the optic disc comes into view; this is a pale ‘button’ of tissue where retinal nerves converge and leave for the brain, and through which small arteries and veins also pass.
The resident repeats this sequence on the left eye before asking the patient to sit back in the chair. She switches off the light source on the slit lamp, turns a small screw at the base of the microscope to lock it into place, and pushes the device away from the patient.
In essence, basic use of the slit lamp requires examiners to manage the perspective of the microscope—not only moving up or down and left or right, but also toward or away from the patient to adjust focus—while simultaneously controlling the angle, shape, and intensity of the light beam so that the structures of the eye can be appropriately seen.

Figure 2. Close-up of the slit lamp examination. Source: United States Air Force, 2012, free of copyright (https://commons.wikimedia.org/wiki/File:Luke_AFB_eye_exam.jpg).
Additional instrumentation can be incorporated into the slit lamp examination, as in the above vignette where a small lens is held by the examiner in front of the patient’s eye; the position of this lens and the focus of the microscope must be carefully adjusted to see structures such as the retina and optic nerve.
Binocular indirect ophthalmoscopy, the other fundamental technique that ophthalmology residents must learn, allows for more detailed examinations of the retina. Two pieces of equipment are necessary here. The first is a head-mounted ophthalmoscope, which consists of a light source and two eyepieces that are secured to the examiner using adjustable straps. Before using the device, users must carefully adjust the position of the light beam so that it falls within the field of vision for each of their eyes. The second piece of equipment is a larger handheld lens than is used with the slit lamp, which the examiner places in front of the patient’s eye to bring the retina into focus. The principal advantage of this ophthalmoscope is that it gives a wide-field view of the retina, provided that the patient’s eye, the handheld lens, and the examiner’s head have been precisely aligned.

Figure 3. Binocular indirect ophthalmoscopy. Source: National Eye Institute, National Institutes of Health, CC BY 2.0 licence. (https://www.flickr.com/photos/nationaleyeinstitute/7544456856/).
Using this device requires that dilating eye drops be administered, since a constricted pupil would not provide adequate room for light to pass through. After the patient’s eyes have been dilated, the examination typically unfolds as follows:
The resident turns on the ophthalmoscope’s light, picks up his lens, and walks to the right side of the patient. He stretches out his hand and places the lens in front of the patient’s eye; grasping the lens with his thumb and index finger, he rests his other fingers on the patient’s brow while making subtle movements to bring the retina into view. ‘Look up for me’, the resident requests with a slight upward inflection. He continues to direct the patient to look in every direction—to the right, down, and left—always moving the lens in the instructed direction as a cue for the patient before placing it back in front of the eye. Finally, the resident asks the patient to look ‘right at the light’ while he examines the macula, the portion of the retina that is most sensitive to light. ‘Great’, the resident says as he shifts his posture to examine the other eye in the same manner. When finished, he turns back to the desk to add his findings to the chart and to a form which includes two large circles, within which he draws basic features of the retina.
The naming of the binocular indirect ophthalmoscope (or ‘the indirect’, as it is called in ordinary practice) designates important differences between this device and other instruments used to view the back of the eye. Unlike ophthalmoscopes one might find on the wall of a primary care physician’s office, which consist of only one eyepiece that the examiner must hold within a few inches of the patient, the binocular indirect ophthalmoscope provides a wider-field view of the retina. Furthermore, its two eyepieces allow the user a sense of depth which is useful for gauging the height of lesions, such as blood suspended in front of the retina or tumours that protrude toward the centre of the eyeball. The term ‘indirect’ references the optical properties of the device, which have the downside of flipping and inverting the image perceived by the examiner—that is, right becomes left and up becomes down.
 It takes novice residents
months to learn to use this ophthalmoscope correctly, in large part
because obtaining a view of the retina requires the precise and
simultaneous alignment of several variables: the light beam and
eyepieces must be appropriately positioned; the examiner’s head must be
moved into place and kept still; the handheld lens must be stabilised so
that it can be manipulated in five directions of movement (left/right,
up/down, forward/back, and the vertical and horizontal tilting movements
of pitch and yaw); and finally the patient’s head and eye must be
adjusted so that the examiner can see specific regions of the
retina.
It takes novice residents
months to learn to use this ophthalmoscope correctly, in large part
because obtaining a view of the retina requires the precise and
simultaneous alignment of several variables: the light beam and
eyepieces must be appropriately positioned; the examiner’s head must be
moved into place and kept still; the handheld lens must be stabilised so
that it can be manipulated in five directions of movement (left/right,
up/down, forward/back, and the vertical and horizontal tilting movements
of pitch and yaw); and finally the patient’s head and eye must be
adjusted so that the examiner can see specific regions of the
retina.
Figure 4. Approximation of the view obtained with a binocular indirect ophthalmoscope, using a smartphone camera. Source: Nazari Khanamiri, Nakatsuka, and El-Annan (2017), CC BY-NC-ND 3.0 licence.
Manoeuvring the handheld lens is the hardest aspect of the technique for residents to master, since it must be placed in precisely the correct spot to obtain a view. A few millimetres to the side, and the resident might be looking at the patient’s cheek instead of the eye. If the lens is held too close to the patient, or too far away, the resident will not achieve the full, magnified view that makes the ophthalmoscope useful. The view can be similarly compromised if the distance between the lens and the resident’s head is too great or too small. Examiners must often stretch out their arms and lean back their heads to put enough distance between themselves and their patients. This, too, is a counterintuitive practice of visual coordination; generally when one wants to get a better look at something, the first impulse is to lean in and peer closer at it.
In the sections that follow, I consider a range of affects that arise as ophthalmology residents enter the profession and embody these techniques for examining the eye. For these beginner residents, excitement about beholding the eye is tempered by a range of frustrations and anxieties as they struggle to obtain a proper view.
Struggling to see
The slit lamp and indirect ophthalmoscope make life challenging for ophthalmology trainees who are beginning their training. These frustrations often start before residency, when medical students first arrive in the ophthalmology clinic. Unlike specialties such as internal medicine, where students spend two years learning the fundamentals of the field and can thus meaningfully participate in patient care, ophthalmology rotations provide few opportunities for students to do or see anything. Students who are not interested in ophthalmology might spend two to four weeks standing in the corner of the examination room as silent spectators; if they are given any responsibilities these will usually be limited to gathering patient histories, checking visual acuity, examining eye movements, or evaluating the size and movement of the pupils. When residents and teaching staff discover important findings at the slit lamp, they will sometimes hold the instrument in place so medical students can quickly peek through the eyepieces; frequently, though, subtle movements of the slit lamp and of the patient’s gaze mean the finding can no longer be seen.
Trainees fare much better when slit lamps have teaching scopes, although it is still often difficult for them to make sense of what they see. One resident, who went to medical school having a prior interest in ophthalmology, recounted his disappointment when shadowing an ophthalmologist for a day as a first-year student:
I could not see anything … they’re trying to show me, they’re moving the slit lamp around, there’s a teaching scope so I’m looking at exactly what they’re looking at, and everything looks so minuscule … I can’t appreciate any of it. I mean they’re all small things. They’re like ‘Oh, do you see meibomian gland disease?’ or ‘They have blepharitis’, or ‘The cornea has punctate epithelial erosions’, or ‘The lens is 1+ nuclear sclerosis’. Yeah, the whole time you’re shaking your head like, ‘Ahh, yes yes yes’. And after the afternoon there, I was so distraught. I was like, ‘This is horrible. I don’t think I wanna do this at all. I can’t see anything.’
When attending ophthalmologists ask students to describe and interpret what they have seen during an examination there is a peculiar mix of elation and terror: the chance to perform one’s burgeoning expertise is tinged with the possibility of failure.
While motivated medical students can conduct some aspects of the slit lamp examination, performing indirect ophthalmoscopy is more challenging as the views it provides of the retina are fleeting and findings are often difficult to interpret. As a result, most ophthalmology residents start their training with very little experience using this device. During the early months of their training, residents described how they attempted to get a feel for the instrument by using it to examine the letters on tissue boxes and other objects in the clinic.
At times, anxiety about one’s ability to perform examination techniques and spot critical findings can unearth deeper concerns among trainees about their own visual capabilities. Residents may struggle to behold the eye when they begin training, but their vision is presumed to be normal, at least according to the tests of visual function that ophthalmologists perform on patients. In fact, many residency programmes require applicants to submit documentation of normal vision to even be considered for entry. The most important measures are visual acuity (when best corrected by glasses or contact lenses), colour vision, and depth perception. Occasionally, applicants have been surprised by teaching staff conducting impromptu tests of their vision in the middle of interviews. Although the ethics and legality of enforcing these standards are matters of active debate among ophthalmology teaching staff and residents, residency applicants are nonetheless discouraged from disclosing visual limitations or serious eye disease when applying to training programmes (Blomquist 2014; Vislisel 2015).
My hybrid positioning as an anthropologist and aspiring ophthalmologist influenced my own affective encounters with the ophthalmic examination during my fieldwork. Take, for instance, the moment of panic I experienced after observing a resident evaluate the depth perception of a patient with strabismus, or misalignment of the eyes. As I watched the patient struggle to perceive test images, I started to wonder about my own depth perception. Had it been tested before, perhaps during an eye examination in the distant past? Although I had no reason to suspect my depth perception to be deficient, the idea of having an unrecognised visual deficit gnawed at me for hours before I asked one of the residents to administer a formal test. Much to my relief, my depth perception was pronounced perfectly intact.
Wondrous sights
Many ophthalmologists explain that the aesthetic qualities of the eye contribute to their enjoyment of the specialty. When I asked residents to name aspects of the eye that they found aesthetically pleasing, the iris was frequently called ‘beautiful’ for its intricate texture and the mixture of hues that one can discern upon close inspection. One resident explained that she found the iris beautiful because many of its subtle details go unnoticed by others:
There are definitely structures in the eye that I like—that I think are just more beautiful than the others. I really like the iris, like the folds, the crypts. You look across the room and you say someone’s eyes are brown, or someone’s eyes are blue, and that’s pretty much all you can see. And then you bring them behind the slit lamp with a good amount of magnification, and you can see it’s not a flat sheet. It has all these strands, there’s sometimes little hyperpigmentation spots. It’s all very unique, and it’s a much more complicated structure than you realise from afar—which is kinda awesome because without a slit lamp, nobody knows! Nobody knows except for you!
In this case, the beauty of the iris is compounded by the feeling that one has special access to it. As with many other ophthalmic structures, the act of glimpsing what is otherwise hidden makes the eye even more wondrous.
Certain pathological findings were also described as beautiful, particularly those that involve delicate and complicated structures. A few residents mentioned the so-called ‘sea fan sign’, or an abnormal growth of retinal blood vessels that resembles a variety of coral of the same name. The ‘sea fan sign’ is one of several evocative descriptors used in ophthalmology along with ‘snail tracks’, ‘bear tracks’, ‘horseshoe tear’, and—my personal favourite—‘asteroid hyalosis’. Much of this naming has been a straightforward process of recognising resemblance. There is, however, a certain whimsy at work when pathological findings are likened to corals swaying in the ocean currents, or snails crawling across the retina, or asteroids floating through space. For the ophthalmologists using these descriptors, who may know little about their origins, the terms retain a fanciful quality. As one resident explained to me, ‘It’s just kinda incredible that it looks exactly like a real sea fan … it’s fun that the body is mimicking natural things.’
While the aesthetics of the ‘sea fan sign’ and similar descriptors might best be described as a minor, playful enchantment of ordinary clinical practice, other encounters with the eye give rise to more profound and transformative states of awe. In my own exposure to ophthalmology as a medical student, the wonder I experienced when first seeing the retina with the binocular indirect ophthalmoscope helped crystalise my interest in the specialty. As the patient’s retina came into view, I felt engulfed by its red and orange hues, as if I were diving into the patient’s eye. The experience was reminiscent of an anecdote from the early days of ophthalmoscopy in the mid-nineteenth century where an ophthalmologist was reportedly so excited to see the optic nerve in a living patient (as opposed to a dissected specimen) that he threw the instrument into the air (Ravin 2017).
Residents also take pleasure in the puzzle-solving aspects of diagnosis—or ‘sleuthing’, as one resident put it to me. They are particularly satisfied when their conjectures about a diagnosis from the patient history portion of the encounter are confirmed upon making a visual inspection of the eye with the slit lamp microscope or ophthalmoscope:
I got a patient the other day who was saying that she just saw all these ‘spider webs’ in front of her. So, I thought to myself, ‘you have vitreous haemorrhage—no joke, for sure’. We did the examination, looked inside [the eye], and sure enough there’s blood. I almost want to tell [patients] before I even look in their eye, but I don’t say anything until after, just because I want to confirm … when you confirm what you think things are, I think that’s what all of us want in medicine.
In another instance, a resident noted a faint but unusual pattern of streaks on the surface of a patient’s cornea. He asked the patient whether she took amiodarone and grinned with a sense of achievement when she confirmed that she did, as this is a classic association that ophthalmology residents are taught. The satisfaction he felt by inferring the use of this medication solely from the appearance of the patient’s eye was obvious.
Similar satisfaction arises when residents happen to find ‘textbook’ presentations of diseases in their patients. One resident, recalling a large retinal detachment that he diagnosed in the emergency room, said he had found the sight especially wondrous because it conformed to classic rules that describe how detachments evolve from small tears in the retina. Here the resident’s sense of wonder rests not in the retinal detachment itself, but in the correspondence between the patient’s presentation and the knowledge codified in textbooks. For professionals who spend years poring over textbooks, hoping all the while that their contents will one day be relevant, these correspondences are understandably cause for enjoyment.
Expertise and recognition
The relationship between the professional authority of ophthalmologists and their practices of beholding the eye has a long history. Accounts tend to frame the nineteenth century as a transformative period for ophthalmology in Europe and North America, during which the profession became increasingly specialised and institutionalised. In the United States, the establishment of dedicated eye infirmaries created opportunities for ophthalmologists to differentiate themselves from general surgeons and other groups who treated ophthalmic complaints (Rosen 1972; Brownlee 2008; Ludmerer 2015). Against this backdrop, the introduction of the ophthalmoscope created even more opportunities for ophthalmologists to solidify their position as eye experts. Although some expressed scepticism about the new device, claiming the ophthalmoscope was a tool best suited for inexperienced examiners and for those with poor eyesight, most valued it as a way to expand ophthalmological practice and assert the emerging specialty’s authority (Hubbell 1908; Rosen 1972; Stevens 1998).
For residents, there is a distinct satisfaction and pleasure immanent within the possibility of being an expert and having that expertise recognised. Some residents explained to me that part of ophthalmology’s allure as a career was that it is an intensely specialised field. All medical students learn to auscultate heart sounds with a stethoscope; although not every physician learns to perform this examination technique with the same astuteness as a cardiologist, the basic skill is essentially universal. Ophthalmology, by contrast, is a field that is largely inaccessible to physicians in other specialties. As one resident recounted to me, reflecting on times in medical school that he witnessed ophthalmologists carry out consultations on inpatients: ‘[they] had power … they went in, nobody knew what was going on, and they came out with an answer. You trust them because they’re the ophthalmologists’.
When I accompanied residents on inpatient consultations, it became clear that their ability to provide insight that no other clinicians in the hospital could offer was a point of pride. One instance illustrates the special authority that ophthalmology residents, still very much trainees, wield when interacting with other specialties. I reconstruct the event from my field notes:
A first-year resident and I are called to examine a patient in the emergency room who is experiencing headaches and vision changes. The resident tells me the emergency room team suspects this may be a case of idiopathic intracranial hypertension (IIH), also known as pseudotumor cerebri. Indeed, certain features of the patient’s presentation fit the expected picture for IIH. The most striking of these was a finding on the patient’s CT scan, taken that day, which revealed an abnormality known as ‘empty sella’ that is strongly associated with IIH.
The resident examines the patient. She says to me: ‘I actually don’t think this is IIH; the [left optic] disc looks more inflamed than swollen, and there are diffuse yellow exudates. I wonder whether this is a neuroretinitis or subacute meningitis’.
We are met by the emergency room physician as we walk out of the examination room. He is leaning more towards IIH because of the CT scan findings, and he reasons that our patient would appear much sicker if this were indeed meningitis. In a friendly yet decisive tone, the resident settles the debate: ‘Her retina does not look like IIH.’ The emergency room physician acquiesces: ‘Gotcha’, he says, without missing a beat.
A few minutes later the resident calls the neuro-ophthalmology fellow to seek confirmation of her reasoning on this case. Sure enough, when supplied with the details of the case, the fellow wonders whether this is ‘actually subacute meningitis instead of IIH’. The resident and I exchange knowing glances.
In this episode, the resident’s performance as a visual expert—underscored by the confident assertion of her diagnostic conclusions—is instrumental in affirming her authority.
Another dimension of an ophthalmology resident’s burgeoning visual expertise is bodily comportment during the ophthalmic examination. As an ethnographic observer standing at the teaching scope, I myself often felt the difference between an inexperienced and seasoned examiner. When the slit lamp was used by a senior resident or an attending ophthalmologist, the sequence of movements was predictable and smooth; with the teaching scope right in front of my face, I could anticipate the examiner’s movements and follow them with ease. When the slit lamp was operated by a beginner resident, however, who had yet to embody the smooth, methodical sequence of where and how to look, the apparatus would jerk erratically, and I was more likely to have the teaching scope shoved into my glasses. Once I started my own ophthalmology training, I felt myself under the scrutiny of supervising ophthalmologists and patients alike as I manoeuvred the slit lamp to perform examinations. Worried that fumbling with dials and other parts of the apparatus would betray my inexperience, I often found myself paying special attention to the speed and efficiency of my movement at the slit lamp.
Conclusion
As echoed by decades of ethnographic scholarship on therapeutic apprenticeship, training in the health professions involves more than the transmission of knowledge and skills. It is, rather, a complex process where explicitly recognised forms of learning occur in tandem with more tacit calibration of the trainee’s identity, ethics, attentions, embodied dispositions, and affects (Bosk 1979; Hahn and Kleinman 1983; Konner 1988; Saunders 2008; Wendland 2010; Holmes et al. 2011; Prentice 2012; Merton et al. 2013). Studies of therapeutic apprenticeship provide useful insight into the subjectivities and everyday labour of health professionals. In so doing, they complement broader ethnographic projects that explore the social fabric of healthcare systems.
One intended contribution of studying ophthalmology is to investigate an area of clinical practice that has received relatively little attention in medical anthropology, science studies, and related literature (Stevens et al. 2007; Varpio et al. 2007; Webb et al. 2013; Coopmans and Button 2014). The diagnostic techniques that I describe here may be specialised, but they are also ubiquitous, given that they are performed in essentially all routine eye examinations. Additionally, this article supplements existing literature on embodiment in biomedical training that is geared toward the explicitly ‘manual’ fields of surgery and anatomy (Cassell 1991; Hirschauer 1991; Lawrence 1998; Moreira 2004; Prentice 2012; Fountain 2014). Although ophthalmology is a surgical specialty, slit lamp biomicroscopy and binocular indirect ophthalmoscopy are performed in the clinic by ophthalmologists and optometrists alike.
Although I conducted fieldwork on ophthalmology years before undertaking my own training in the specialty, the account I provide now is inextricable from my identity and experiences as an ophthalmologist. I have leveraged this hybrid background to provide first-hand description of ophthalmology training, revisiting my field notes and other research materials with the updated perspective of a practitioner. As such, the narratives I offer about early stages of ophthalmology residency reflect a combination of analysis and reminiscence. This stance bears resemblance to the work of other physician-anthropologists who bring their training and experiences as healthcare workers to bear on their ethnographic research (see Wendland 2019), in addition to other clinician-anthropologists whose projects examine fields in which they practice (Smith 2017; Weiner 2019).
A practical intervention of this project is to illustrate new avenues for medical educators by which to conceptualise the embodied discipline of clinical training and the frequently powerful affective states that trainees experience as they navigate their formation as health professionals. One field where these frameworks may be of interest is the ‘medical humanities’, a movement among health professions educators with wide-ranging disciplinary orientations and objectives that tends to describe its mission as the promotion of empathy, professionalism, and ethical reasoning in medical education (Shapiro et al. 2009; Ousager and Johannessen 2010). Within the medical humanities, calls have been made to articulate clearer objectives and build more productively on academic disciplines such as history, anthropology, philosophy, literary studies, and art history (Campo 2005). For instance, Greene and Jones (2017) encourage careful review of the contributions that wider disciplines can make to the medical humanities, describing how the history of medicine, in particular, teaches students to locate themselves within historical legacies and to recognise the contingency of disease categories, medical knowledge, and healthcare systems. Polianski and Fangerau (2012) argue that the medical humanities should teach students how to think reflexively about the sociocultural embeddedness of clinical practice, rather than harnessing the arts as a tool for inculcating moral sensibilities.
In accord with these critiques that suggest a need to reimagine the goals of the medical humanities, ethnography, too, has a great deal to offer. Although the accounts of ‘culture’ that most medical students recognise originate outside anthropology—such as Fadiman’s (1998) widely read tale about the collision of two cultures during a Hmong family’s interactions with biomedical institutions in California—recent attempts to bring anthropology into medical education have shifted away from narratives about cultural difference and exhortations to practice ‘cultural competency’. Metzl and Hansen (2014), for instance, have developed a model they term ‘structural competency’, where students are taught to recognise the socioeconomic and political conditions that undergird and constrain healthcare systems.
Reading ethnographies of medical education can provide trainees with deeper understanding of their own transformation into health professionals. The goal here is not to train clinicians in ethnographic methods, but to foster an ethnographic disposition where clinicians are equipped to connect their first-hand experiences to broader analytical frameworks. As opposed to writing poetry and reflective essays—which many in medicine find satisfying as forms of creative expression and introspection—ethnography holds value as a technique for identifying subtle aspects of everyday life and situating the particularities of experience within historical, ideological, and political economic contexts that transcend the individual. Clinicians are ready for these new modes of self-inspection and contextualisation that can take shape through engagement with ethnography.
Acknowledgements
I am indebted to the many ophthalmology residents and teaching staff who graciously participated in this research. Financial support during my fieldwork and dissertation writing was provided by the Morris Fishbein Center for the History of Science and Medicine at the University of Chicago. Thanks are also due to my colleagues and mentors who provided invaluable guidance, criticism, and camaraderie throughout my training. My thanks, finally, to David Ansari and Amy Cooper, who have diligently curated this special issue on therapeutic apprenticeship.
About the author
Adam D. Baim is a senior ophthalmology resident at Washington University in St. Louis, Missouri. He is a graduate of the MD/PhD programme in Medicine, the Social Sciences, and Humanities (MeSH) at the University of Chicago, where his training focused on the anthropology of biomedicine.
Footnotes
Ophthalmologists in the United States and most other nations are medical doctors who have completed postgraduate training in an ophthalmology residency programme after being awarded a Doctor of Medicine or equivalent degree. They diagnose and treat diseases of the eye, eyelids, and eye socket as well as disorders of eye movement and neurologic issues that affect the transmission or processing of visual information in the brain. Ophthalmologists are distinct from optometrists, who attend four-year graduate programmes and hold instead a Doctor of Optometry degree. Optometrists are licensed to measure vision and prescribe corrective eyewear along with eye drops and certain oral medications. Although ophthalmologists and optometrists often work together, the latter are not trained or licensed to perform surgery in most jurisdictions. Procedures such as cataract extraction, refractive surgery (e.g., ‘LASIK’), retinal detachment repair, and corneal transplant are performed exclusively by ophthalmologists.↩︎
Much of my fieldwork was conducted in 2016 at an ophthalmology residency programme in a major North American city, under the auspices of an Institutional Review Board protocol whose terms preclude me from publishing the name of the institution that graciously hosted me. My experiences as a medical student and ophthalmology resident inform this article only as autoethnographic reflections about my own training and are not associated with any particular institution or individual.↩︎
Of note are two studies by Coopmans, Graham, and Hamzah (2012) and Coopmans and Button (2014) which explore the interpretation of retinal photographs with emphasis on standardised techniques for grading diabetes-related retinal disease. In the earlier study, the authors discuss a clinical trial that investigated the use of retinal photography as a screening test for eye disease. The later article is a study of image interpreters who come not only from ophthalmology, but other fields such as family medicine. The authors briefly discuss the embodied practice of interpreters as they navigate through retinal photographs on computer monitors and annotate these images with their interpretations. Other studies of eye care professionals include Stevens et al. (2007), Varpio et al. (2007), and Webb et al. (2013).↩︎
As Daston and Galison (2007) argue, objectivity itself is a malleable category that can assume varied forms depending on differences in scientific practice and the ‘epistemic virtues’ of scientists.↩︎
As Lock and Farquhar (2007) observe, phenomenology has important shortcomings when applied in ethnographic research. These include an emphasis on the individual subject that obscures the social contingency of embodiment and subjectivity, as well as a tendency to presume an idealised, universal subject that transcends history and culture.↩︎
References
Adorno, Theodor W. 1997. Aesthetic Theory. Translated by Robert Hullot-Kentor. Minneapolis, MN: University of Minnesota Press.
Benjamin, Walter. 1968. Illuminations. New York, NY: Harcourt.
Blomquist, Preston H. 2014. ‛Is It Time to Adopt Vision Screening for Ophthalmology Residency Program Applicants?’ Journal of Academic Ophthalmology 07 (01): e001–e002. https://doi.org/10.1055/s-0034-1396086.
Boas, Franz. 1889. ‛On Alternating Sounds’. American Anthropologist 2 (1): 47–54. https://doi.org/10.1525/aa.1889.2.1.02a00040.
Bosk, Charles L. 1979. Forgive and Remember: Managing Medical Failure. Chicago, IL: University of Chicago Press.
Bourdieu, Pierre. 1977. Outline of a Theory of Practice. Cambridge, UK: Cambridge University Press.
Brownlee, Peter J. 2008. ‛Ophthalmology, Popular Physiology, and the Market Revolution in Vision, 1800–1850’. Journal of the Early Republic 28 (4): 597–626. https://doi.org/10.1353/jer.0.0040.
Burri, Regula Valérie. 2013. ‛Visual Power in Action: Digital Images and the Shaping of Medical Practices’. Science as Culture 22 (3): 367–87. https://doi.org/10.1080/09505431.2013.768223.
Burri, Regula Valérie, and Joseph Dumit. 2008. ‛Social Studies of Scientific Imaging and Visualization’. In The Handbook of Science and Technology Studies, edited by Edward J. Hackett, 297–317. Cambridge, MA: MIT Press.
Campo, Rafael. 2005. ‛A Piece of My Mind. ‟The Medical Humanities,” for Lack of a Better Term’. JAMA 294 (9): 1009–11. https://doi.org/10.1001/jama.294.9.1009.
Cassell, Joan. 1991. Expected Miracles: Surgeons at Work. Philadelphia, PA: Temple University Press.
Coopmans, Catelijne, and Graham Button. 2014. ‛Eyeballing Expertise’. Social Studies of Science 44 (5): 758–85. https://doi.org/10.1177/0306312714531472.
Coopmans, Catelijne, Connor Graham, and Haslina Hamzah. 2012. ‛The Lab, the Clinic, and the Image: Working on Translational Research in Singapore’s Eye Care Realm’. Science, Technology and Society 17 (1): 57–77. https://doi.org/10.1177/097172181101700104.
Crary, Jonathan. 1990. Techniques of the Observer: On Vision and Modernity in the Nineteenth Century. Cambridge, MA: MIT Press.
Daston, Lorraine, and Peter Galison. 2007. Objectivity. New York, NY: Zone Books.
Dumit, Joseph. 2004. Picturing Personhood: Brain Scans and Biomedical Identity. Princeton, NJ: Princeton University Press.
Fadiman, Anne. 1998. The Spirit Catches You and You Fall Down: A Hmong Child, Her American Doctors, and the Collision of Two Cultures. New York, NY: Farrar, Straus and Giroux.
Foster, Hal, ed. 1988. Vision and Visuality. Seattle, WA: Bay Press.
Foucault, Michel. 1980. ‛The Eye of Power’. In Power/Knowledge: Selected Interviews and Other Writings, 1972–1977, edited by Colin Gordon, 146–65. New York, NY: Pantheon Books.
Fountain, T. Kenny. 2014. Rhetoric in the Flesh: Trained Vision, Technical Expertise, and the Gross Anatomy Lab. New York, NY: Taylor & Francis.
Frank, Jason R., Linda. S. Snell, Olle Ten Cate, Eric. S. Holmboe, Carol Carraccio, Susan R. Swing, Peter Harris, Nicholas J. Glasgow, Craig Campbell, Deepak Dath et al. 2010. ‛Competency-Based Medical Education: Theory to Practice’. Medical Teacher 32 (8): 638–45. https://doi.org/10.3109/0142159x.2010.501190.
Goodwin, Charles. 1994. ‛Professional Vision’. American Anthropologist 96 (3): 606–33. https://doi.org/10.1525/aa.1994.96.3.02a00100.
Greene, Jeremy A., and David S. Jones. 2017. ‛The Shared Goals and Distinct Strengths of the Medical Humanities: Can the Sum of the Parts Be Greater Than the Whole?’ Academic Medicine 92 (12): 1661–64. https://doi.org/10.1097/ACM.0000000000001991.
Hahn, Robert A., and Arthur Kleinman. 1983. ‛Biomedical Practice and Anthropological Theory: Frameworks and Directions’. Annual Review of Anthropology 12 (1): 305–33. https://doi.org/10.1146/annurev.an.12.100183.001513.
Hammer, Gili. 2018. ‛‟You Can Learn Merely by Listening to the Way a Patient Walks through the Door”: The Transmission of Sensory Medical Knowledge’. Medical Anthropology Quarterly 32 (1): 138–54. https://doi.org/10.1111/maq.12366.
Haraway, Donna. 1988. ‛Situated Knowledges: The Science Question in Feminism and the Privilege of Partial Perspective’. Feminist Studies 14 (3): 575–99. https://doi.org/10.2307/3178066.
Heidegger, Martin. 1977. ‛The Age of the World Picture’. In The Question Concerning Technology, and Other Essays, 115–54. New York, NY: Garland.
Hirschauer, Stefan. 1991. ‛The Manufacture of Bodies in Surgery’. Social Studies of Science 21 (2): 279–319. https://doi.org/10.1177/030631291021002005.
Holmes, Seth M., Angela C. Jenks, and Scott Stonington. 2011. ‛Clinical Subjectivation: Anthropologies of Contemporary Biomedical Training’. Culture, Medicine, and Psychiatry 35 (2): 105–12. https://doi.org/10.1007/s11013-011-9207-1.
Hubbell, Alvin Allace. 1908. The Development of Ophthalmology in America, 1800 to 1870: A Contribution to Ophthalmologic History and Biography; an Address Delivered in Abstract Before the Section of Opthalmology of the American Medical Association, June 4, 1907. Chicago, IL: W.T. Keener & Co.
Jasanoff, Sheila. 1998. ‛The Eye of Everyman: Witnessing DNA in the Simpson Trial’. Social Studies of Science 28 (5–6): 713–40. https://doi.org/10.1177/030631298028005003.
Jay, Martin. 1993. Downcast Eyes: The Denigration of Vision in Twentieth-Century French Thought. Berkeley, CA: University of California Press.
Joyce, Kelly. 2010. ‛The Body as Image: An Examination of the Economic and Political Dynamics of Magnetic Resonance Imaging and the Construction of Difference’. In Biomedicalization: Technoscience, Health, and Illness in the U.S., edited by Adele E. Clarke, Laura Mamo, Jennifer Ruth Fosket, Jennifer R. Fishman, and Janet K. Shim, 197–217. Durham, NC: Duke University Press. https://doi.org/10.1215/9780822391258-007.
Jütte, Robert, and James Lynn. 2005. A History of the Senses: From Antiquity to Cyberspace. Cambridge, UK: Polity.
Kant, Immanuel. (1790) 2000. Critique of the Power of Judgment. Edited by P. Guyer. Translated by M. Guyer and E. Matthews. Cambridge, UK: Cambridge University Press.
Knorr-Cetina, Karin, and Klaus Amann. 1990. ‛Image Dissection in Natural Scientific Inquiry’. Science, Technology, & Human Values 15 (3): 259–83. https://doi.org/10.1177/016224399001500301.
Konner, Melvin. 1988. Becoming a Doctor: A Journey of Initiation in Medical School. New York, NY: Penguin Books.
Lawrence, Christopher. 1998. ‛Medical Minds, Surgical Bodies’. In Science Incarnate: Historical Embodiments of Natural Knowledge, edited by Christopher Lawrence and Steven Shapin, 156–201. Chicago, IL: University of Chicago Press.
Leys, Ruth. 2011. ‛The Turn to Affect: A Critique’. Critical Inquiry 37 (3): 434–72. https://doi.org/10.1086/659353.
Lock, Margaret, and Judith Farquhar. 2007. Beyond the Body Proper: Reading the Anthropology of Material Life. Durham, NC: Duke University Press.
Ludmerer, Kenneth M. 2015. Let Me Heal: The Opportunity to Preserve Excellence in American Medicine. Oxford, UK: Oxford University Press.
Lynch, Michael. 1990. ‛The Externalized Retina: Selection and Mathematization in the Visual Documentation of Objects in the Life Sciences’. In Representation in Scientific Practice, edited by Michael Lynch and Steve Woolgar, 153–86. Cambridge, MA: MIT Press.
Mahmood, Saba. 2005. Politics of Piety: The Islamic Revival and the Feminist Subject. Princeton, NJ: Princeton University Press.
Martin, Emily. 2013. ‛The Potentiality of Ethnography and the Limits of Affect Theory’. Current Anthropology 54 (S7): S149–58. https://doi.org/10.1086/670388.
Masco, Joseph. 2004. ‛Nuclear Technoaesthetics: Sensory Politics from Trinity to the Virtual Bomb in Los Alamos’. American Ethnologist 31 (3): 349–73. https://doi.org/10.1525/ae.2004.31.3.349.
Massumi, Brian. 2002. Parables for the Virtual: Movement, Affect, Sensation, Post-Contemporary Interventions. Durham, NC: Duke University Press.
Mauss, Marcel. 2007. ‛Techniques of the Body’. In Beyond the Body Proper: Reading the Anthropology of Material Life, edited by Margaret Lock and Judith Farquhar, 70–88. Durham, NC: Duke University Press.
Mazzarella, William. 2009. ‛Affect: What Is It Good For?’ In Enchantments of Modernity: Empire, Nation, Globalization, edited by Saurabh Dube, 291–309. New York, NY: Routledge, Taylor & Francis Group.
Merleau-Ponty, Maurice. 2002. Phenomenology of Perception. Translated by Colin Smith. London, UK: Routledge.
Merton, Robert K., George G. Reader, and Patricia Kendall, eds. (1957) 2013. The Student-Physician: Introductory Studies in the Sociology of Medical Education. Reprint, Cambridge, MA: Harvard University Press.
Metzl, Jonathan M., and Helena Hansen. 2014. ‛Structural Competency: Theorizing a New Medical Engagement with Stigma and Inequality’. Social Science & Medicine 103 (0): 126–33. https://doi.org/10.1016/j.socscimed.2013.06.032.
Mol, Annemarie. 2002. The Body Multiple: Ontology in Medical Practice. Durham, NC: Duke University Press.
Moreira, Tiago. 2004. ‛Coordination and Embodiment in the Operating Room’. Body & Society 10 (1): 109–29. https://doi.org/10.1177/1357034x04042169.
Myers, Natasha. 2015. Rendering Life Molecular: Models, Modelers, and Excitable Matter. Durham, NC: Duke University Press.
Nazari Khanamiri, Hossein, Austin Nakatsuka, and Jaafar El-Annan. 2017. ‛Smartphone Fundus Photography’. JoVE (125): e55958. https://doi.org/doi:10.3791/55958.
Ousager, Jakob, and Helle Johannessen. 2010. ‛Humanities in Undergraduate Medical Education: A Literature Review’. Academic Medicine 85 (6): 988–98. https://doi.org/10.1097/ACM.0b013e3181dd226b.
Polianski, Igor J., and Heiner Fangerau. 2012. ‛Toward ‟Harder” Medical Humanities: Moving Beyond the ‟Two Cultures” Dichotomy’. Academic Medicine 87 (1): 121–26. https://doi.org/10.1097/ACM.0b013e31823ad204.
Prentice, Rachel. 2012. Bodies in Formation: An Ethnography of Anatomy and Surgery Education. Durham, NC: Duke University Press.
Ravin, James. G. 2017. ‛Hermann Von Helmholtz: The Power of Ophthalmoscopy’. In Foundations of Ophthalmology: Great Insights That Established the Discipline, edited by M.F. Marmor and D.M. Albert, 85–93. Cham, Switzerland: Springer International Publishing.
Rice, Tom. 2013. Hearing and the Hospital: Sound, Listening, Knowledge and Experience. Canon Pyon, UK: Sean Kingston Publishing.
Rosen, George. (1944) 1972. The Specialization of Medicine with Particular Reference to Ophthalmology. New York, NY: Froben Press. Reprint, New York, NY: Arno Press. Citations refer to the Arno edition.
Saunders, Barry F. 2008. CT Suite: The Work of Diagnosis in the Age of Noninvasive Cutting. Durham, NC: Duke University Press.
Schiller, Friedrich. (1795) 2004. On the Aesthetic Education of Man. Translated by R. Snell. Mineola, NY: Dover Publications.
Shapiro, Johanna, Jack Coulehan, Delese Wear, and Martha Montello. 2009. ‛Medical Humanities and Their Discontents: Definitions, Critiques, and Implications’. Academic Medicine 84 (2): 192–98. https://doi.org/10.1097/ACM.0b013e3181938bca.
Simon, Christian M. 1999. ‛Images and Image: Technology and the Social Politics of Revealing Disorder in a North American Hospital’. Medical Anthropology Quarterly 13 (2): 141–62. https://doi.org/10.1525/maq.1999.13.2.141.
Smith, Yvonne. 2017. ‛“Sense” and Sensitivity: Informal Apprenticeship among Youth Care Workers in a Residential Treatment Center for Children’. Child & Family Social Work 22 (3): 1330–37. https://doi.org/https://doi.org/10.1111/cfs.12350.
Stevens, Fred C. J., Joseph P. M. Diederiks, Fieke Grit, and Frans van der Horst. 2007. ‛Exclusive, Idiosyncratic and Collective Expertise in the Interprofessional Arena: The Case of Optometry and Eye Care in the Netherlands’. Sociology of Health & Illness 29 (4): 481–96. https://doi.org/10.1111/j.1467-9566.2007.01001.x.
Stevens, Rosemary. 1998. American Medicine and the Public Interest. Berkeley, CA: University of California Press.
Varpio, Lara, Marlee M. Spafford, Catherine F. Schryer, and Lorelei Lingard. 2007. ‛Seeing and Listening: a Visual and Social Analysis of Optometric Record-Keeping Practices’. Journal of Business and Technical Communication 21 (4): 343–75. https://doi.org/10.1177/1050651907303991.
Vertesi, Janet. 2015. Seeing Like a Rover: How Robots, Teams, and Images Craft Knowledge of Mars. Chicago, IL: University of Chicago Press.
Vislisel, Jesse. 2015. The Iowa Guide to the Ophthalmology
Match. University of Iowa. https://www.EyeRounds.org/
tutorials/Iowa-Guide-to-the-Ophthalmology-Match/.
Webb, Helena, Christian Heath, Dirk vom Lehn, and William Gibson. 2013. ‛Engendering Response: Professional Gesture and the Assessment of Eyesight in Optometry Consultations’. Symbolic Interaction 36 (2): 137–58. https://doi.org/10.1002/symb.55.
Weiner, Talia R. 2019. ‛Billable Services and the “Therapeutic Fee”: On the Work of Disavowal of Political Economy and its Re-Emergence in Clinical Practice’. Anthropological Quarterly 92 (3): 697–728. https://doi.org/10.1353/anq.2019.0055.
Wendland, Claire L. 2010. A Heart for the Work: Journeys through an African Medical School. Chicago, IL: University of Chicago Press.
Wendland, Claire L. 2019. ‛Physician Anthropologists’. In Annual Review of Anthropology, Volume 48, edited by D. Brenneis and K. B. Strier, 187–205. Palo Alto, CA: Annual Reviews. https://doi.org/10.1146/annurev-anthro-102218-011338.