Qualitative cancer research
Taking stock, stepping further
—
Introduction
On 28–29 April 2014, the Qualitative Research Group on Cancer, based at the Berlin School of Public Health, Charité – Universitätsmedizin, in Berlin, Germany, hosted a two-day conference to review current perspectives in qualitative cancer research.[note 1] Such research has become a major focus of qualitative health research in recent decades, both challenging and supplementing studies grounded in the epistemology of biomedical sciences. Qualitative cancer research is committed to investigating various actors’ perspectives on and the implications of contexts, (power) relations, and processes related to a cancer diagnosis, and cancer prevention, treatment, and the experience thereof.
The conference provided a rare opportunity to bring together a diverse group of researchers and clinicians engaging in qualitative cancer research from twelve countries, various career stages, and multiple disciplines, including biomedicine, social sciences, and public health. The conference included fifteen individual presentations grouped into five thematic sessions (see the list of presentations at the end of this report).
Taking stock: Introduction and keynote
Welcoming participants, Christine Holmberg opened the conference by suggesting that a central question for the conference should be: ‘What is cancer?’ Such a question concerns the epistemological underpinnings of cancer research and bridges the gap between different methodological approaches by focusing on deciphering the topic and its underlying power relations and assumptions. Arguing that the construct of cancer has many meanings, Holmberg proposed that cancer has become a defining model of sickness itself. The analysis of what constitutes ‘cancer’ in the research projects presented gives insight into the phenomenon itself and helps illuminate the field of cancer research and its power relations more generally.
In her keynote contribution, Rikke Sand Andersen argued that shifting orientations toward cancer diagnostics, emphasizing early disease detection, should be reflected in the way we frame and position ‘qualitative research’. While early detection of cancer is exemplary of techno-medicine, made possible by biomedical technologies designed to detect early tumor growth and to some extent the identification of biomarkers and genetic markers, current rationales underpinning early disease detection accentuate symptom-based diagnostics and the search for sensorial markers of cancer. According to Andersen, cancer diagnostics – despite their technological alignments – to a large degree rest on human perception, prompting individuals, doctors, and patients alike to decipher and evaluate bodily sensations as part of the diagnostic process. Early disease detection thus exemplifies how particular historical, political, and social contexts may contribute to embodied experiences and the framing of bodily sensations. The qualitative study of cancer diagnostics may generate new contextualized perspectives, in particular the collective framing of bodily sensations and the processes by which they are evoked, legitimized, and mobilized for action.
Session A: Exploring cancer experiences
Chaired by Y. Adam and S. Blakeslee
This panel highlighted experiences of specific patient groups, including young women coping with breast cancer in three European countries (Greco, De Michele, and Hamarat), cancer survivors in Puerto Rico (Dyer), and cancer patients living alone during their treatment (Benoot et al.). In addition to individual health biographies and patients’ coping strategies, the influence of sociality on individual lives was discussed, with the research results bridging the gap between social research and activism (Greco).
Session B: Navigating prevention and treatment
Chaired by S. Blakeslee and W. Stritter
Examining how the shifting landscapes and broader discourses of cancer prevention and treatment are navigated, this panel demonstrated that decisions about prevention and treatment are reached in lived contexts. For older adults in Canada, age and sense of time can become a point of reference, both in terms of the value of time and timing of treatment decisions (Strohschein et al.). Further, Canadian parents’ narratives regarding vaccinating teens for human papilloma viruses (HPV) demonstrated how vaccination decisions are negotiated, both reproducing and struggling against broader gendered and political discourses that inform the practice of HPV vaccination (Polzer).
Session C: Chronic illness and survivorship
Chaired by J. Kennedy and W. Stritter
For a growing number of cancer patients, their illness has evolved from life threatening to a chronic condition. This shift necessitates changes in the structures of biomedical healthcare to properly address the needs of individuals during the unpredictable timespan of living as a cancer survivor. The notion of ‘palliative care’ used in the sense of end-of-life care in France, for example, does not address these changes and thus complicates translating study results from one (national) context to another (Buthion).
Session D: Institutionalising cancer
Chaired by W. Stritter and S. Brandner
This session discussed cancer in relation to different institutionalised settings in the healthcare system and health politics, which frame how and why cooperation between different medical specialists is configured. This was elucidated by an analysis of German practitioners’ views on their interdisciplinary interactions (Chakkalakal). Institutionalised settings also affect how translational researchers define their field of work and influence public opinion (Thonon et al.), likewise demonstrated by the example of public participation in United States Food and Drug Administration oncological drug evaluations (Knaapen).
Sessions E and F: Cancer knowledge under construction
Chaired by D. Chakkalakal, M. Schultze, and J. Kennedy
The production of knowledge about cancer was the focal point of these two panels. First, in a presentation by de Graaf, patients with advanced-stage cancer participating in a clinical trial were studied as shapers of knowledge who actively construct and negotiate a concept of hope in order to cope with uncertainty while facing a bleak diagnosis. Next, the need for diversifying ‘cancer knowledge’ was demonstrated by three presentations. An analysis of HPV vaccination discourses (Molino et al.) and breast cancer awareness campaigns in different countries (Jäger and Bouskill) demonstrated how heteronormatively gendered images, language, and calls for personal behavior changes currently shape cancer knowledge. These showed that the authoritative knowledge of biomedicine and the unwarranted overemphasis on controlling risk for cancer results in unnecessary feelings of guilt among those with cancer.
The co-construction of ‘culturally appropriate’ knowledge about cancer care was shown by involving the experiences of lesbian, bisexual, transgender, and queer patients with breast or gynaecological cancer in the process of cancer knowledge production (Rail et al.). Seo presented how medical professionals and journalists in South Korea shape cancer discourses using neologisms that transport cultural values, thus shaping and influencing public discourse and individual treatment decisions. In the last presentation of the conference, Blakeslee looked at decision making in the context of breast cancer risk in the United States and examined how women who are diagnosed as being at risk for breast cancer begin to discuss themselves in quantitative terms.
Discussion
Chaired by Y. Adam, S. Blakeslee, and S. Brandner
In a lively final discussion, the conference concluded with an overall mapping and positioning of qualitative cancer research within the field of (biomedical) cancer research, methodological debates, and the potential positions of qualitative cancer researchers. In an environment dominated by quantitative methods and evidence-based medicine, the reality of conducting qualitative research was considered both a limitation and a resource. In this context, it was suggested that it would be fruitful to shift the quantitative–qualitative debate away from a discussion of methods to the different epistemological and ontological presumptions underlying both approaches. Researchers in the field of qualitative cancer research could both contribute to and benefit from such a shift in the debate. The discussion transcended a simple dualism of quantitative vs. qualitative research and tried to grasp the realities of most participants working in or with different disciplines. It was further suggested that binary categories such as ‘theory vs. applied research’ could and should be bridged by our work while still exploring the radical potential of our research. The incongruity of complex knowledge production and applied knowledge production also yielded a rigorous discussion.
Stepping further
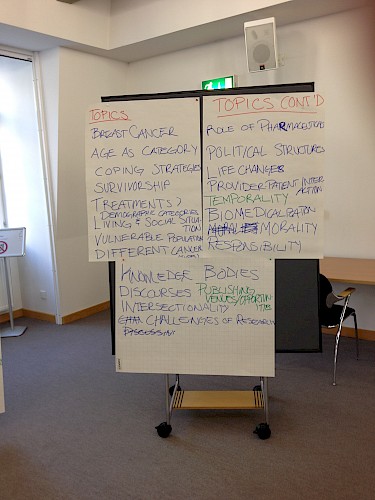
Chaired by D. Chakkalakal, J. Kennedy, M. Schultze, and W. Stritter
The conference participants identified research gaps that they felt had not been exhausted at the conference or are still missing in the field of qualitative cancer research in general, including: perspectives and action strategies of actors (such as the elderly and biomedical professionals), health services research, topics related to complementary medicine or the role of the pharmaceutical industry, different epistemological and ontological approaches, aspects of intersectionality, the notion of survivorship and cancer as a chronic condition, cancer and the body, and finally, various challenges of qualitative research in general (political structures, funding issues, dialogue with the medical world, complexity of field contexts, and institutionalized ethical issues). As a springboard into the field of qualitative cancer research, this conference mapped current research while elaborating on topics for future research and collaborative conferences.
Presentations
Adam, Y., S. Blakeslee, and S. Brandner. 2014. Final Discussion (Day One).
Andersen, R. S. 2014. Why Strive for Solidarity in Qualitative Cancer Research? Discussing the Case of ‘Patient Delay’ in Healthcare Seeking.
Benoot, C., R. Deschepper, M. Grypdonck, and J. Bilsen. 2014. ‘Staying Independent’: A Qualitative Study to Explore the Experiences of Cancer Patients Living Alone During Their Treatment.
Blakeslee, S. 2014. Reflections on Risk: Consultation Experience of Women Diagnosed with Breast Cancer Risk.
Buthion, V., N. Moumjid, and J. Margier. 2014. Chronic Cancer Treatment and Healthcare Configurations: A Qualitative Investigation.
Chakkalakal, D. 2014. Complexities, Complications and Competencies: Physicians’ Views on the Interdisciplinary Treatment of Urological Cancer in Germany.
Chakkalakal, D., J. Kennedy, M. Schultze, and W. Stritter. 2014. Final Discussion and Closing of Conference.
De Graaf, S. 2014. Caught between Hopes and Fears: The Construction of Hope in a Cancer Trial.
Dyer, K.E. 2014. Experiencing Life after Cancer in Puerto Rico: Findings from a Qualitative Study on Survivorship.
Greco, C., G. De Michele, and N. Hamarat. 2014. Young Women Coping with Breast Cancer: The Cases of Belgium, France and Italy in a Comparative Perspective.
Holmberg, C. 2014. Introduction: Qualitative Cancer Research.
Jäger, M., and K. Bouskill. 2014. The Illusion of Control in the Global Flow of Breast Cancer Awareness Campaigns.
Knaapen, L. 2014. Public Participation in Oncologic Drug Evaluation.
Molino, L., G. Rail, and C. Fusco. 2014. HPV Vaccination Discourses: Impact on Canadian Girls’ Bodies and Subjectivities.
Polzer, J. 2014. Negotiating Risks and Responsibilities: A Critical Narrative Study of Parents’ Decision-Making about Human Papillomavirus (HPV) Vaccination.
Rail, G., M. Bryson, T. Hart, J. Gahagan, J. Ristock, and L. Molino. 2014. Queering Qualitative Cancer Research: Cancer’s Margins, Knowledge and Subjectivities.
Seo, M. 2014. Inventing Neologisms Regarding Breast Cancer in South Korea.
Strohschein, F.J., R.S. Schreiber, J.L. Bottorff, F. Ducharme, H. Bergman, and C.G. Loiselle. 2014. Coming to Decisions about Cancer Treatment: Understanding the Processes among Older Men and Women with Colorectal Cancer.
Thonon, F., M. Saghatchian, R. Boulkedid, S. Gottot, M. Texeira, and C. Alberti. 2014. A Qualitative Study of the Views of Researchers on the Definitions, Issues and Evaluation of Translational Research in Oncology.